Tuesday Poster Session
Category: Stomach and Spleen
P6372 - Gastrocolic Fistula: A Rare Late Complication of Percutaneous Endoscopic Gastrostomy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Freya R. Thummar, MBBS (she/her/hers)
C.U. Shah Medical Collage
Surat, Gujarat, India
Presenting Author(s)
Freya R. Thummar, MBBS1, Rahul Kumbhojkar, MBBS2, Haider Abbas. Naqvi, MD3, Sumanth Kumar. Bandaru, MBBS4
1C.U. Shah Medical Collage, Surat, Gujarat, India; 2Terna Medical College, Mumbai, Maharashtra, India; 3MedStar Franklin Square Medical Center, Baltimore, MD; 4MedStar Harbor Hospital, Baltimore, MD
Introduction: Percutaneous endoscopic gastrostomy(PEG) is a relatively safe procedure, multiple complications can still occur ranging from minor complications such as bleeding, wound infection, tube dysfunction to major complications such as necrotizing fasciitis and Colonic fistulas.
Case Description/
Methods: A 78-year-old man with medical history of epiglottic cancer, dysphagia requiring PEG tube placement presented with irritation and discomfort around the PEG tube for 2 weeks. He denied abdominal pain, diarrhea, vomiting and fever.
Patient had undergone uneventful PEG tube placement 10 months ago which was indicated due to long term nutritional needs secondary to dysphagia and odynophagia following radiation therapy for epiglottic cancer. Physical examination revealed a minimal brownish-black discharge around the PEG tube without any erythema or induration. Lab work was unremarkable.
A computed tomography (CT) scan with IV contrast of the abdomen and pelvis revealed diffuse wall thickening of the stomach and an elongated colon with PEG tube positioned in the stomach antrum. There was no abnormal fluid or abscess around the entry site or in the intra-abdominal course of gastrostomy tube. Based on the findings from the CT scan, acute gastritis was suspected and treated with a proton pump inhibitor. As the patient was hemodynamically stable with unremarkable lab work, He was discharged from the emergency department.
A week later, the patient presented to hospital with fecal matter discharge from the PEG tube. Contrast-enhanced (oral) abdominal and pelvic CT scan revealed PEG tube tracking along the superior portion of the transverse colon, with the contrast filling the colon confirming gastrocolic fistula(GCF). Patient was recommended for laparotomy, removal of the PEG tube, and placement of a new feeding tube but the patient's family denied the surgery and chose to pursue hospice care.
Discussion: GCF is a rare but serious late complication of PEG tube insertion with incidence rates of 0.5–3%. It occurs due to inadvertent colonic injury or tube migration, creating an abnormal connection between the stomach and colon. Patients can typically be asymptomatic but can present with diarrhea, nausea, vomiting, abdominal pain, or fecal discharge from PEG tube. Contrast imaging is key for confirmation, and management typically involves PEG tube removal, with surgical intervention. Early recognition and proper PEG placement techniques are crucial to preventing GCF and improving patient outcomes.
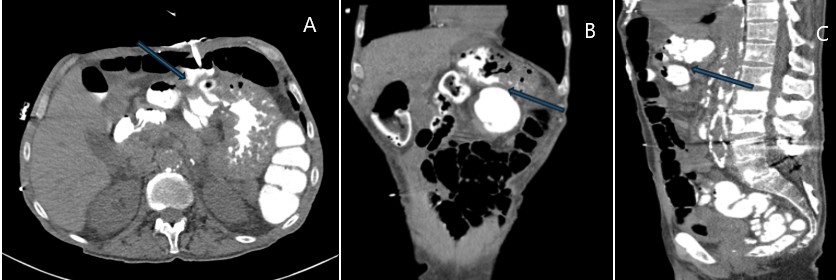
Figure: Axial (A), coronal (B) and sagittal (C) post contrast images of abdomen and pelvis showing gastro-colonic fistula ( blue arrows) demonstrating contrast in the transverse after introduction of oral contrast via gastrostomy tube.
Disclosures:
Freya Thummar indicated no relevant financial relationships.
Rahul Kumbhojkar indicated no relevant financial relationships.
Haider Naqvi indicated no relevant financial relationships.
Sumanth Bandaru indicated no relevant financial relationships.
