Tuesday Poster Session
Category: Stomach and Spleen
P6411 - A Twisted Tale: Median Arcuate Ligament Syndrome (MALS) in a Patient with Intestinal Malrotation
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Panida Charnvitayapong, MD (she/her/hers)
University of Miami Miller School of Medicine at JFK Medical Center
Atlantis, FL
Presenting Author(s)
Panida Charnvitayapong, MD1, Michelle Lopez Baez, MD1, Bebika Subedi, MD1, Shaun Isaac, MD2
1University of Miami Miller School of Medicine at JFK Medical Center, Atlantis, FL; 2HCA Florida Healthcare, Atlantis, FL
Introduction: Median Arcuate Ligament Syndrome (MALS), also known as celiac artery compression syndrome or Dunbar syndrome, is a rare condition with unclear etiology involving extrinsic compression of the celiac axis. It can lead to nonspecific clinical symptoms of postprandial epigastric pain, nausea, vomiting, and weight loss.
Here, we present a patient with MALS and unique anatomy.
Case Description/
Methods: A 45-year-old male with no medical history presented with five days of worsening abdominal pain localized to the periumbilical region and bilateral lower quadrants. He described the pain as more severe than the intermittent abdominal discomfort he had experienced since childhood. He reported one episode of vomiting, early satiety, decreased appetite, and unquantified weight loss. He otherwise endorsed occasional blood when wiping but denied diarrhea, recent illness, or sick contacts.
CT abdomen/pelvis showed approximately 70% celiac axis stenosis, malrotated bowel, and the appendix in the left midabdomen. US duplex scan of the abdomen showed a patent artery without stenosis. After confirmation of MALS, the option for surgery was presented to the patient, who was instructed to follow up outpatient.
