Tuesday Poster Session
Category: Stomach and Spleen
P6414 - Early Buried Bumper Syndrome: A Targeted Approach to Salvage a Recent PEG Site and Restore Enteral Access
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mina Awadallah, MD, MSc
University of Utah
Salt Lake City, UT
Presenting Author(s)
Mina Awadallah, MD, MSc1, Christopher Ko, MD1, John Fang, MD1, John Erikson Yap, MD, MBA, FACG2
1University of Utah, Salt Lake City, UT; 2University of Utah Health, Salt Lake City, UT
Introduction: Buried bumper syndrome (BBS) is an uncommon but serious complication of percutaneous endoscopic gastrostomy (PEG) tube placement, in which the internal bumper migrates into the gastric wall. Risk factors include excessive bumper tension, malnutrition, and impaired wound healing. Clinicians should maintain a high index of suspicion in patients presenting with persistent or worsening abdominal pain after PEG placement. Imaging and endoscopic evaluation are critical for timely diagnosis and management, which may help prevent complications such as perforation or peritonitis.
Case Description/
Methods: A 51-year-old female with a 20 Fr PEG placed 10 days prior presented with persistent and worsening abdominal pain, along with nausea and vomiting. A CT scan revealed migration of the internal bumper into the gastric muscularis, consistent with early buried bumper syndrome. Esophagogastroduodenoscopy (EGD) confirmed the finding, with the bumper embedded within the gastric wall. The gastrostomy tract was wide measuring 10-12 mm in diameter with ulceration inside the tract, allowing the endoscope to pass easily through the fistula.
Given her need for ongoing enteral nutrition and the recent timing of PEG placement, the team opted to salvage the existing tract. A guidewire was passed through the PEG to secure access, and the buried tube was gently removed using traction and torsion. A new 20 Fr PEG tube was then placed using a pull technique through the same tract. Due to mucosal oozing after removal of the old PEG tube and the large diameter of the fistulous tract, RADA 16 gel was applied to the fistula for hemostasis and healing, and the gastric side was endoscopically sutured to reduce the fistula diameter to approximately 7 mm. Final endoscopic appearance of the new PEG was satisfactory, and the patient's symptoms improved following the procedure and was able to continue using her PEG tube.
Discussion: This case highlights a practical and minimally invasive approach to managing early BBS. BBS should be considered in patients with ongoing pain post-PEG placement, and imaging plus EGD can guide diagnosis and tailor interventions. While re-siting the PEG may be necessary, early identification may allow for preservation of the existing tract. The combination modality of endoscopic suturing and RADA 16 application successfully helped salvage the existing tract in our case. Salvage techniques may be appropriate in selected cases with early presentation and favorable anatomy.
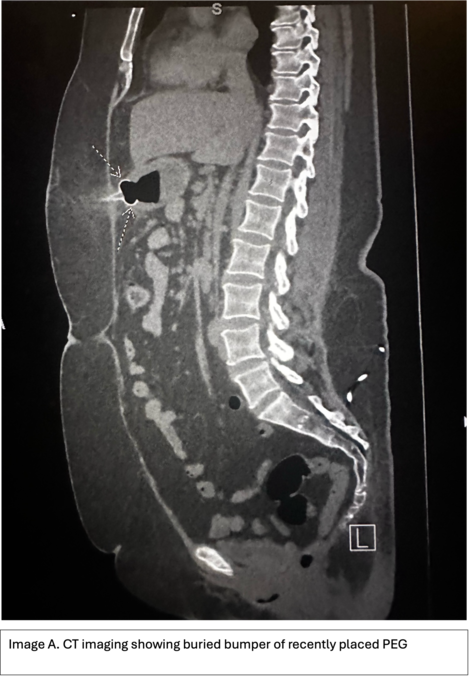
Figure: Image A. CT imaging showing buried bumper of recently placed PEG.
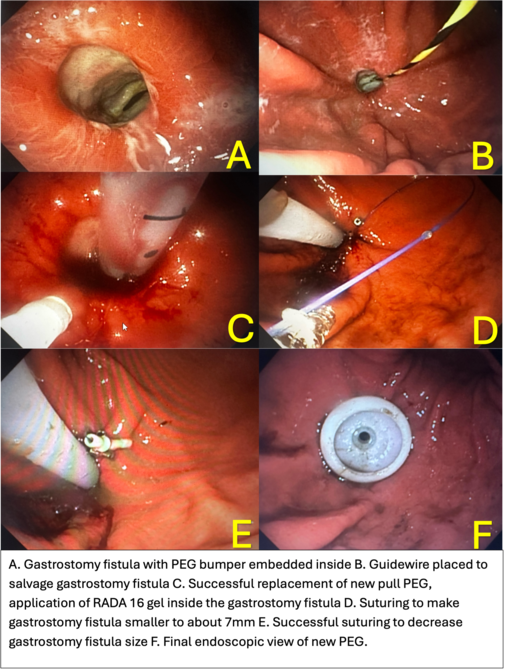
Figure: A. Gastrostomy fistula with PEG bumper embedded inside B. Guidewire placed to salvage gastrostomy fistula C. Successful replacement of new pull PEG, application of RADA 16 gel inside the gastrostomy fistula D. Suturing to make gastrostomy fistula smaller to about 7mm E. Successful suturing to decrease gastrostomy fistula size F. Final endoscopic view of new PEG.
Disclosures:
Mina Awadallah indicated no relevant financial relationships.
Christopher Ko indicated no relevant financial relationships.
