Tuesday Poster Session
Category: Stomach and Spleen
P6374 - Gastric Adenocarcinoma Presenting as Idiopathic Gastroparesis: A Diagnostic Pitfall
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Adrianna Wierzbicka, MD
Cleveland Clinic Florida
Weston, FL
Presenting Author(s)
Adrianna Wierzbicka, MD, Tasneem Jamal Al-Din, MD, Akram Ahmad, MD, Alison Schneider, MD, Andrew Ukleja, MD, CNSP
Cleveland Clinic Florida, Weston, FL
Introduction: Diffuse gastric adenocarcinoma can present insidiously mimicking benign gastric motility disorders. Its propensity for submucosal infiltration can lead to false-negative biopsies and diagnostic delays. This case underscores the limitations of conventional diagnostics in distinguishing severe gastroparesis (GP) from malignant gastric outlet obstruction (GOO) and the importance of re-evaluating presumed functional disorders when clinical and imaging findings raise concern.
Case Description/
Methods: A 49-year-old woman with a history of hemorrhagic stroke and GP presented with persistent nausea, daily non-bloody vomiting, and 100 Ibs unintentional weight loss over 6 months. She was diagnosed in outside hospital with severe idiopathic GP after a gastric emptying study showed complete absence of gastric content emptying at 2 hours. Initial endoscopy revealed gastritis, small antral erosions, and duodenitis, with negative biopsies for H. pylori and malignancy. CT showed gastric distension and antral wall thickening. She declined prokinetic therapy due to concerns about side effects. Her symptoms worsened despite supportive care. Repeat CT showed persistent gastric distension, concentric mural thickening of the distal stomach and pylorus (Figure 1). Repeat EGD revealed 650 mL of retained fluid and a friable, intrinsic antral stenosis that could not be traversed (Figure 2). Deep biopsies revealed reactive gastropathy but no malignancy. Subsequent imaging showed new ascites and peritoneal nodularity concerning for carcinomatosis. Upper GI contrast study showed complete GOO due to a 7.7 cm antral narrowing (Figure3). Diagnostic laparoscopy revealed diffuse peritoneal carcinomatosis with malignant ascites without evidence of hepatic metastasis. Histology confirmed poorly differentiated adenocarcinoma, positive for keratin, MOC-31, and Ber-EP4, and negative for calretinin. Tumor markers revealed elevated CA-125 of 813 U/mL with normal CEA. Palliative chemotherapy with docetaxel, cisplatin, and 5-fluorouracil was initiated. She was lost to follow-up and died 6 months later.
Discussion: This case highlights the diagnostic challenges of diffuse gastric adenocarcinoma, which can mimic idiopathic GP and evade detection on standard mucosal biopsies. Absent gastric emptying at 2 hours suggests obstruction or primary dysmotility, yet multiple endoscopic biopsies failed to confirm malignancy. A high clinical suspicion and early diagnostic laparoscopy are crucial to avoid misdiagnosis and treatment delays.
