Tuesday Poster Session
Category: Stomach and Spleen
Acquired Double Pylorus as a Sequela of NSAID Use, Alcohol, and <i>Helicobacter pylori</i>
P6395 - Acquired Double Pylorus as a Sequela of NSAID Use, Alcohol, and Helicobacter pylori
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Anveet Janwadkar, MD
Tulane School of Medicine
New Orleans, LA
Presenting Author(s)
Anveet Janwadkar, MD1, Husayn F. Ramji, MD2, Stephanie Mrowczynski, BS, MD1, Yucel Aydin, MD3, John M. Bloch, MD1
1Tulane School of Medicine, New Orleans, LA; 2Tulane University School of Medicine, New Orleans, LA; 3Tulane University, New Orleans, LA
Introduction: Double pylorus, or gastroduodenal fistula, is a rare, acquired complication of peptic ulcer disease (PUD) involving an additional tract between the distal stomach and the duodenal bulb. This condition is most often associated with Helicobacter pylori infection, chronic NSAID use, and other contributors to impaired mucosal healing. Its incidence ranges from 0.001% to 0.4% on endoscopy, and it is typically discovered incidentally, though it may occasionally present with bleeding.
Case Description/
Methods: A 64-year-old man with hypertension, hyperlipidemia, and chronic alcohol use disorder presented with syncope and hematemesis. He reported several days of melena and postprandial epigastric discomfort relieved by food. He endorsed frequent ibuprofen use and daily alcohol intake. On admission, he was hypotensive and tachycardic, with hemoglobin 7.3 g/dL. He received IV fluids, packed red blood cell transfusion, and IV pantoprazole. Upper endoscopy revealed a large cratered pre-pyloric ulcer with a secondary opening that allowed passage of the scope into the duodenal bulb, consistent with a gastroduodenal fistula. There was no active bleeding or stigmata. Gastric biopsies showed chronic active gastritis with H. pylori identified on immunohistochemistry. He was discharged on bismuth-based quadruple therapy and PPI, with a plan for repeat endoscopy in eight weeks.
Discussion: This case illustrates a classic but uncommon complication of PUD resulting from synergistic mucosal injury due to H. pylori, NSAID use, and alcohol. Double pylorus often signifies chronic ulceration and impaired healing but is frequently asymptomatic. Its recognition should prompt eradication of risk factors and close endoscopic follow-up. Although typically managed conservatively, endoscopic or surgical intervention may be necessary if complicated by bleeding, obstruction, or refractory symptoms. Awareness of this finding is critical to guide appropriate therapy and prevent recurrence.

Figure: Figure 1. Endoscopic image of the pylorus with presence of a gastroduodenal fistula (double pylorus)
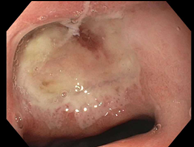
Figure: Figure 2. Endoscopic image of the pre-pyloric region demonstrating a large cratered gastric ulcer with surrounding fibrinous exudate and a gastroduodenal fistula (double pylorus) seen at the inferior margin
Disclosures:
Anveet Janwadkar indicated no relevant financial relationships.
Husayn Ramji indicated no relevant financial relationships.
Stephanie Mrowczynski indicated no relevant financial relationships.
Yucel Aydin indicated no relevant financial relationships.
John Bloch indicated no relevant financial relationships.
Anveet Janwadkar, MD1, Husayn F. Ramji, MD2, Stephanie Mrowczynski, BS, MD1, Yucel Aydin, MD3, John M. Bloch, MD1. P6395 - Acquired Double Pylorus as a Sequela of NSAID Use, Alcohol, and <i>Helicobacter pylori</i>, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Tulane School of Medicine, New Orleans, LA; 2Tulane University School of Medicine, New Orleans, LA; 3Tulane University, New Orleans, LA
Introduction: Double pylorus, or gastroduodenal fistula, is a rare, acquired complication of peptic ulcer disease (PUD) involving an additional tract between the distal stomach and the duodenal bulb. This condition is most often associated with Helicobacter pylori infection, chronic NSAID use, and other contributors to impaired mucosal healing. Its incidence ranges from 0.001% to 0.4% on endoscopy, and it is typically discovered incidentally, though it may occasionally present with bleeding.
Case Description/
Methods: A 64-year-old man with hypertension, hyperlipidemia, and chronic alcohol use disorder presented with syncope and hematemesis. He reported several days of melena and postprandial epigastric discomfort relieved by food. He endorsed frequent ibuprofen use and daily alcohol intake. On admission, he was hypotensive and tachycardic, with hemoglobin 7.3 g/dL. He received IV fluids, packed red blood cell transfusion, and IV pantoprazole. Upper endoscopy revealed a large cratered pre-pyloric ulcer with a secondary opening that allowed passage of the scope into the duodenal bulb, consistent with a gastroduodenal fistula. There was no active bleeding or stigmata. Gastric biopsies showed chronic active gastritis with H. pylori identified on immunohistochemistry. He was discharged on bismuth-based quadruple therapy and PPI, with a plan for repeat endoscopy in eight weeks.
Discussion: This case illustrates a classic but uncommon complication of PUD resulting from synergistic mucosal injury due to H. pylori, NSAID use, and alcohol. Double pylorus often signifies chronic ulceration and impaired healing but is frequently asymptomatic. Its recognition should prompt eradication of risk factors and close endoscopic follow-up. Although typically managed conservatively, endoscopic or surgical intervention may be necessary if complicated by bleeding, obstruction, or refractory symptoms. Awareness of this finding is critical to guide appropriate therapy and prevent recurrence.

Figure: Figure 1. Endoscopic image of the pylorus with presence of a gastroduodenal fistula (double pylorus)
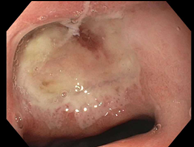
Figure: Figure 2. Endoscopic image of the pre-pyloric region demonstrating a large cratered gastric ulcer with surrounding fibrinous exudate and a gastroduodenal fistula (double pylorus) seen at the inferior margin
Disclosures:
Anveet Janwadkar indicated no relevant financial relationships.
Husayn Ramji indicated no relevant financial relationships.
Stephanie Mrowczynski indicated no relevant financial relationships.
Yucel Aydin indicated no relevant financial relationships.
John Bloch indicated no relevant financial relationships.
Anveet Janwadkar, MD1, Husayn F. Ramji, MD2, Stephanie Mrowczynski, BS, MD1, Yucel Aydin, MD3, John M. Bloch, MD1. P6395 - Acquired Double Pylorus as a Sequela of NSAID Use, Alcohol, and <i>Helicobacter pylori</i>, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