Discussion: MALS remains poorly understood with unclear mechanism of pain. Pain is often present in the upper abdomen or epigastric region and typically worsens after meals, exercise, or leaning forward. It may also lead to "food fear" or when patients develop anxiety with eating due to the anticipation of postprandial abdominal pain, which can lead to severe weight loss or malnutrition. Proposed mechanisms include foregut ischemia from direct celiac artery compression, midgut ischemia due to "steal" phenomena through superior mesenteric artery (SMA) collaterals, or splanchnic vasoconstriction/ischemia from chronic celiac plexus irritation.
Imaging such as computed tomography angiography (CTA), magnetic resonance angiography (MRA), or duplex ultrasound confirms the diagnosis, typically showing a characteristic "hooked" or "J-shaped" appearance of the compressed celiac artery. Definitive management is surgical with laparoscopic release of the median arcuate ligament. In refractory cases, angioplasty, stenting, or vascular reconstruction may be necessary.
While the clinical scenario was further complicated in this patient by underlying intestinal malrotation, the aforementioned etiologies are considered. Recognizing anatomical variants when evaluating MALS and planning effective treatment strategies is crucial.
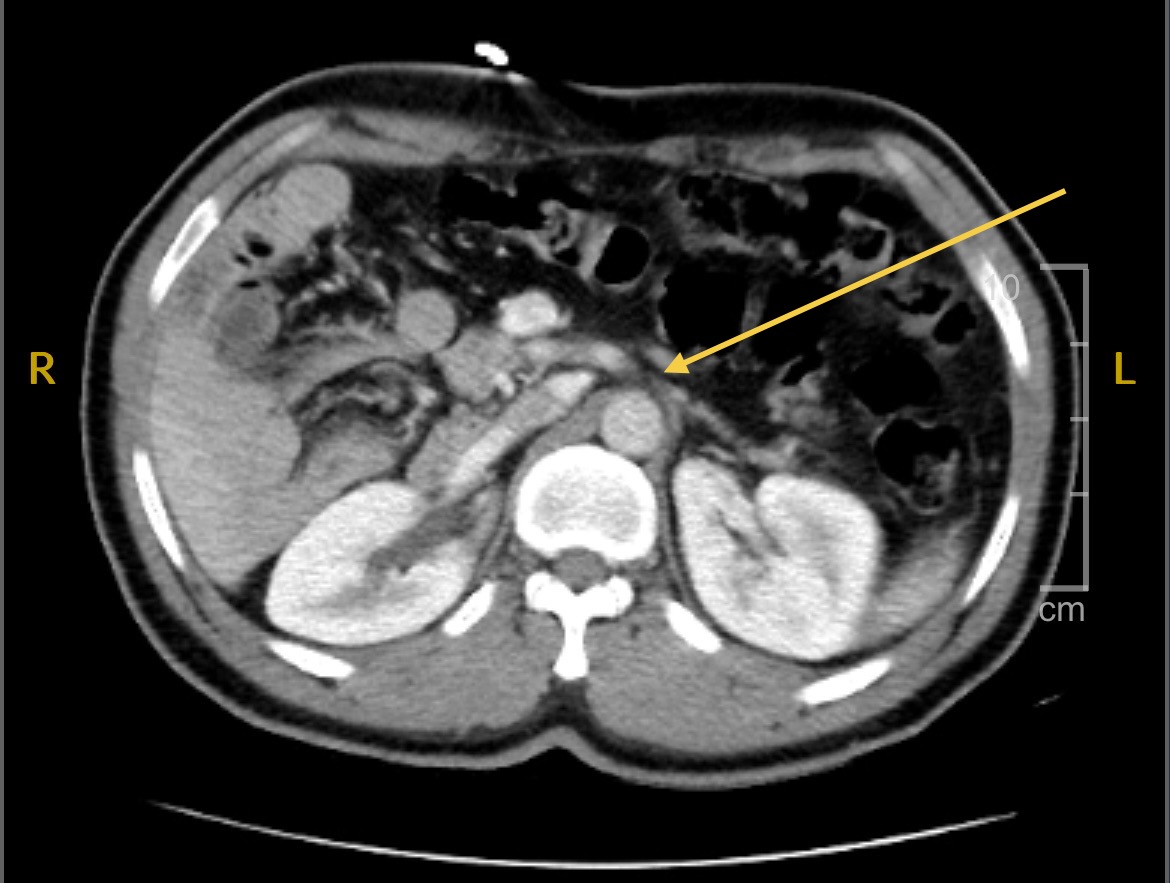
Figure: CT Abdomen/Pelvis (axial): Approximately about 70% celiac axis stenosis (indicated by yellow arrow). Malrotated bowel. Small bowel mainly in the right midabdomen.
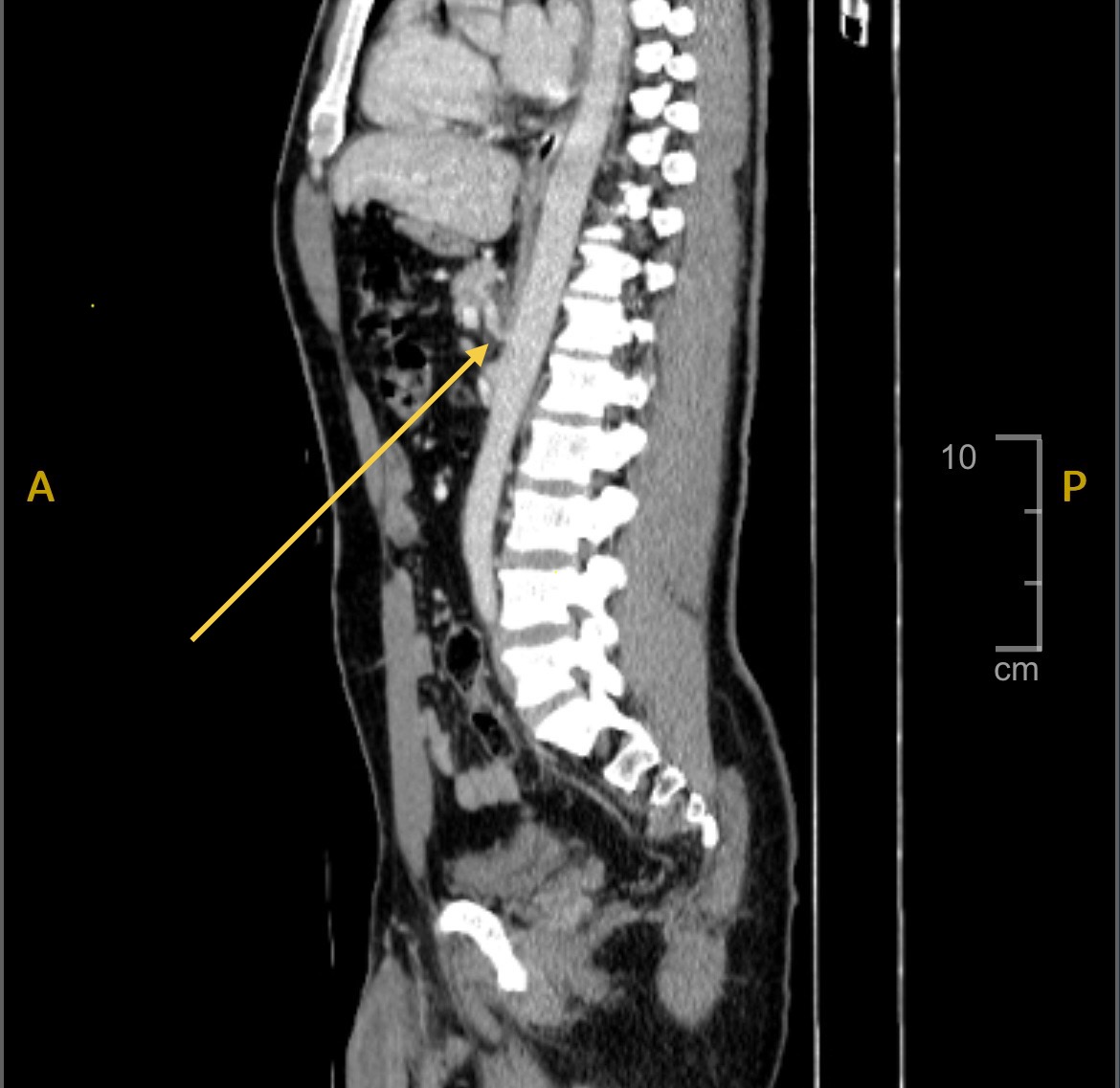
Figure: CT Abdomen/Pelvis (sagittal): Characteristic "J-shaped" or "Hooked" appearance indicating compression
Disclosures:
Panida Charnvitayapong indicated no relevant financial relationships.
Michelle Lopez Baez indicated no relevant financial relationships.
Bebika Subedi indicated no relevant financial relationships.
Shaun Isaac indicated no relevant financial relationships.
Panida Charnvitayapong, MD1, Michelle Lopez Baez, MD1, Bebika Subedi, MD1, Shaun Isaac, MD2. P6411 - A Twisted Tale: Median Arcuate Ligament Syndrome (MALS) in a Patient with Intestinal Malrotation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Miami Miller School of Medicine at JFK Medical Center, Atlantis, FL; 2HCA Florida Healthcare, Atlantis, FL
