Tuesday Poster Session
Category: Stomach and Spleen
P6407 - Masquerading in the Mucosa: A Pyloric Gland Adenoma Initially Diagnosed as a Hyperplastic Polyp
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Benjamin L. Robinson, DO (he/him/his)
Atrium Health Carolinas Medical Center
Charlotte, NC
Presenting Author(s)
Benjamin L. Robinson, DO, Andrew M. Dries, MD, Carl Jacobs, MD, Baha Moshiree, MD
Atrium Health Carolinas Medical Center, Charlotte, NC
Introduction: Pyloric gland adenomas (PGAs) represent approximately 2.7% of all gastric adenomas but may progress to invasive adenocarcinoma in up to 47% of cases. We present a case of a PGA initially diagnosed as a hyperplastic polyp, underscoring the importance of accurate endoscopic and histologic evaluation of high-risk gastric polypoid lesions.
Case Description/
Methods: A 65-year-old female with gastroesophageal reflux disease presented for evaluation of persistent upper abdominal discomfort. Physical examination was notable for epigastric tenderness but was otherwise normal. Laboratory studies showed iron deficiency anemia. Her family history was significant for gastric cancer in two sisters, diagnosed in their 30s and 70s. Given her family history of gastrointestinal malignancy and her own abdominal pain, an esophagogastroduodenoscopy (EGD) was performed to rule out Helicobacter pylori (HP), peptic ulcer disease, or other etiologies. EGD revealed an 18 mm pedunculated polyp in the gastric fundus against a background of erythematous mucosa (Figure 1a). Biopsies demonstrated a gastric hyperplastic polyp without intestinal metaplasia or dysplasia, in the setting of chronic gastritis, negative for HP. Due to the polyp’s size ( >10 mm), anemia, and significant family history, the patient was referred for endoscopic mucosal resection (EMR), during which the lesion was excised using an epinephrine submucosal lift and a hot snare (Figure 1b–d). Final pathology revealed a pyloric gland adenoma without dysplasia, with complete resection and negative margins. The patient was advised to undergo surveillance EGD in one year.
Discussion: Pyloric gland adenomas are rare gastric neoplasms that are often underrecognized due to their benign-appearing endoscopic features. Consistent with previously reported cases, PGAs typically arise in the setting of chronic gastritis, most often localize to the gastric fundus, and demonstrate a predilection for female patients. They may mimic hyperplastic polyps on gross examination and superficial biopsy, making complete resection and thorough histologic evaluation essential for accurate diagnosis. Assessment of the complete glandular architecture, particularly to identify pyloric-type differentiation, is essential for distinguishing PGAs. This case highlights the importance of considering advanced endoscopic resection in patients with gastric polypoid lesions larger than 1 cm, pedunculation, or a family history of gastric malignancy, as adenomas may present deceptively.
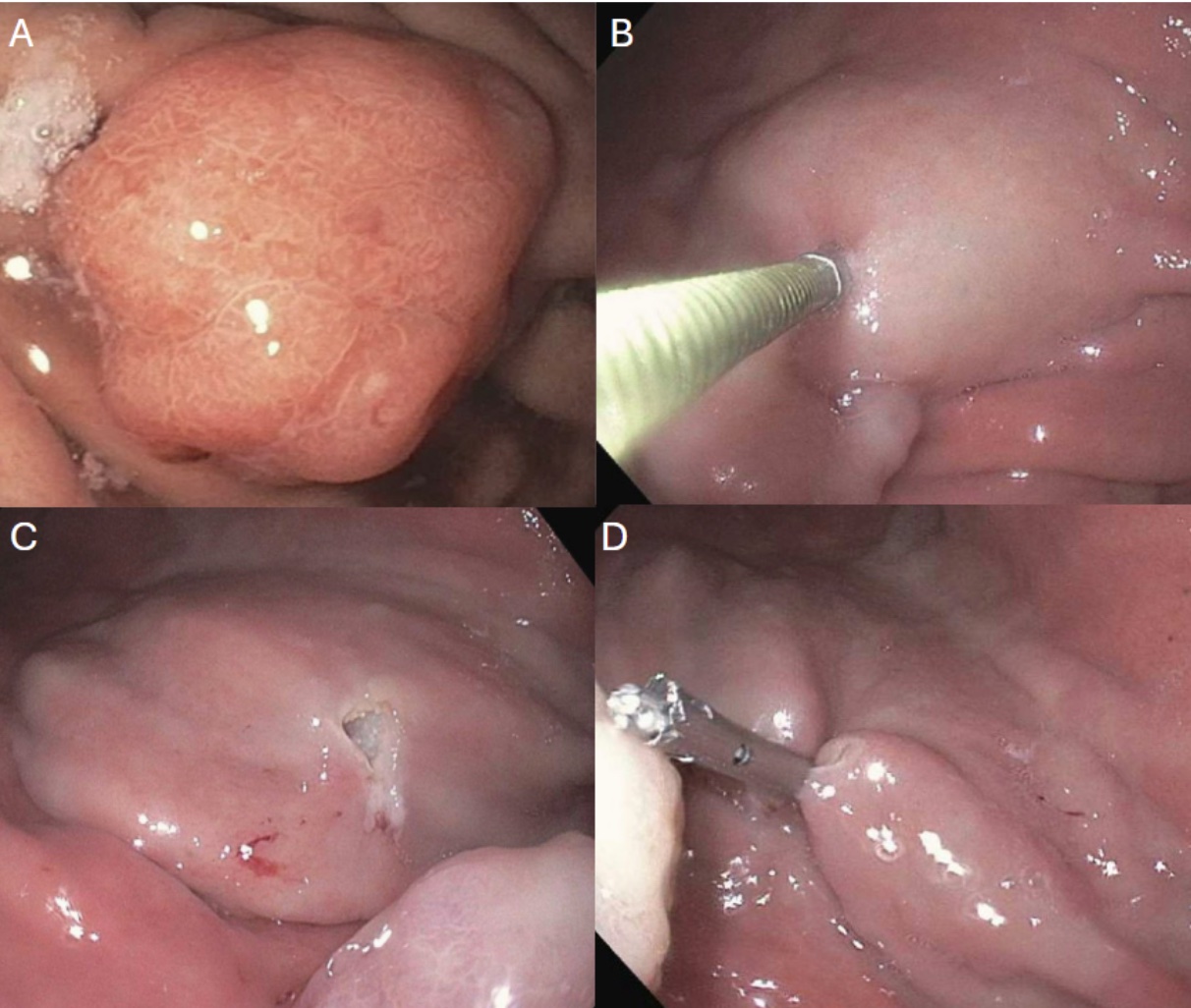
Figure: Figure 1. Initial EGD of 18 mm pedunculated polypoid lesion in the fundus of the stomach (A). Endoscopic mucosal resection using submucosal lift with injection of 4 mL epinephrine (B), complete resection using a hot snare (C), placement of a hemostatic clip at the resection site (D).
