Tuesday Poster Session
Category: Stomach and Spleen
P6391 - Successful Treatment of a Chronic Gastric Phytobezoar Using Effervescent Therapy: A Case Report
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- HM
Himani Mongia, MBBS (she/her/hers)
The Wright Center for Graduate Medical Education
Scranton, PA
Presenting Author(s)
Himani Mongia, MBBS1, Tejas Nikumbh, MD2, Udit Asija, MD3, Keerthy Gopalakrishnan, MD1, Jyoti Yadav, MD1, Sunny Kumar, MD4, Peter Iskander, MD1, Masoud Firouzi, MD5
1The Wright Center for Graduate Medical Education, Scranton, PA; 2The Wright Center for Graduate Medical Education, Dunmore, PA; 3The Wright Center for Graduate Medical Education, Throop, PA; 4Wright Center for Graduate Medical Education, Scranton, PA; 5Wilkes Barre VA Medical Center, Wilkes-Barre, PA
Introduction: Bezoars are aggregates of indigestible material within the gastrointestinal tract, commonly presenting with nonspecific symptoms such as abdominal pain, nausea, and loss of appetite. Risk factors include previous gastric surgery, diabetes mellitus with gastroparesis, persimmon ingestion, poor mastication, and certain psychiatric conditions. Bezoars can be managed through dissolution, mechanical fragmentation, or endoscopic retrieval. Among dissolution agents, carbonated beverages such as Coca-Cola ® have been reported as effective in a few case reports with modes of delivery including nasogastric lavage, oral ingestion over several days, or endoscopic injection. We present a case of a chronic, large bezoar successfully treated with oral Coca-Cola administration.
Case Description/
Methods: A 64-year-old female with a history of asthma, hirsutism, hypertension, morbid obesity, hyperlipidemia, cyclothymia, and breast cancer status post partial right mastectomy was under evaluation for weight management and eating disorder. She reported intermittent dysphagia for one year warranting gastroenterology consultation. One year prior non-contrast CT thorax showed high-density material in the stomach, previously presumed to be residual tablets. Follow-up esophagogastroduodenoscopy (EGD) was performed revealing an unremarkable esophagus but a gastric phytobezoar occupying >50% of gastric volume obscuring mucosal visualization and further leading to premature procedure termination. The patient was instructed to ingest 3 liters of carbonated soda over 3-6 hours. Repeat EGD the following day showed complete resolution of the bezoar, with no residual material in the stomach.
Discussion: This case highlights the effectiveness of carbonated beverages such as Coca-Cola for the non-invasive management of a large, chronic gastric phytobezoar. While multiple treatment strategies exist, the use of carbonated beverages remains a safe, accessible, and cost-effective option. Dissolution with Coca-Cola is proposed to work through mucolytic effects as well as weak acid (H2CO3/H3PO4) based fiber matrix disruption. This approach may help avoid invasive interventions or aid in endoscopic interventions by making the bezoar malleable to removal. Continued awareness and documentation of such treatment successes are important to guide future management strategies.