Introduction: Median Arcuate Ligament Syndrome (MALS), also known as celiac artery compression syndrome or Dunbar syndrome, is a rare condition with unclear etiology involving extrinsic compression of the celiac axis. It can lead to nonspecific clinical symptoms of postprandial epigastric pain, nausea, vomiting, and weight loss.
Here, we present a patient with MALS and unique anatomy.
Case Description/
Methods: A 45-year-old male with no medical history presented with five days of worsening abdominal pain localized to the periumbilical region and bilateral lower quadrants. He described the pain as more severe than the intermittent abdominal discomfort he had experienced since childhood. He reported one episode of vomiting, early satiety, decreased appetite, and unquantified weight loss. He otherwise endorsed occasional blood when wiping but denied diarrhea, recent illness, or sick contacts.
CT abdomen/pelvis showed approximately 70% celiac axis stenosis, malrotated bowel, and the appendix in the left midabdomen. US duplex scan of the abdomen showed a patent artery without stenosis. After confirmation of MALS, the option for surgery was presented to the patient, who was instructed to follow up outpatient.
Discussion: MALS remains poorly understood with unclear mechanism of pain. Pain is often present in the upper abdomen or epigastric region and typically worsens after meals, exercise, or leaning forward. It may also lead to "food fear" or when patients develop anxiety with eating due to the anticipation of postprandial abdominal pain, which can lead to severe weight loss or malnutrition. Proposed mechanisms include foregut ischemia from direct celiac artery compression, midgut ischemia due to "steal" phenomena through superior mesenteric artery (SMA) collaterals, or splanchnic vasoconstriction/ischemia from chronic celiac plexus irritation.
