Tuesday Poster Session
Category: Stomach and Spleen
P6403 - A Case of Pyloric Dysfunction Mimicking Inflammatory Bowel Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- RS
Rajanbir Singh, MD
Southern Illinois University
Springfield, IL
Presenting Author(s)
Rajanbir Singh, MD1, Sophia Haroon. Dar, MD1, Yin Chan, MD2, Phillip Gu, MD3, Lim Jane, MD3
1Southern Illinois University, Springfield, IL; 2Cedars-Sinai Medical Center, Beverly Hills, CA; 3Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Pyloric dysfunction (PD) is a rare gastric motility disorder characterized by abnormal contractions of the pyloric sphincter, often resulting in delayed gastric emptying and severe upper gastrointestinal (GI) symptoms. Its clinical presentation can mimic inflammatory bowel disease (IBD) due to overlapping symptoms of chronic abdominal pain, nausea, vomiting, and unintentional weight loss. Thus, it becomes challenging to diagnose, especially in young patients with a strong family history of IBD. We present a case of a young male whose symptoms were initially concerning for IBD, but he was ultimately diagnosed with PD through advanced motility testing.
Case Description/
Methods: A 27-year-old White male with a family history of Crohn’s disease, in his father and two siblings, was referred to the GI motility clinic for nausea, vomiting, abdominal pain, and unintentional weight loss for 5 years, leading to total parenteral nutrition for severe oral intolerance. Despite his strong family history of Crohn’s disease, extensive diagnostic evaluations, including esophagogastroduodenoscopy (EGD), double-balloon enteroscopy (DBE), magnetic resonance enterography (MRE), and capsule endoscopy results were non-specific, revealing punctuate ulcers and erythema in the small bowel with normal histologic findings. Empiric treatment for presumed IBD with corticosteroids, adalimumab, and ustekinumab was ineffective. Further evaluation with a gastric emptying breath test was normal. Antroduodenal manometry revealed pyloric contractions, and functional lumen imaging probe (FLIP) of the pylorus showed reduced pyloric distensibility with a distensibility index of 4.5 mm2/mmHg at 40 mL and 3.4 mm2/mmHg at 50 mL, consistent with pyloric dysfunction. The patient experienced complete symptom resolution after botulinum toxin injection to the pylorus. He later underwent successful gastric peroral endoscopic myotomy (G-POEM) with resolution of his symptoms.
Discussion: Pyloric dysfunction (PD) may present a diagnostic challenge, particularly in young patients with overlapping symptoms and a strong family history of inflammatory bowel disease (IBD). Despite inconclusive conventional testing, advanced motility evaluation with antroduodenal manometry and pyloric EndoFLIP was instrumental in uncovering a rare gastric motility disorder in this patient. This case highlights the importance of considering PD in the differential diagnosis of patients with persistent upper GI symptoms, even when gastric emptying studies are normal.
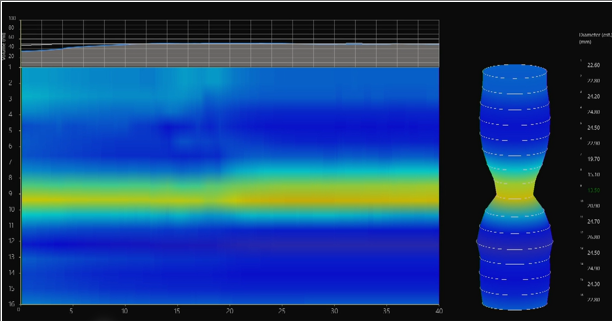
Figure: Pyloric EndoFLIP demonstrating reduced pyloric distensibility

Figure: Antroduodenal manometry demonstrating robust pyloric contractions associated with abdominal pain episodes
Disclosures:
Rajanbir Singh indicated no relevant financial relationships.
Sophia Dar indicated no relevant financial relationships.
Yin Chan indicated no relevant financial relationships.
Phillip Gu indicated no relevant financial relationships.
Lim Jane indicated no relevant financial relationships.