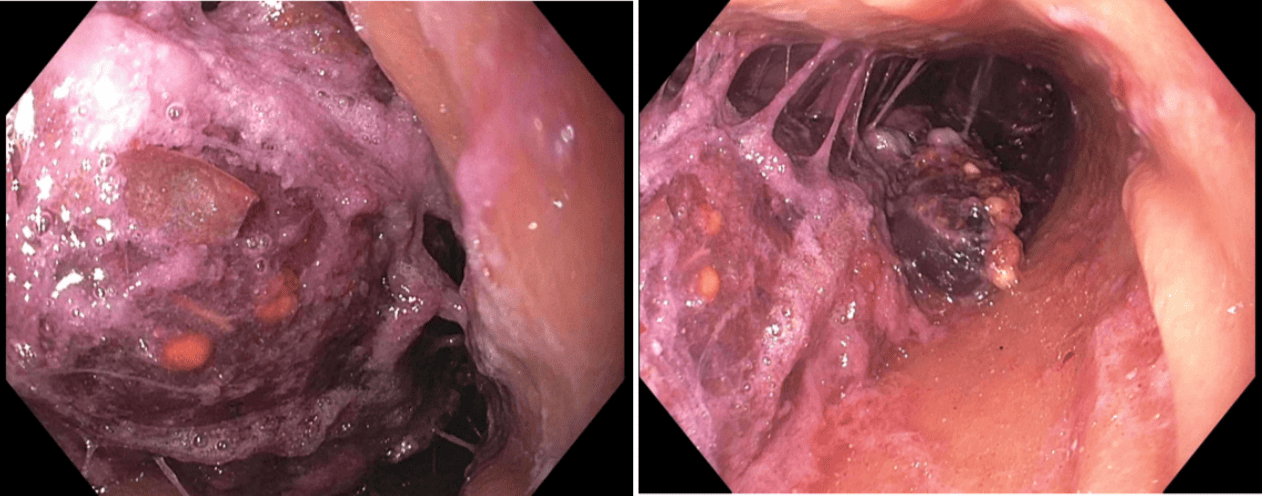
Figure: Initial Endoscopy showing Chronic Gastric Phytobezoar
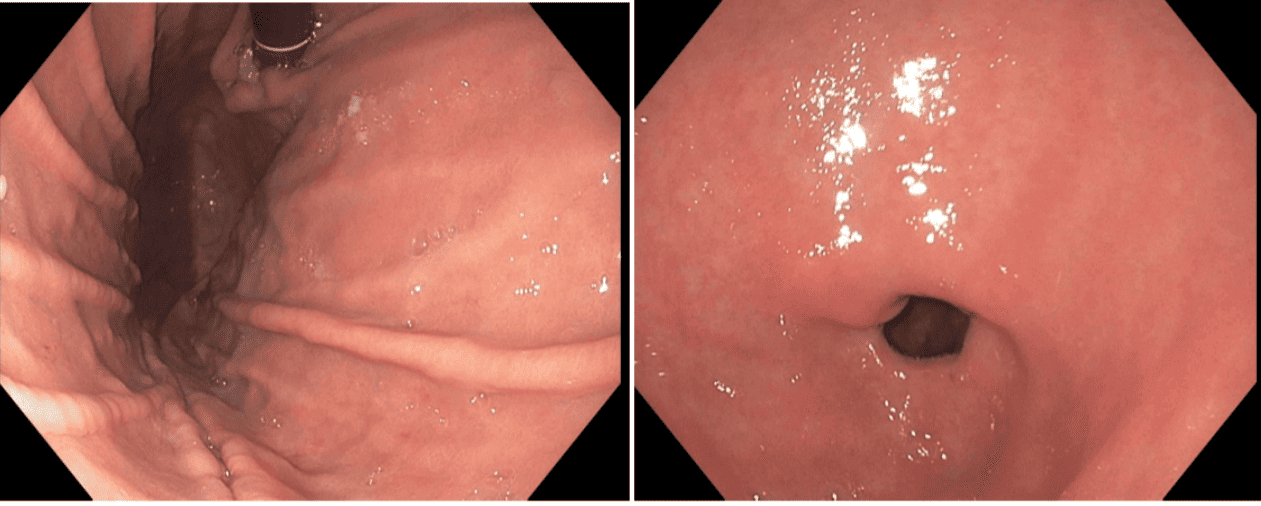
Figure: Follow-up Endoscopy showing no residual material in stomach
Disclosures:
Himani Mongia indicated no relevant financial relationships.
Tejas Nikumbh indicated no relevant financial relationships.
Udit Asija indicated no relevant financial relationships.
Keerthy Gopalakrishnan indicated no relevant financial relationships.
Jyoti Yadav indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Peter Iskander indicated no relevant financial relationships.
Masoud Firouzi indicated no relevant financial relationships.