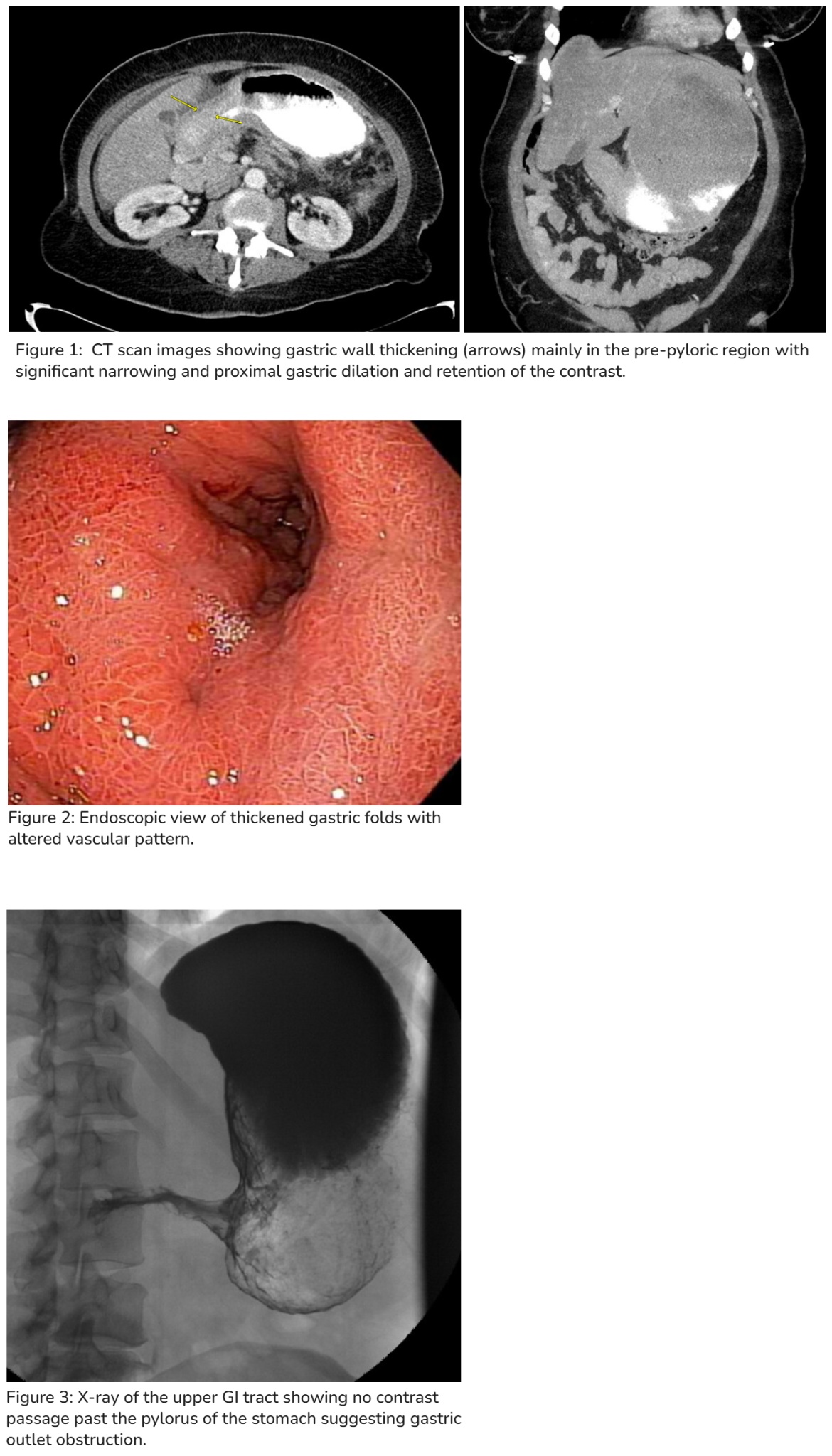
Figure: Figures
Disclosures:
Adrianna Wierzbicka indicated no relevant financial relationships.
Tasneem Jamal Al-Din indicated no relevant financial relationships.
Akram Ahmad indicated no relevant financial relationships.
Alison Schneider indicated no relevant financial relationships.
Andrew Ukleja indicated no relevant financial relationships.
Adrianna Wierzbicka, MD, Tasneem Jamal Al-Din, MD, Akram Ahmad, MD, Alison Schneider, MD, Andrew Ukleja, MD, CNSP. P6374 - Gastric Adenocarcinoma Presenting as Idiopathic Gastroparesis: A Diagnostic Pitfall, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Cleveland Clinic Florida, Weston, FL
Introduction: Diffuse gastric adenocarcinoma can present insidiously mimicking benign gastric motility disorders. Its propensity for submucosal infiltration can lead to false-negative biopsies and diagnostic delays. This case underscores the limitations of conventional diagnostics in distinguishing severe gastroparesis (GP) from malignant gastric outlet obstruction (GOO) and the importance of re-evaluating presumed functional disorders when clinical and imaging findings raise concern.
Case Description/
Methods: A 49-year-old woman with a history of hemorrhagic stroke and GP presented with persistent nausea, daily non-bloody vomiting, and 100 Ibs unintentional weight loss over 6 months. She was diagnosed in outside hospital with severe idiopathic GP after a gastric emptying study showed complete absence of gastric content emptying at 2 hours. Initial endoscopy revealed gastritis, small antral erosions, and duodenitis, with negative biopsies for H. pylori and malignancy. CT showed gastric distension and antral wall thickening. She declined prokinetic therapy due to concerns about side effects. Her symptoms worsened despite supportive care. Repeat CT showed persistent gastric distension, concentric mural thickening of the distal stomach and pylorus (Figure 1). Repeat EGD revealed 650 mL of retained fluid and a friable, intrinsic antral stenosis that could not be traversed (Figure 2). Deep biopsies revealed reactive gastropathy but no malignancy. Subsequent imaging showed new ascites and peritoneal nodularity concerning for carcinomatosis. Upper GI contrast study showed complete GOO due to a 7.7 cm antral narrowing (Figure3). Diagnostic laparoscopy revealed diffuse peritoneal carcinomatosis with malignant ascites without evidence of hepatic metastasis. Histology confirmed poorly differentiated adenocarcinoma, positive for keratin, MOC-31, and Ber-EP4, and negative for calretinin. Tumor markers revealed elevated CA-125 of 813 U/mL with normal CEA. Palliative chemotherapy with docetaxel, cisplatin, and 5-fluorouracil was initiated. She was lost to follow-up and died 6 months later.
