Tuesday Poster Session
Category: Stomach and Spleen
P6377 - From GAVE to Polyps: Is Treatment a Double-Edged Sword?
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Aria Khan, MD (she/her/hers)
NYC Health + Hospitals/Woodhull
Jamaica, NY
Presenting Author(s)
Joanna Lenik, MD1, Aria Khan, MD2, Jennifer Harley, MD1
1NYC Health + Hospitals/Metropolitan, New York, NY; 2NYC Health + Hospitals/Woodhull, Jamaica, NY
Introduction: Gastric Antral Vascular Ectasia (GAVE), or “watermelon stomach,” is a rare but important cause of chronic gastrointestinal bleeding and iron deficiency anemia. While commonly associated with portal hypertension and autoimmune diseases, other contributing factors—such as mechanical stress and metabolic syndrome—have been implicated. Aortic stenosis, through Heyde’s syndrome, is also linked to GAVE. Argon Plasma Coagulation (APC) remains a first-line treatment. We present a unique case of a patient with GAVE who developed numerous hyperplastic gastric polyps after undergoing repeated APC treatments.
Case Description/
Methods: A 66-year-old woman with a history of bariatric surgery and moderate aortic stenosis presented with recurrent iron deficiency anemia and melena. Initial endoscopy revealed gastric and duodenal hyperplastic polyps along with Helicobacter pylori infection. Over time, she developed active GAVE, managed with multiple APC sessions. Despite therapy, bleeding persisted, and the polyps enlarged progressively. Histology confirmed chronic gastritis and hyperplastic changes, with no evidence of dysplasia. Serum gastrin levels remained within normal range, making hypergastrinemia an unlikely cause of polyp growth.
