Tuesday Poster Session
Category: Stomach and Spleen
P6415 - Reducing Radiation and Intervention: The Role of Point-of-Care Ultrasound in Tracking Gastrointestinal Foreign Bodies
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mehak Sharma, MD
Florida International University
Miami, FL
Presenting Author(s)
Mehak Sharma, MD, Guillermo Izquierdo-Pretel, MD, Joel Mantilla, MHS, Carolina Valdes-Guicciardi, BS
Florida International University, Miami, FL
Introduction: In adults, foreign body ingestion is often associated with psychiatric disorders, incarceration, or intellectual disabilities, with intentional ingestion being especially prevalent in prison populations. While most ingested objects pass spontaneously, 10–20% requires endoscopic intervention, and less than 1% necessitates surgical procedures. Plain radiographs have been the primary diagnostic tool, providing information on the location, size, shape, and number of ingested foreign bodies, and helping to exclude aspiration. However, radiolucent materials, such as chicken bones and thin metal objects are often not visible on X-rays. Ultrasound has not been incorporated into standard diagnostic guidelines, and there remains a paucity of literature supporting its routine use in the evaluation of gastrointestinal foreign body ingestion.
Case Description/
Methods: A 25-year-old male from a corrections facility with a history of psychiatric disorder, specifically antisocial personality disorder, presented to the emergency department after ingesting a foreign body, a screw. The patient reported swallowing the screw impulsively in an attempt to be removed from confinement. He was asymptomatic upon arrival and had a normal physical exam. A kidney, ureter, and bladder (KUB) scan identified a flat-tip screw, measuring 22 mm x 13 mm, located in the distal stomach. A gastroenterology consultation was obtained, and it was recommended that the patient remain nil per os (NPO) with daily KUB scans to monitor the screw’s progression. Since the screw was less than 2.5 cm in size, endoscopic removal was not necessary.
Discussion: This case aims to determine the effectiveness of POCUS in managing GI foreign body ingestion, particularly in populations at higher risk. Repeated imaging to monitor the progression of a foreign body often results in increased radiation exposure and may cause patient discomfort, especially in cases requiring serial assessments. The use of POCUS within the GI system remains underexplored. The foreign body consistently appeared as a hyperechoic linear structure on POCUS, allowing for real-time visualization at every stage transit. The ability to perform serial bedside ultrasounds provided a non-invasive, radiation-free means of tracking the foreign body, offering advantages in patient safety. Furthermore, the cost-effectiveness and ease of access associated with POCUS make it a valuable tool when rapid decision-making is required, such as emergency departments and correctional facilities.
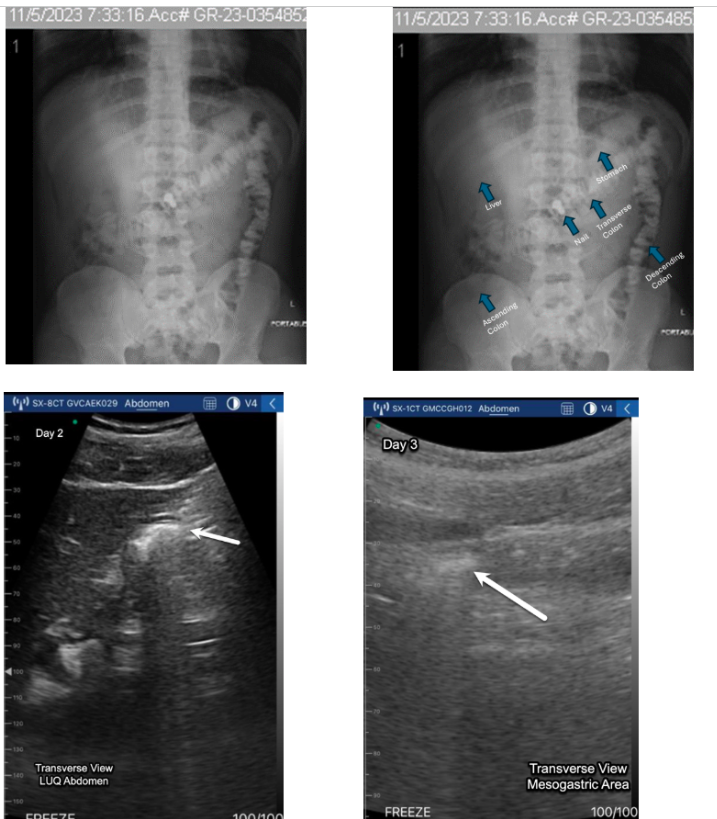
Figure: Figure 1 (top): On day 1, a KUB scan revealed the screw projecting over the upper central abdomen, likely in the region of the distal stomach body.