John Fang: Aspero Medical – Consultant. Circa Scientific – Consultant. Merit – Consultant.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Mina Awadallah, MD, MSc1, Christopher Ko, MD1, John Fang, MD1, John Erikson Yap, MD, MBA, FACG2. P6414 - Early Buried Bumper Syndrome: A Targeted Approach to Salvage a Recent PEG Site and Restore Enteral Access, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Utah, Salt Lake City, UT; 2University of Utah Health, Salt Lake City, UT
Introduction: Buried bumper syndrome (BBS) is an uncommon but serious complication of percutaneous endoscopic gastrostomy (PEG) tube placement, in which the internal bumper migrates into the gastric wall. Risk factors include excessive bumper tension, malnutrition, and impaired wound healing. Clinicians should maintain a high index of suspicion in patients presenting with persistent or worsening abdominal pain after PEG placement. Imaging and endoscopic evaluation are critical for timely diagnosis and management, which may help prevent complications such as perforation or peritonitis.
Case Description/
Methods: A 51-year-old female with a 20 Fr PEG placed 10 days prior presented with persistent and worsening abdominal pain, along with nausea and vomiting. A CT scan revealed migration of the internal bumper into the gastric muscularis, consistent with early buried bumper syndrome. Esophagogastroduodenoscopy (EGD) confirmed the finding, with the bumper embedded within the gastric wall. The gastrostomy tract was wide measuring 10-12 mm in diameter with ulceration inside the tract, allowing the endoscope to pass easily through the fistula.
Given her need for ongoing enteral nutrition and the recent timing of PEG placement, the team opted to salvage the existing tract. A guidewire was passed through the PEG to secure access, and the buried tube was gently removed using traction and torsion. A new 20 Fr PEG tube was then placed using a pull technique through the same tract. Due to mucosal oozing after removal of the old PEG tube and the large diameter of the fistulous tract, RADA 16 gel was applied to the fistula for hemostasis and healing, and the gastric side was endoscopically sutured to reduce the fistula diameter to approximately 7 mm. Final endoscopic appearance of the new PEG was satisfactory, and the patient's symptoms improved following the procedure and was able to continue using her PEG tube.
Discussion: This case highlights a practical and minimally invasive approach to managing early BBS. BBS should be considered in patients with ongoing pain post-PEG placement, and imaging plus EGD can guide diagnosis and tailor interventions. While re-siting the PEG may be necessary, early identification may allow for preservation of the existing tract. The combination modality of endoscopic suturing and RADA 16 application successfully helped salvage the existing tract in our case. Salvage techniques may be appropriate in selected cases with early presentation and favorable anatomy.
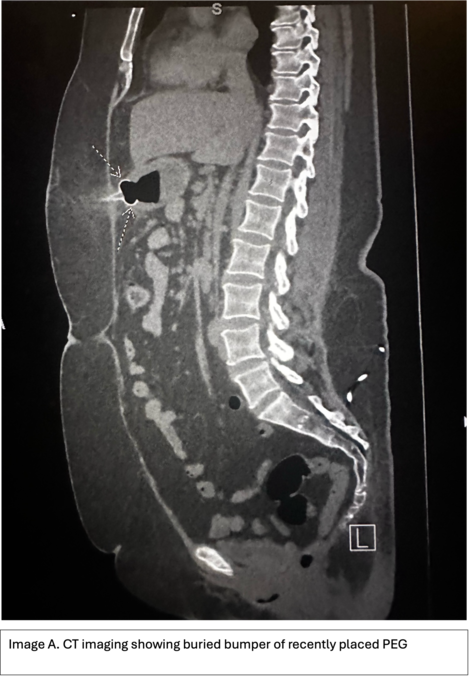
Figure: Image A. CT imaging showing buried bumper of recently placed PEG.
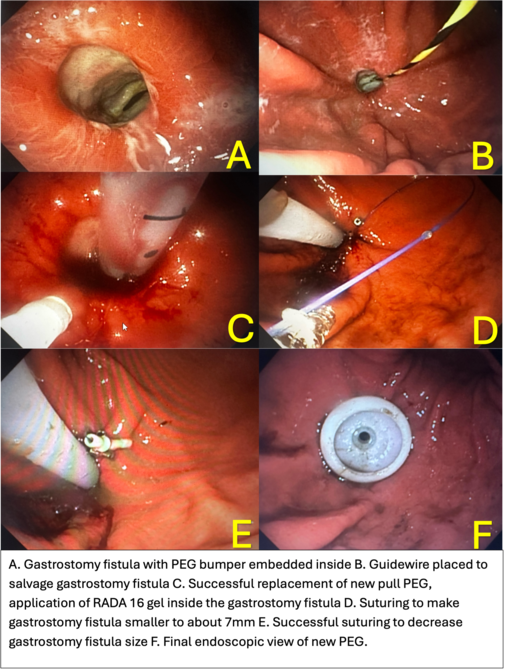
Figure: A. Gastrostomy fistula with PEG bumper embedded inside B. Guidewire placed to salvage gastrostomy fistula C. Successful replacement of new pull PEG, application of RADA 16 gel inside the gastrostomy fistula D. Suturing to make gastrostomy fistula smaller to about 7mm E. Successful suturing to decrease gastrostomy fistula size F. Final endoscopic view of new PEG.
Disclosures:
Mina Awadallah indicated no relevant financial relationships.
Christopher Ko indicated no relevant financial relationships.
John Fang: Aspero Medical – Consultant. Circa Scientific – Consultant. Merit – Consultant.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Mina Awadallah, MD, MSc1, Christopher Ko, MD1, John Fang, MD1, John Erikson Yap, MD, MBA, FACG2. P6414 - Early Buried Bumper Syndrome: A Targeted Approach to Salvage a Recent PEG Site and Restore Enteral Access, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
