Tuesday Poster Session
Category: Stomach and Spleen
P6375 - Splenic Artery Hemorrhage as a Rare Delayed Complication of Percutaneous Endoscopic Gastrostomy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Joshua E. Pagán-Busigó, MD
Rutgers New Jersey Medical School
Kearny, NJ
Presenting Author(s)
Joshua E. Pagán-Busigó, MD1, Ethan Shamsian, MD2, Rohan Karkra, MBBS2, Mohammed Ayyad, MD2, Kranthi Mandava, MD2, Salil Chowdhury, MD2, Gokturk Suut, MD3
1Rutgers New Jersey Medical School, Kearny, NJ; 2Rutgers New Jersey Medical School, Newark, NJ; 3Rutgers New Jersey Medical School, Montville Township, NJ
Introduction: Percutaneous endoscopic gastrostomy (PEG) is a commonly performed procedure used to provide enteral access in patients with impaired swallowing. It is indicated in various clinical scenarios, including cerebrovascular accidents, head and neck cancers, and anatomical or functional bowel obstructions. Although generally safe, PEG placement carries procedural and post-procedural risks. While common complications include peristomal infection, tube dislodgement, and leakage, more serious events such as gastrointestinal or vascular injury can occur. Intra-abdominal hemorrhage, particularly from arterial sources, is extremely rare and potentially fatal. This case highlights a delayed and life-threatening splenic artery hemorrhage following PEG placement.
Case Description/
Methods: A 67-year-old male with a history of laryngeal carcinoma was admitted for sepsis in the setting of aspiration pneumonia. He improved with antibiotic therapy. After clinical stabilization, a modified barium swallow confirmed oropharyngeal dysphagia, likely secondary to prior radiotherapy. A PEG was placed for long-term nutritional support. The immediate post-procedural course was uneventful, aside from one episode of mild hematemesis. Seven days later, the patient developed acute abdominal pain, intolerance to enteral feeds, and passage of blood clots through the PEG tube. He became hypotensive and tachycardic, with a hemoglobin drop to 5.4 g/dL, requiring vasopressors and transfusions. Computed tomography angiography (CTA) of the abdomen revealed a hemorrhage in the lesser sac. Mesenteric angiography (MA) demonstrated active extravasation from a small branch of the splenic artery, which was embolized by interventional radiology. The patient recovered and was discharged with multidisciplinary follow-up.
Discussion: This case demonstrates a rare presentation of delayed hemorrhagic shock following PEG placement, caused by splenic artery bleeding. Although PEG is routinely performed, clinicians must remain aware of potentially life-threatening delayed complications. In this case, CTA was crucial for identifying intra-abdominal hemorrhage, and MA enabled definitive localization and embolization of the bleeding vessel. In patients presenting with new abdominal pain, unexplained anemia, or bleeding at the gastrostomy site, visceral arterial hemorrhage should be included in the differential. Early recognition along with prompt multidisciplinary intervention is essential to prevent fatal outcomes.

Figure: CTA of the abdomen revealing a hemorrhagic fluid collection (red arrow) within the lesser sac, interposed between the stomach and the pancreas.
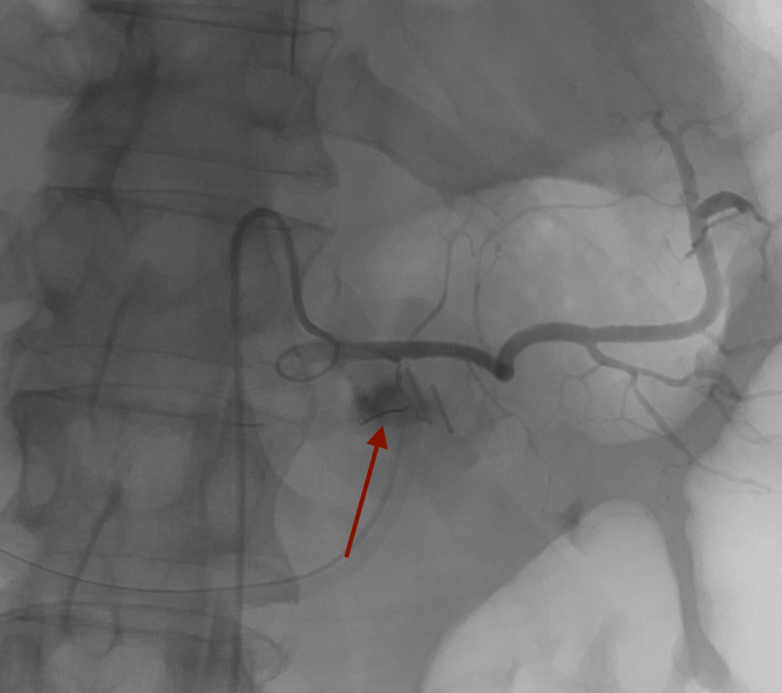
Figure: MA of the abdomen demonstrating a focal blush of contrast (red arrow), consistent with active extravasation from a small branch of the splenic artery.
Disclosures:
Joshua Pagán-Busigó indicated no relevant financial relationships.
Ethan Shamsian indicated no relevant financial relationships.
Rohan Karkra indicated no relevant financial relationships.
Mohammed Ayyad indicated no relevant financial relationships.
Kranthi Mandava indicated no relevant financial relationships.
Salil Chowdhury indicated no relevant financial relationships.
Gokturk Suut indicated no relevant financial relationships.