Figure 2 (bottom): On day 2, the KUB showed the screw projecting over the bowel topography in the left upper quadrant. Oral contrast was noted over the gastric region, and the visualized portion of the abdomen displayed a nonobstructive bowel gas pattern.
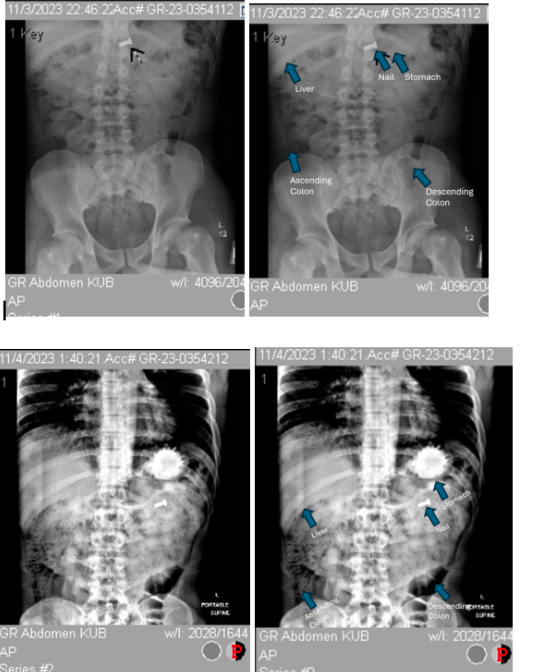
Figure: Figure 3 (top): On day 3, the KUB demonstrated that the screw had moved to the mid-upper abdomen, possibly within the transverse colon. The bowel gas pattern remained nonobstructive, and enteric contrast was visible within the large bowel.
Figure 4 (bottom left): On day 2, POCUS identified a hyperechoic linear structure with an associated acoustic shadow in the left upper quadrant (LUQ).
Figure 5 (bottom right): On day 3, POCUS again detected a hyperechoic linear structure and acoustic shadow, this time located in the mesogastric area, confirming the screw’s progression through the gastrointestinal tract.
Disclosures:
Mehak Sharma indicated no relevant financial relationships.
Guillermo Izquierdo-Pretel indicated no relevant financial relationships.
Joel Mantilla indicated no relevant financial relationships.
Carolina Valdes-Guicciardi indicated no relevant financial relationships.
Mehak Sharma, MD, Guillermo Izquierdo-Pretel, MD, Joel Mantilla, MHS, Carolina Valdes-Guicciardi, BS. P6415 - Reducing Radiation and Intervention: The Role of Point-of-Care Ultrasound in Tracking Gastrointestinal Foreign Bodies, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Florida International University, Miami, FL
Introduction: In adults, foreign body ingestion is often associated with psychiatric disorders, incarceration, or intellectual disabilities, with intentional ingestion being especially prevalent in prison populations. While most ingested objects pass spontaneously, 10–20% requires endoscopic intervention, and less than 1% necessitates surgical procedures. Plain radiographs have been the primary diagnostic tool, providing information on the location, size, shape, and number of ingested foreign bodies, and helping to exclude aspiration. However, radiolucent materials, such as chicken bones and thin metal objects are often not visible on X-rays. Ultrasound has not been incorporated into standard diagnostic guidelines, and there remains a paucity of literature supporting its routine use in the evaluation of gastrointestinal foreign body ingestion.
Case Description/
Methods: A 25-year-old male from a corrections facility with a history of psychiatric disorder, specifically antisocial personality disorder, presented to the emergency department after ingesting a foreign body, a screw. The patient reported swallowing the screw impulsively in an attempt to be removed from confinement. He was asymptomatic upon arrival and had a normal physical exam. A kidney, ureter, and bladder (KUB) scan identified a flat-tip screw, measuring 22 mm x 13 mm, located in the distal stomach. A gastroenterology consultation was obtained, and it was recommended that the patient remain nil per os (NPO) with daily KUB scans to monitor the screw’s progression. Since the screw was less than 2.5 cm in size, endoscopic removal was not necessary.
Discussion: This case aims to determine the effectiveness of POCUS in managing GI foreign body ingestion, particularly in populations at higher risk. Repeated imaging to monitor the progression of a foreign body often results in increased radiation exposure and may cause patient discomfort, especially in cases requiring serial assessments. The use of POCUS within the GI system remains underexplored. The foreign body consistently appeared as a hyperechoic linear structure on POCUS, allowing for real-time visualization at every stage transit. The ability to perform serial bedside ultrasounds provided a non-invasive, radiation-free means of tracking the foreign body, offering advantages in patient safety. Furthermore, the cost-effectiveness and ease of access associated with POCUS make it a valuable tool when rapid decision-making is required, such as emergency departments and correctional facilities.