Disclosures:
Benjamin Robinson indicated no relevant financial relationships.
Andrew Dries indicated no relevant financial relationships.
Carl Jacobs indicated no relevant financial relationships.
Baha Moshiree indicated no relevant financial relationships.
Benjamin L. Robinson, DO, Andrew M. Dries, MD, Carl Jacobs, MD, Baha Moshiree, MD. P6407 - Masquerading in the Mucosa: A Pyloric Gland Adenoma Initially Diagnosed as a Hyperplastic Polyp, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Atrium Health Carolinas Medical Center, Charlotte, NC
Introduction: Pyloric gland adenomas (PGAs) represent approximately 2.7% of all gastric adenomas but may progress to invasive adenocarcinoma in up to 47% of cases. We present a case of a PGA initially diagnosed as a hyperplastic polyp, underscoring the importance of accurate endoscopic and histologic evaluation of high-risk gastric polypoid lesions.
Case Description/
Methods: A 65-year-old female with gastroesophageal reflux disease presented for evaluation of persistent upper abdominal discomfort. Physical examination was notable for epigastric tenderness but was otherwise normal. Laboratory studies showed iron deficiency anemia. Her family history was significant for gastric cancer in two sisters, diagnosed in their 30s and 70s. Given her family history of gastrointestinal malignancy and her own abdominal pain, an esophagogastroduodenoscopy (EGD) was performed to rule out Helicobacter pylori (HP), peptic ulcer disease, or other etiologies. EGD revealed an 18 mm pedunculated polyp in the gastric fundus against a background of erythematous mucosa (Figure 1a). Biopsies demonstrated a gastric hyperplastic polyp without intestinal metaplasia or dysplasia, in the setting of chronic gastritis, negative for HP. Due to the polyp’s size ( >10 mm), anemia, and significant family history, the patient was referred for endoscopic mucosal resection (EMR), during which the lesion was excised using an epinephrine submucosal lift and a hot snare (Figure 1b–d). Final pathology revealed a pyloric gland adenoma without dysplasia, with complete resection and negative margins. The patient was advised to undergo surveillance EGD in one year.
Discussion: Pyloric gland adenomas are rare gastric neoplasms that are often underrecognized due to their benign-appearing endoscopic features. Consistent with previously reported cases, PGAs typically arise in the setting of chronic gastritis, most often localize to the gastric fundus, and demonstrate a predilection for female patients. They may mimic hyperplastic polyps on gross examination and superficial biopsy, making complete resection and thorough histologic evaluation essential for accurate diagnosis. Assessment of the complete glandular architecture, particularly to identify pyloric-type differentiation, is essential for distinguishing PGAs. This case highlights the importance of considering advanced endoscopic resection in patients with gastric polypoid lesions larger than 1 cm, pedunculation, or a family history of gastric malignancy, as adenomas may present deceptively.