Freya R. Thummar, MBBS1, Rahul Kumbhojkar, MBBS2, Haider Abbas. Naqvi, MD3, Sumanth Kumar. Bandaru, MBBS4. P6372 - Gastrocolic Fistula: A Rare Late Complication of Percutaneous Endoscopic Gastrostomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1C.U. Shah Medical Collage, Surat, Gujarat, India; 2Terna Medical College, Mumbai, Maharashtra, India; 3MedStar Franklin Square Medical Center, Baltimore, MD; 4MedStar Harbor Hospital, Baltimore, MD
Introduction: Percutaneous endoscopic gastrostomy(PEG) is a relatively safe procedure, multiple complications can still occur ranging from minor complications such as bleeding, wound infection, tube dysfunction to major complications such as necrotizing fasciitis and Colonic fistulas.
Case Description/
Methods: A 78-year-old man with medical history of epiglottic cancer, dysphagia requiring PEG tube placement presented with irritation and discomfort around the PEG tube for 2 weeks. He denied abdominal pain, diarrhea, vomiting and fever.
Patient had undergone uneventful PEG tube placement 10 months ago which was indicated due to long term nutritional needs secondary to dysphagia and odynophagia following radiation therapy for epiglottic cancer. Physical examination revealed a minimal brownish-black discharge around the PEG tube without any erythema or induration. Lab work was unremarkable.
A computed tomography (CT) scan with IV contrast of the abdomen and pelvis revealed diffuse wall thickening of the stomach and an elongated colon with PEG tube positioned in the stomach antrum. There was no abnormal fluid or abscess around the entry site or in the intra-abdominal course of gastrostomy tube. Based on the findings from the CT scan, acute gastritis was suspected and treated with a proton pump inhibitor. As the patient was hemodynamically stable with unremarkable lab work, He was discharged from the emergency department.
A week later, the patient presented to hospital with fecal matter discharge from the PEG tube. Contrast-enhanced (oral) abdominal and pelvic CT scan revealed PEG tube tracking along the superior portion of the transverse colon, with the contrast filling the colon confirming gastrocolic fistula(GCF). Patient was recommended for laparotomy, removal of the PEG tube, and placement of a new feeding tube but the patient's family denied the surgery and chose to pursue hospice care.
Discussion: GCF is a rare but serious late complication of PEG tube insertion with incidence rates of 0.5–3%. It occurs due to inadvertent colonic injury or tube migration, creating an abnormal connection between the stomach and colon. Patients can typically be asymptomatic but can present with diarrhea, nausea, vomiting, abdominal pain, or fecal discharge from PEG tube. Contrast imaging is key for confirmation, and management typically involves PEG tube removal, with surgical intervention. Early recognition and proper PEG placement techniques are crucial to preventing GCF and improving patient outcomes.
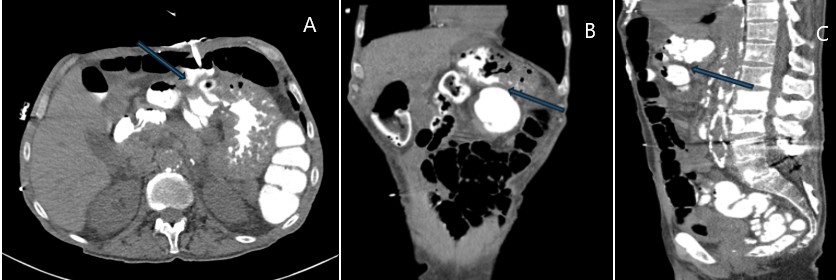
Figure: Axial (A), coronal (B) and sagittal (C) post contrast images of abdomen and pelvis showing gastro-colonic fistula ( blue arrows) demonstrating contrast in the transverse after introduction of oral contrast via gastrostomy tube.
Disclosures:
Freya Thummar indicated no relevant financial relationships.
Rahul Kumbhojkar indicated no relevant financial relationships.
Haider Naqvi indicated no relevant financial relationships.
Sumanth Bandaru indicated no relevant financial relationships.
Freya R. Thummar, MBBS1, Rahul Kumbhojkar, MBBS2, Haider Abbas. Naqvi, MD3, Sumanth Kumar. Bandaru, MBBS4. P6372 - Gastrocolic Fistula: A Rare Late Complication of Percutaneous Endoscopic Gastrostomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