Imaging such as computed tomography angiography (CTA), magnetic resonance angiography (MRA), or duplex ultrasound confirms the diagnosis, typically showing a characteristic "hooked" or "J-shaped" appearance of the compressed celiac artery. Definitive management is surgical with laparoscopic release of the median arcuate ligament. In refractory cases, angioplasty, stenting, or vascular reconstruction may be necessary.
While the clinical scenario was further complicated in this patient by underlying intestinal malrotation, the aforementioned etiologies are considered. Recognizing anatomical variants when evaluating MALS and planning effective treatment strategies is crucial.
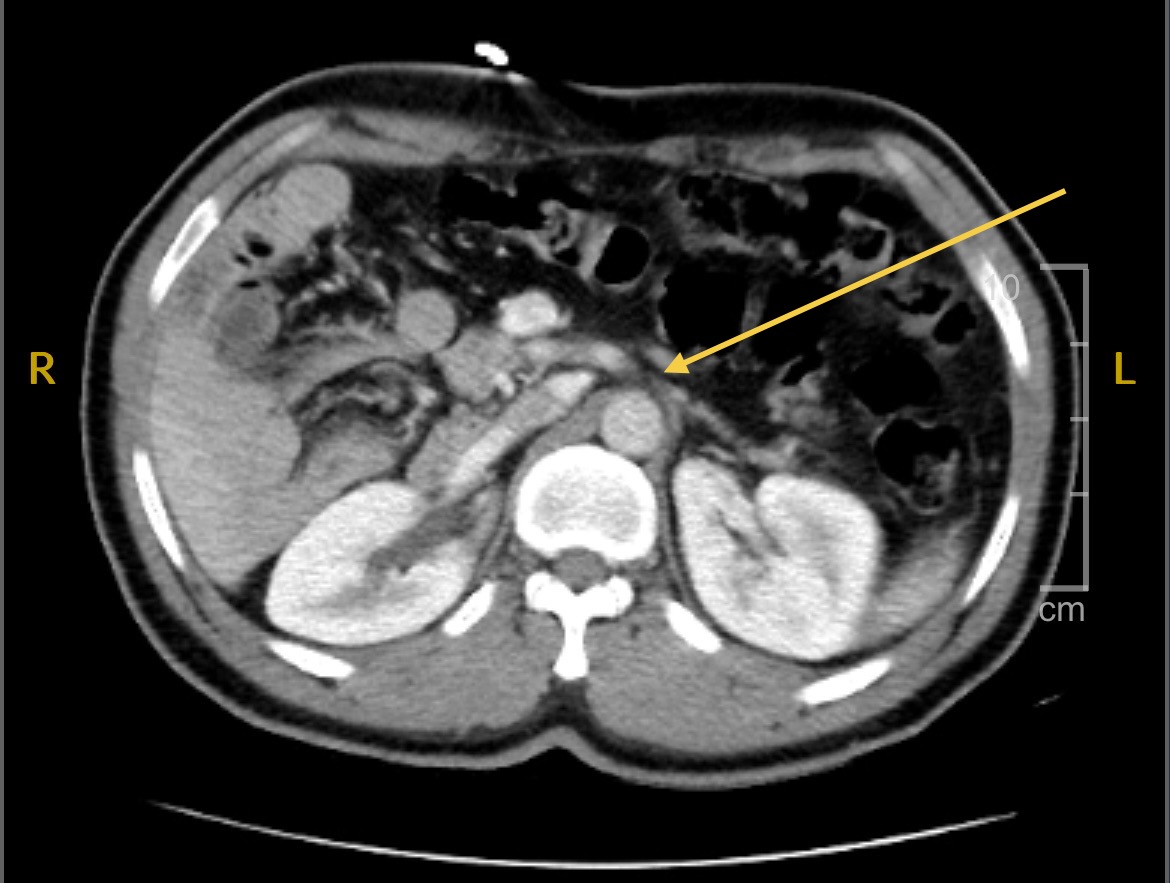
Figure: CT Abdomen/Pelvis (axial): Approximately about 70% celiac axis stenosis (indicated by yellow arrow). Malrotated bowel. Small bowel mainly in the right midabdomen.