Discussion: This case illustrates an atypical presentation of GAVE in a post-bariatric surgery patient without the common risk factors of portal hypertension or autoimmune disease. Aortic stenosis, possibly through acquired von Willebrand factor deficiency, may underlie the bleeding seen in Heyde’s syndrome. Mechanical stress from altered gastric anatomy and features of metabolic syndrome may also contribute to mucosal injury and GAVE development.
A notable aspect of this case is the emergence of diffuse hyperplastic polyps following repeated APC therapy. Although APC is the standard treatment for GAVE, cumulative mucosal injury from repeated ablation may provoke a regenerative response, resulting in hyperplastic polyp formation. These polyps, though benign, may bleed, obstruct, or rarely undergo malignant transformation. The observed temporal association in this case highlights the importance of awareness regarding this potential complication. Regular endoscopic surveillance and timely management of symptomatic or enlarging polyps are essential to minimize bleeding and long-term risks.
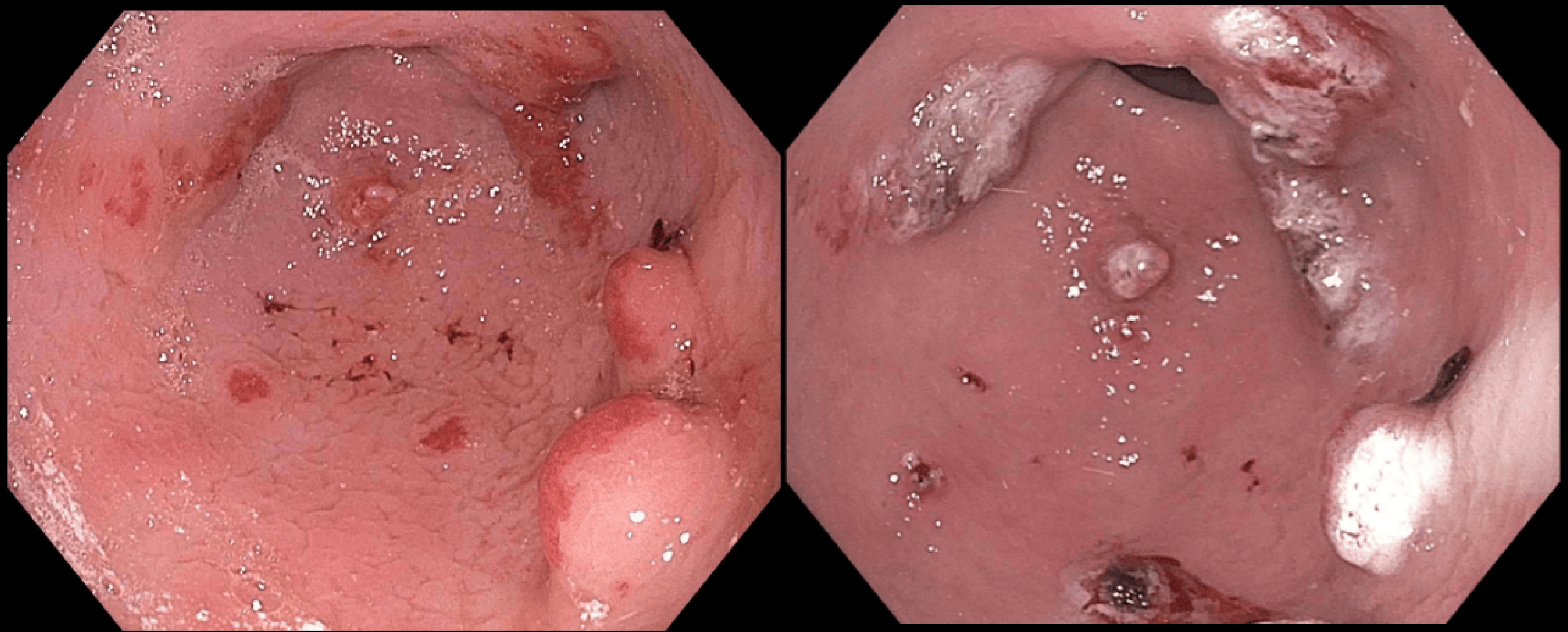
Figure: Left - Gastric Antrum with GAVE and Polyps in 2021, Right - Same region After APC treatment
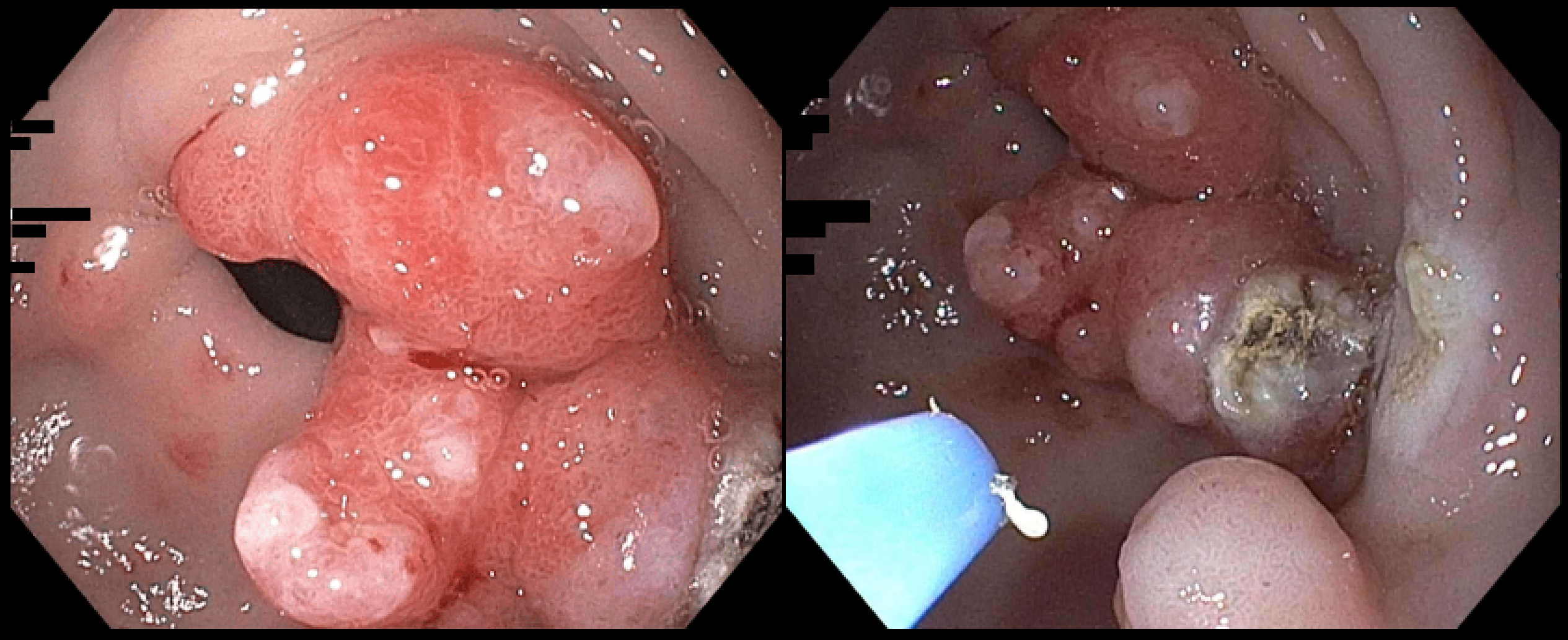
Figure: Left - Gastric Antrum with Antral Mass in 2024, Right - Same region After APC treatment
Disclosures:
Joanna Lenik indicated no relevant financial relationships.
Aria Khan indicated no relevant financial relationships.
Jennifer Harley indicated no relevant financial relationships.