Joshua E. Pagán-Busigó, MD1, Ethan Shamsian, MD2, Rohan Karkra, MBBS2, Mohammed Ayyad, MD2, Kranthi Mandava, MD2, Salil Chowdhury, MD2, Gokturk Suut, MD3. P6375 - Splenic Artery Hemorrhage as a Rare Delayed Complication of Percutaneous Endoscopic Gastrostomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Kearny, NJ; 2Rutgers New Jersey Medical School, Newark, NJ; 3Rutgers New Jersey Medical School, Montville Township, NJ
Introduction: Percutaneous endoscopic gastrostomy (PEG) is a commonly performed procedure used to provide enteral access in patients with impaired swallowing. It is indicated in various clinical scenarios, including cerebrovascular accidents, head and neck cancers, and anatomical or functional bowel obstructions. Although generally safe, PEG placement carries procedural and post-procedural risks. While common complications include peristomal infection, tube dislodgement, and leakage, more serious events such as gastrointestinal or vascular injury can occur. Intra-abdominal hemorrhage, particularly from arterial sources, is extremely rare and potentially fatal. This case highlights a delayed and life-threatening splenic artery hemorrhage following PEG placement.
Case Description/
Methods: A 67-year-old male with a history of laryngeal carcinoma was admitted for sepsis in the setting of aspiration pneumonia. He improved with antibiotic therapy. After clinical stabilization, a modified barium swallow confirmed oropharyngeal dysphagia, likely secondary to prior radiotherapy. A PEG was placed for long-term nutritional support. The immediate post-procedural course was uneventful, aside from one episode of mild hematemesis. Seven days later, the patient developed acute abdominal pain, intolerance to enteral feeds, and passage of blood clots through the PEG tube. He became hypotensive and tachycardic, with a hemoglobin drop to 5.4 g/dL, requiring vasopressors and transfusions. Computed tomography angiography (CTA) of the abdomen revealed a hemorrhage in the lesser sac. Mesenteric angiography (MA) demonstrated active extravasation from a small branch of the splenic artery, which was embolized by interventional radiology. The patient recovered and was discharged with multidisciplinary follow-up.
Discussion: This case demonstrates a rare presentation of delayed hemorrhagic shock following PEG placement, caused by splenic artery bleeding. Although PEG is routinely performed, clinicians must remain aware of potentially life-threatening delayed complications. In this case, CTA was crucial for identifying intra-abdominal hemorrhage, and MA enabled definitive localization and embolization of the bleeding vessel. In patients presenting with new abdominal pain, unexplained anemia, or bleeding at the gastrostomy site, visceral arterial hemorrhage should be included in the differential. Early recognition along with prompt multidisciplinary intervention is essential to prevent fatal outcomes.

Figure: CTA of the abdomen revealing a hemorrhagic fluid collection (red arrow) within the lesser sac, interposed between the stomach and the pancreas.
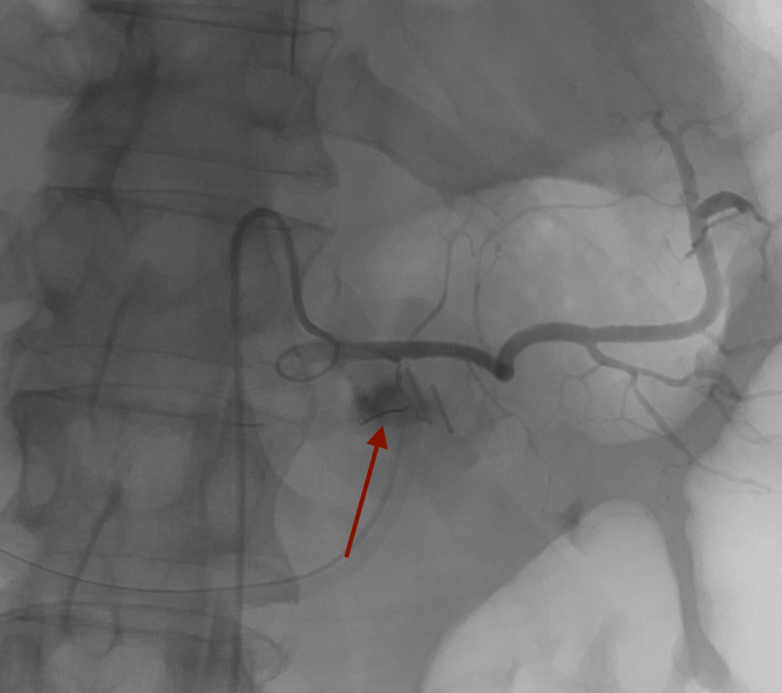
Figure: MA of the abdomen demonstrating a focal blush of contrast (red arrow), consistent with active extravasation from a small branch of the splenic artery.
Disclosures:
Joshua Pagán-Busigó indicated no relevant financial relationships.
Ethan Shamsian indicated no relevant financial relationships.
Rohan Karkra indicated no relevant financial relationships.
Mohammed Ayyad indicated no relevant financial relationships.
Kranthi Mandava indicated no relevant financial relationships.
Salil Chowdhury indicated no relevant financial relationships.
Gokturk Suut indicated no relevant financial relationships.
Joshua E. Pagán-Busigó, MD1, Ethan Shamsian, MD2, Rohan Karkra, MBBS2, Mohammed Ayyad, MD2, Kranthi Mandava, MD2, Salil Chowdhury, MD2, Gokturk Suut, MD3. P6375 - Splenic Artery Hemorrhage as a Rare Delayed Complication of Percutaneous Endoscopic Gastrostomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