Himani Mongia, MBBS1, Tejas Nikumbh, MD2, Udit Asija, MD3, Keerthy Gopalakrishnan, MD1, Jyoti Yadav, MD1, Sunny Kumar, MD4, Peter Iskander, MD1, Masoud Firouzi, MD5. P6391 - Successful Treatment of a Chronic Gastric Phytobezoar Using Effervescent Therapy: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1The Wright Center for Graduate Medical Education, Scranton, PA; 2The Wright Center for Graduate Medical Education, Dunmore, PA; 3The Wright Center for Graduate Medical Education, Throop, PA; 4Wright Center for Graduate Medical Education, Scranton, PA; 5Wilkes Barre VA Medical Center, Wilkes-Barre, PA
Introduction: Bezoars are aggregates of indigestible material within the gastrointestinal tract, commonly presenting with nonspecific symptoms such as abdominal pain, nausea, and loss of appetite. Risk factors include previous gastric surgery, diabetes mellitus with gastroparesis, persimmon ingestion, poor mastication, and certain psychiatric conditions. Bezoars can be managed through dissolution, mechanical fragmentation, or endoscopic retrieval. Among dissolution agents, carbonated beverages such as Coca-Cola ® have been reported as effective in a few case reports with modes of delivery including nasogastric lavage, oral ingestion over several days, or endoscopic injection. We present a case of a chronic, large bezoar successfully treated with oral Coca-Cola administration.
Case Description/
Methods: A 64-year-old female with a history of asthma, hirsutism, hypertension, morbid obesity, hyperlipidemia, cyclothymia, and breast cancer status post partial right mastectomy was under evaluation for weight management and eating disorder. She reported intermittent dysphagia for one year warranting gastroenterology consultation. One year prior non-contrast CT thorax showed high-density material in the stomach, previously presumed to be residual tablets. Follow-up esophagogastroduodenoscopy (EGD) was performed revealing an unremarkable esophagus but a gastric