Joanna Lenik, MD1, Aria Khan, MD2, Jennifer Harley, MD1. P6377 - From GAVE to Polyps: Is Treatment a Double-Edged Sword?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYC Health + Hospitals/Metropolitan, New York, NY; 2NYC Health + Hospitals/Woodhull, Jamaica, NY
Introduction: Gastric Antral Vascular Ectasia (GAVE), or “watermelon stomach,” is a rare but important cause of chronic gastrointestinal bleeding and iron deficiency anemia. While commonly associated with portal hypertension and autoimmune diseases, other contributing factors—such as mechanical stress and metabolic syndrome—have been implicated. Aortic stenosis, through Heyde’s syndrome, is also linked to GAVE. Argon Plasma Coagulation (APC) remains a first-line treatment. We present a unique case of a patient with GAVE who developed numerous hyperplastic gastric polyps after undergoing repeated APC treatments.
Case Description/
Methods: A 66-year-old woman with a history of bariatric surgery and moderate aortic stenosis presented with recurrent iron deficiency anemia and melena. Initial endoscopy revealed gastric and duodenal hyperplastic polyps along with Helicobacter pylori infection. Over time, she developed active GAVE, managed with multiple APC sessions. Despite therapy, bleeding persisted, and the polyps enlarged progressively. Histology confirmed chronic gastritis and hyperplastic changes, with no evidence of dysplasia. Serum gastrin levels remained within normal range, making hypergastrinemia an unlikely cause of polyp growth.