Rajanbir Singh, MD1, Sophia Haroon. Dar, MD1, Yin Chan, MD2, Phillip Gu, MD3, Lim Jane, MD3. P6403 - A Case of Pyloric Dysfunction Mimicking Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Southern Illinois University, Springfield, IL; 2Cedars-Sinai Medical Center, Beverly Hills, CA; 3Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Pyloric dysfunction (PD) is a rare gastric motility disorder characterized by abnormal contractions of the pyloric sphincter, often resulting in delayed gastric emptying and severe upper gastrointestinal (GI) symptoms. Its clinical presentation can mimic inflammatory bowel disease (IBD) due to overlapping symptoms of chronic abdominal pain, nausea, vomiting, and unintentional weight loss. Thus, it becomes challenging to diagnose, especially in young patients with a strong family history of IBD. We present a case of a young male whose symptoms were initially concerning for IBD, but he was ultimately diagnosed with PD through advanced motility testing.
Case Description/
Methods: A 27-year-old White male with a family history of Crohn’s disease, in his father and two siblings, was referred to the GI motility clinic for nausea, vomiting, abdominal pain, and unintentional weight loss for 5 years, leading to total parenteral nutrition for severe oral intolerance. Despite his strong family history of Crohn’s disease, extensive diagnostic evaluations, including esophagogastroduodenoscopy (EGD), double-balloon enteroscopy (DBE), magnetic resonance enterography (MRE), and capsule endoscopy results were non-specific, revealing punctuate ulcers and erythema in the small bowel with normal histologic findings. Empiric treatment for presumed IBD with corticosteroids, adalimumab, and ustekinumab was ineffective. Further evaluation with a gastric emptying breath test was normal. Antroduodenal manometry revealed pyloric contractions, and functional lumen imaging probe (FLIP) of the pylorus showed reduced pyloric distensibility with a distensibility index of 4.5 mm2/mmHg at 40 mL and 3.4 mm2/mmHg at 50 mL, consistent with pyloric dysfunction. The patient experienced complete symptom resolution after botulinum toxin injection to the pylorus. He later underwent successful gastric peroral endoscopic myotomy (G-POEM) with resolution of his symptoms.
Discussion: Pyloric dysfunction (PD) may present a diagnostic challenge, particularly in young patients with overlapping symptoms and a strong family history of inflammatory bowel disease (IBD). Despite inconclusive conventional testing, advanced motility evaluation with antroduodenal manometry and pyloric EndoFLIP was instrumental in uncovering a rare gastric motility disorder in this patient. This case highlights the importance of considering PD in the differential diagnosis of patients with persistent upper GI symptoms, even when gastric emptying studies are normal.
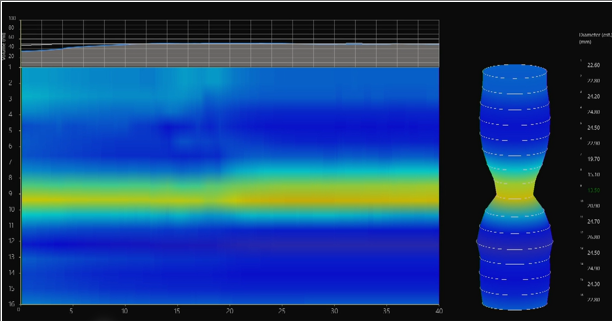
Figure: Pyloric EndoFLIP demonstrating reduced pyloric distensibility

Figure: Antroduodenal manometry demonstrating robust pyloric contractions associated with abdominal pain episodes
Disclosures:
Rajanbir Singh indicated no relevant financial relationships.
Sophia Dar indicated no relevant financial relationships.
Yin Chan indicated no relevant financial relationships.
Phillip Gu indicated no relevant financial relationships.
Lim Jane indicated no relevant financial relationships.
Rajanbir Singh, MD1, Sophia Haroon. Dar, MD1, Yin Chan, MD2, Phillip Gu, MD3, Lim Jane, MD3. P6403 - A Case of Pyloric Dysfunction Mimicking Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