phytobezoar occupying >50% of gastric volume obscuring mucosal visualization and further leading to premature procedure termination. The patient was instructed to ingest 3 liters of carbonated soda over 3-6 hours. Repeat EGD the following day showed complete resolution of the bezoar, with no residual material in the stomach.
Discussion: This case highlights the effectiveness of carbonated beverages such as Coca-Cola for the non-invasive management of a large, chronic gastric phytobezoar. While multiple treatment strategies exist, the use of carbonated beverages remains a safe, accessible, and cost-effective option. Dissolution with Coca-Cola is proposed to work through mucolytic effects as well as weak acid (H2CO3/H3PO4) based fiber matrix disruption. This approach may help avoid invasive interventions or aid in endoscopic interventions by making the bezoar malleable to removal. Continued awareness and documentation of such treatment successes are important to guide future management strategies.
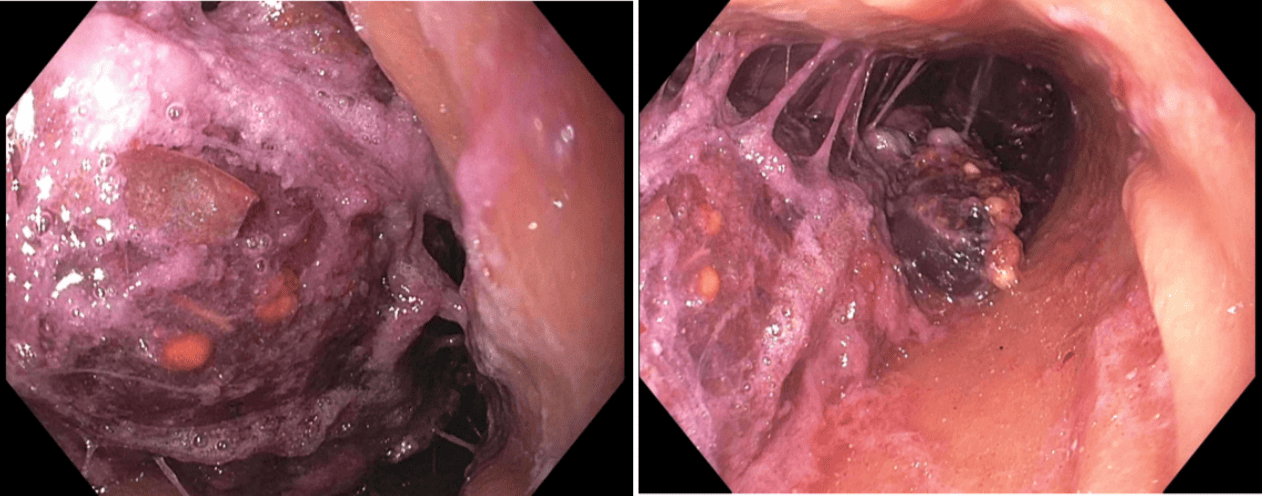
Figure: Initial Endoscopy showing Chronic Gastric Phytobezoar
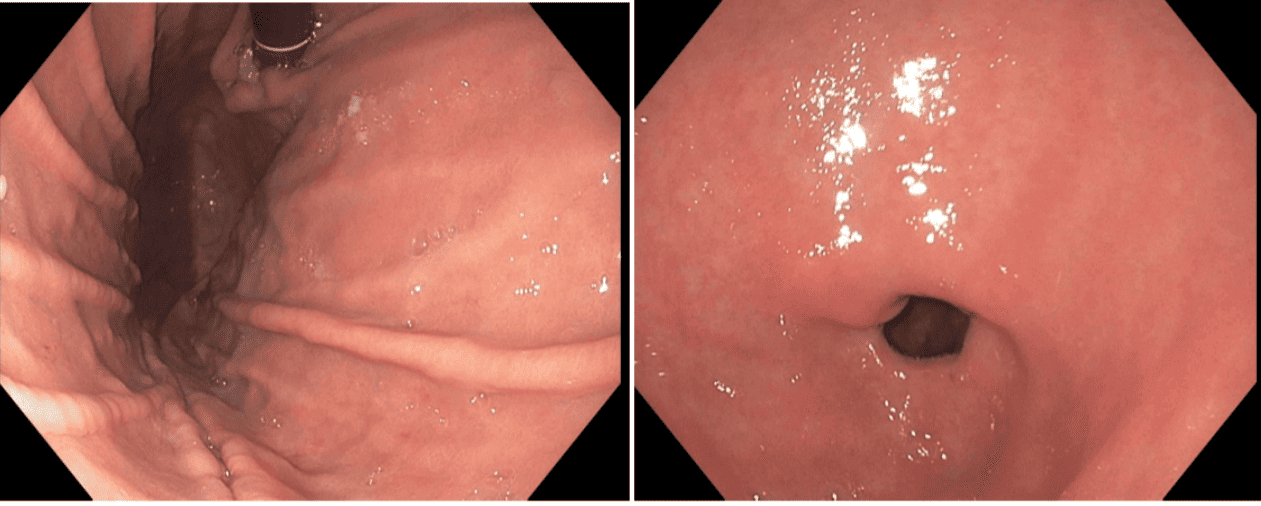
Figure: Follow-up Endoscopy showing no residual material in stomach
Disclosures:
Himani Mongia indicated no relevant financial relationships.
Tejas Nikumbh indicated no relevant financial relationships.
Udit Asija indicated no relevant financial relationships.
Keerthy Gopalakrishnan indicated no relevant financial relationships.
Jyoti Yadav indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Peter Iskander indicated no relevant financial relationships.
Masoud Firouzi indicated no relevant financial relationships.
Himani Mongia, MBBS1, Tejas Nikumbh, MD2, Udit Asija, MD3, Keerthy Gopalakrishnan, MD1, Jyoti Yadav, MD1, Sunny Kumar, MD4, Peter Iskander, MD1, Masoud Firouzi, MD5. P6391 - Successful Treatment of a Chronic Gastric Phytobezoar Using Effervescent Therapy: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