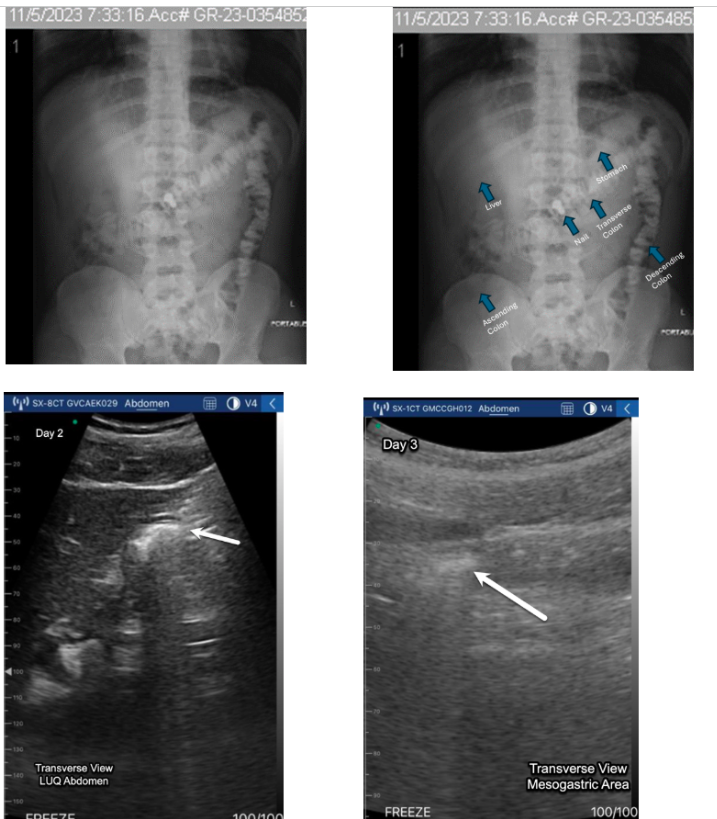
Figure: Figure 1 (top): On day 1, a KUB scan revealed the screw projecting over the upper central abdomen, likely in the region of the distal stomach body.
Figure 2 (bottom): On day 2, the KUB showed the screw projecting over the bowel topography in the left upper quadrant. Oral contrast was noted over the gastric region, and the visualized portion of the abdomen displayed a nonobstructive bowel gas pattern.
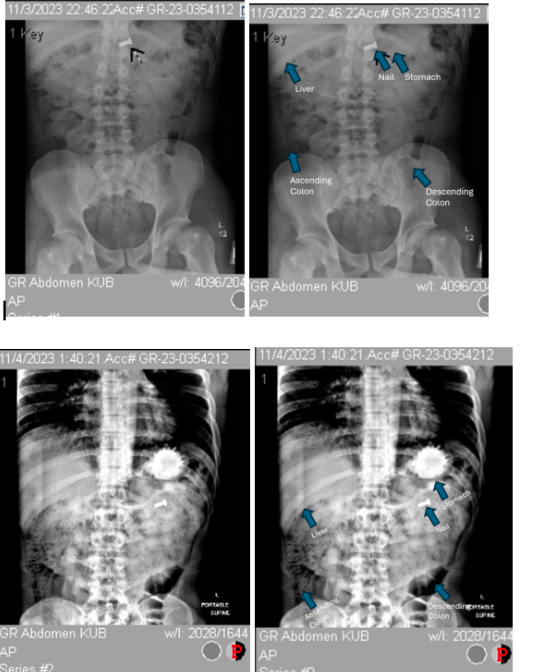
Figure: Figure 3 (top): On day 3, the KUB demonstrated that the screw had moved to the mid-upper abdomen, possibly within the transverse colon. The bowel gas pattern remained nonobstructive, and enteric contrast was visible within the large bowel.
Figure 4 (bottom left): On day 2, POCUS identified a hyperechoic linear structure with an associated acoustic shadow in the left upper quadrant (LUQ).
Figure 5 (bottom right): On day 3, POCUS again detected a hyperechoic linear structure and acoustic shadow, this time located in the mesogastric area, confirming the screw’s progression through the gastrointestinal tract.
Disclosures:
Mehak Sharma indicated no relevant financial relationships.
Guillermo Izquierdo-Pretel indicated no relevant financial relationships.
Joel Mantilla indicated no relevant financial relationships.
Carolina Valdes-Guicciardi indicated no relevant financial relationships.
Mehak Sharma, MD, Guillermo Izquierdo-Pretel, MD, Joel Mantilla, MHS, Carolina Valdes-Guicciardi, BS. P6415 - Reducing Radiation and Intervention: The Role of Point-of-Care Ultrasound in Tracking Gastrointestinal Foreign Bodies, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