Discussion: This case illustrates an atypical presentation of GAVE in a post-bariatric surgery patient without the common risk factors of portal hypertension or autoimmune disease. Aortic stenosis, possibly through acquired von Willebrand factor deficiency, may underlie the bleeding seen in Heyde’s syndrome. Mechanical stress from altered gastric anatomy and features of metabolic syndrome may also contribute to mucosal injury and GAVE development.
A notable aspect of this case is the emergence of diffuse hyperplastic polyps following repeated APC therapy. Although APC is the standard treatment for GAVE, cumulative mucosal injury from repeated ablation may provoke a regenerative response, resulting in hyperplastic polyp formation. These polyps, though benign, may bleed, obstruct, or rarely undergo malignant transformation. The observed temporal association in this case highlights the importance of awareness regarding this potential complication. Regular endoscopic surveillance and timely management of symptomatic or enlarging polyps are essential to minimize bleeding and long-term risks.
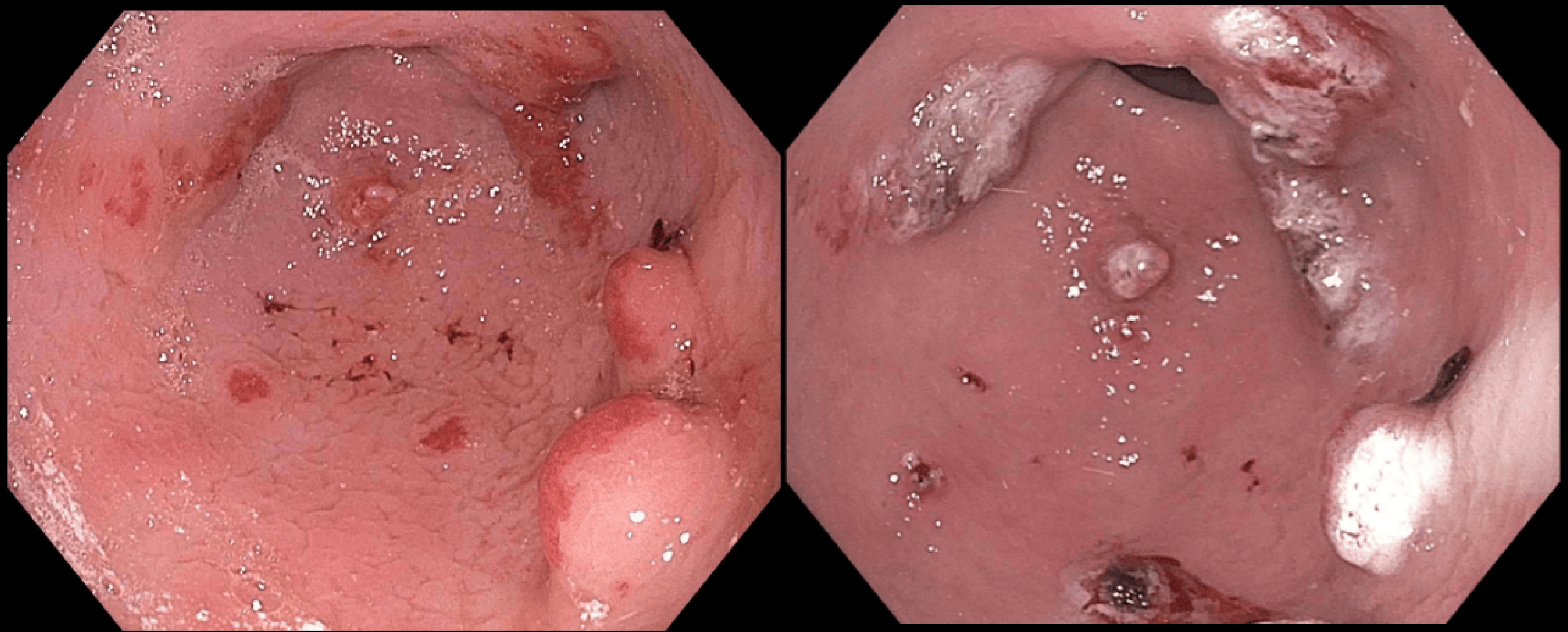
Figure: Left - Gastric Antrum with GAVE and Polyps in 2021, Right - Same region After APC treatment
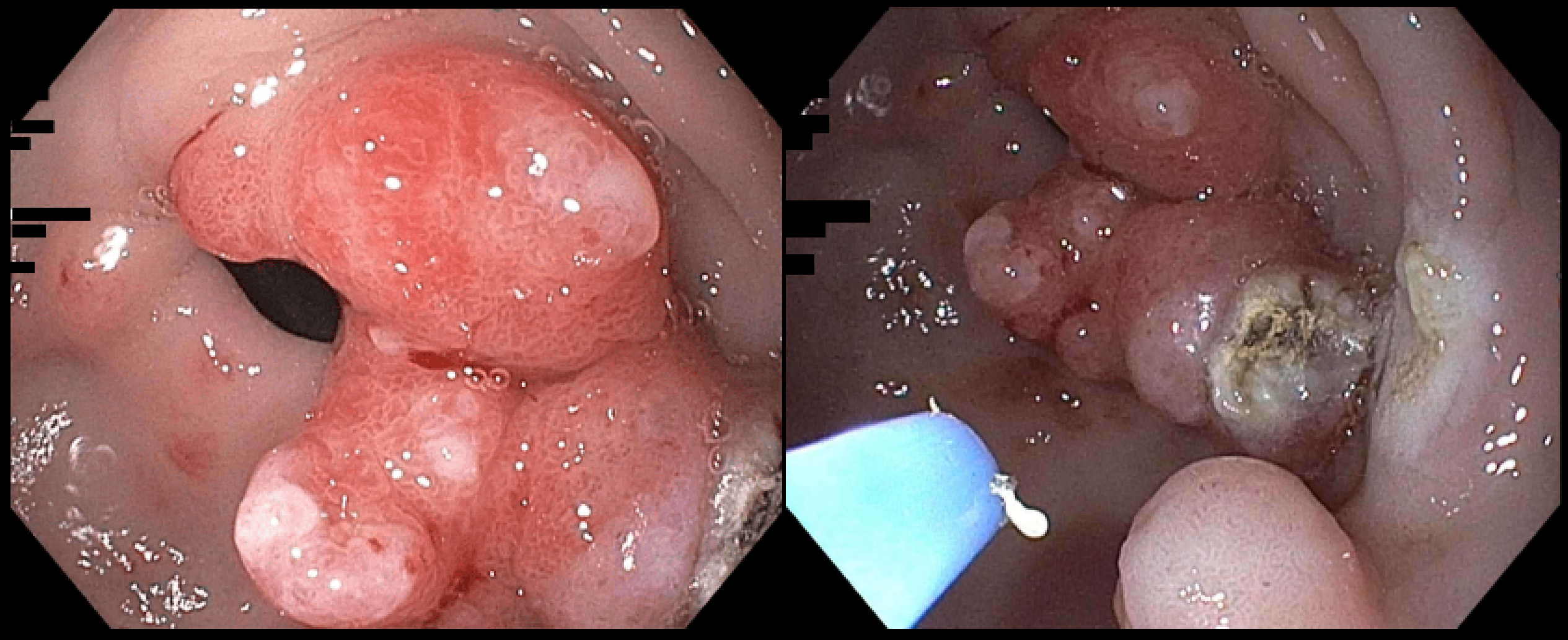
Figure: Left - Gastric Antrum with Antral Mass in 2024, Right - Same region After APC treatment
Disclosures:
Joanna Lenik indicated no relevant financial relationships.
Aria Khan indicated no relevant financial relationships.
Jennifer Harley indicated no relevant financial relationships.
Joanna Lenik, MD1, Aria Khan, MD2, Jennifer Harley, MD1. P6377 - From GAVE to Polyps: Is Treatment a Double-Edged Sword?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