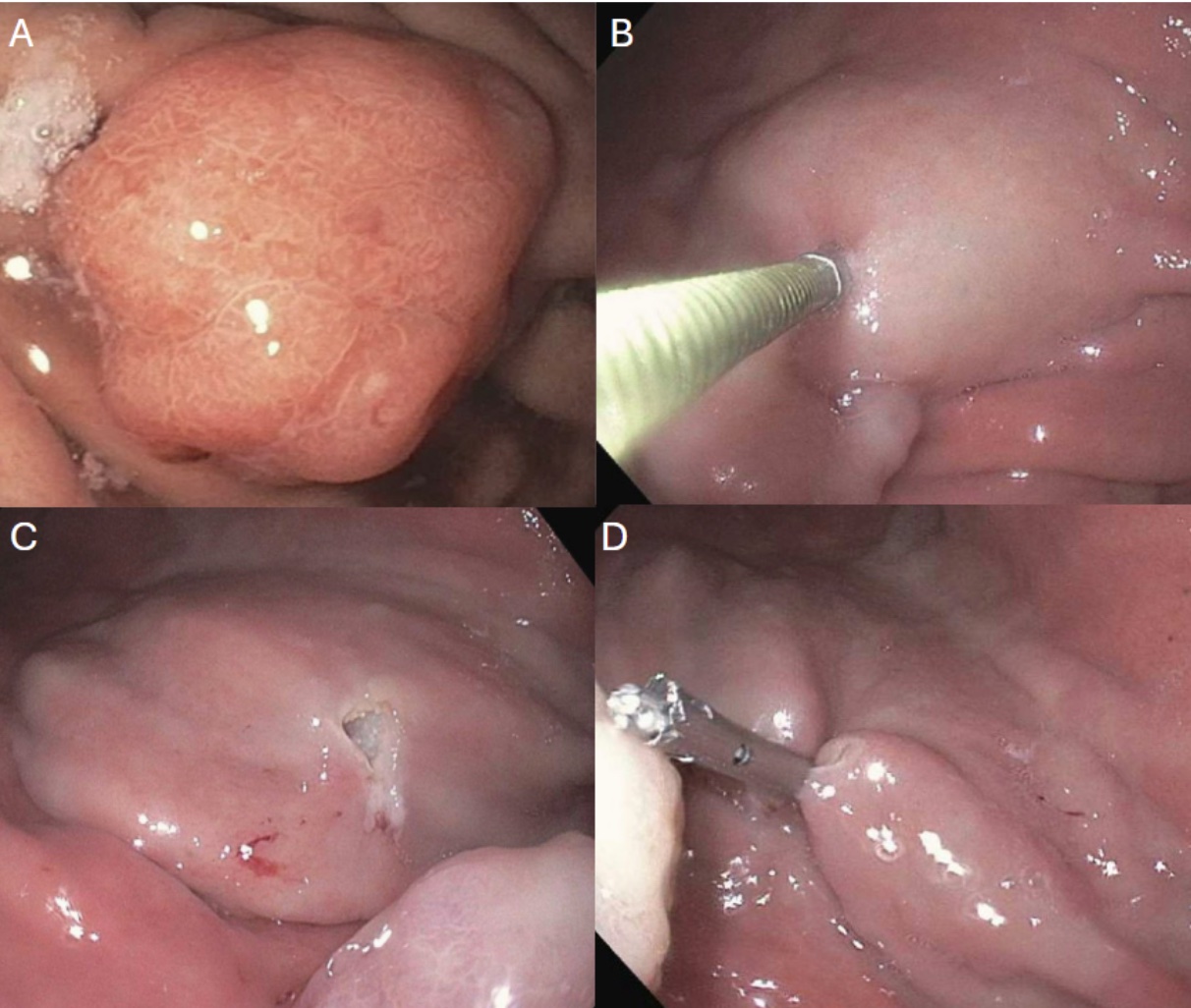
Figure: Figure 1. Initial EGD of 18 mm pedunculated polypoid lesion in the fundus of the stomach (A). Endoscopic mucosal resection using submucosal lift with injection of 4 mL epinephrine (B), complete resection using a hot snare (C), placement of a hemostatic clip at the resection site (D).
Disclosures:
Benjamin Robinson indicated no relevant financial relationships.
Andrew Dries indicated no relevant financial relationships.
Carl Jacobs indicated no relevant financial relationships.
Baha Moshiree indicated no relevant financial relationships.
Benjamin L. Robinson, DO, Andrew M. Dries, MD, Carl Jacobs, MD, Baha Moshiree, MD. P6407 - Masquerading in the Mucosa: A Pyloric Gland Adenoma Initially Diagnosed as a Hyperplastic Polyp, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