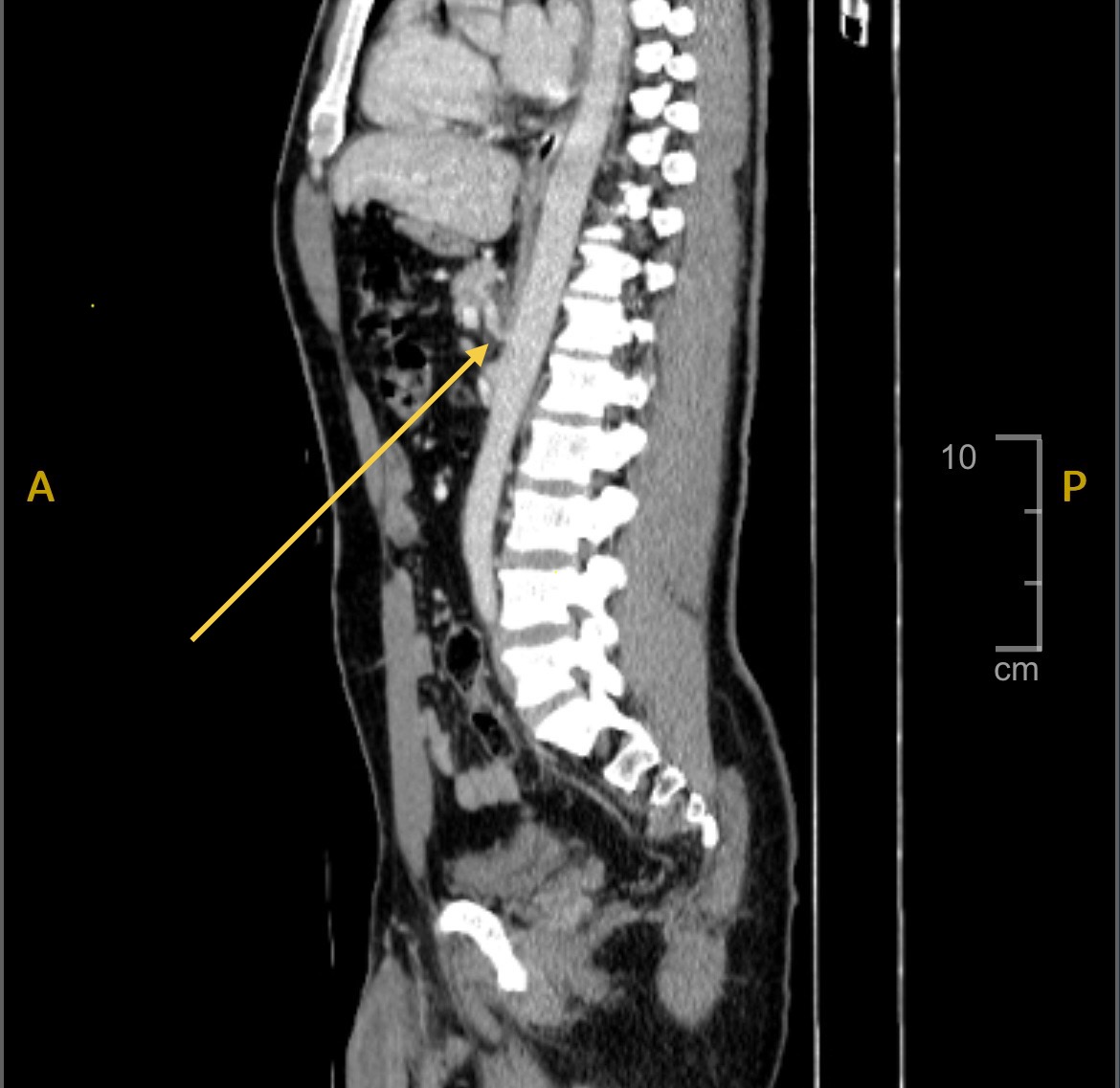
Figure: CT Abdomen/Pelvis (sagittal): Characteristic "J-shaped" or "Hooked" appearance indicating compression
Disclosures:
Panida Charnvitayapong indicated no relevant financial relationships.
Michelle Lopez Baez indicated no relevant financial relationships.
Bebika Subedi indicated no relevant financial relationships.
Shaun Isaac indicated no relevant financial relationships.
Panida Charnvitayapong, MD1, Michelle Lopez Baez, MD1, Bebika Subedi, MD1, Shaun Isaac, MD2. P6411 - A Twisted Tale: Median Arcuate Ligament Syndrome (MALS) in a Patient with Intestinal Malrotation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