Discussion: This case highlights the diagnostic challenges of diffuse gastric adenocarcinoma, which can mimic idiopathic GP and evade detection on standard mucosal biopsies. Absent gastric emptying at 2 hours suggests obstruction or primary dysmotility, yet multiple endoscopic biopsies failed to confirm malignancy. A high clinical suspicion and early diagnostic laparoscopy are crucial to avoid misdiagnosis and treatment delays.
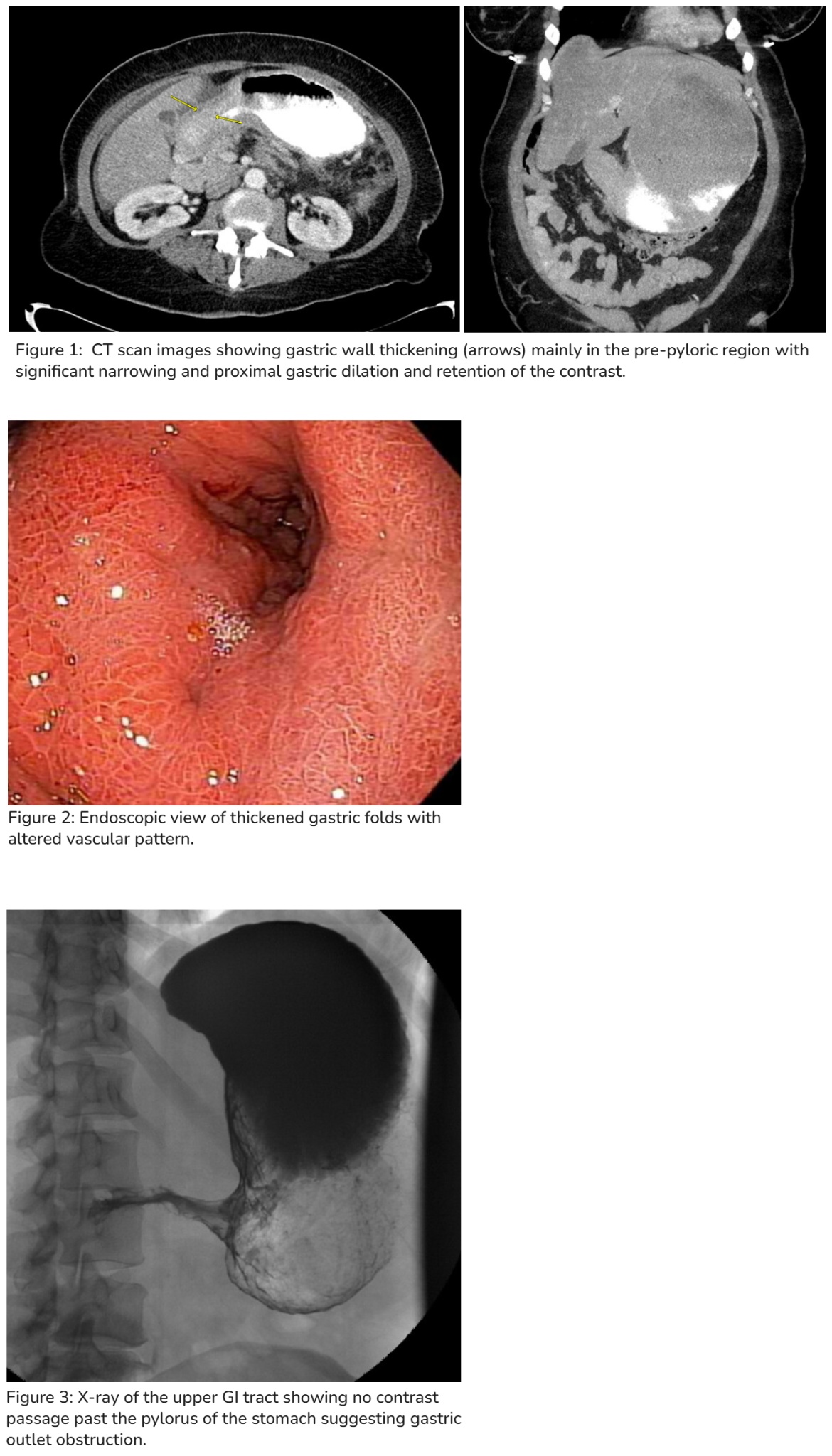
Figure: Figures
Disclosures:
Adrianna Wierzbicka indicated no relevant financial relationships.
Tasneem Jamal Al-Din indicated no relevant financial relationships.
Akram Ahmad indicated no relevant financial relationships.
Alison Schneider indicated no relevant financial relationships.
Andrew Ukleja indicated no relevant financial relationships.
Adrianna Wierzbicka, MD, Tasneem Jamal Al-Din, MD, Akram Ahmad, MD, Alison Schneider, MD, Andrew Ukleja, MD, CNSP. P6374 - Gastric Adenocarcinoma Presenting as Idiopathic Gastroparesis: A Diagnostic Pitfall, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
