Tuesday Poster Session
Category: Stomach and Spleen
P6388 - Gastric Ulcer Presenting as a Double-Channel Pylorus: Could This Be Eosinophilic Gastritis?
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
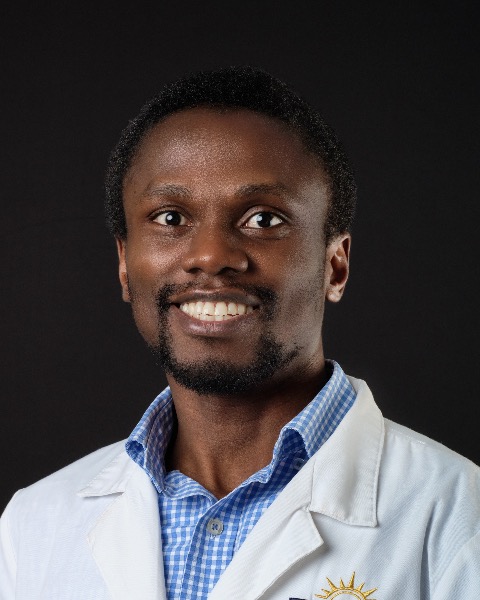
Kwabena Asafo-Agyei, MD
Medical College of Georgia at Augusta University
Evans, GA
Presenting Author(s)
Kwabena Asafo-Agyei, MD1, Angela Barnes, MD2, Lakshmi Vemavarapu, MD3, Leonard Little, MD4
1Medical College of Georgia at Augusta University, Evans, GA; 2Medical College of Georgia at Augusta University, Augusta, GA; 3VA-Augusta, Augusta, GA; 4VA AUGUSTA, Augusta, GA
Introduction: Peptic ulcer disease is a common gastrointestinal disorder characterized by ulceration in the stomach & duodenum. However, during endoscopic and histological evaluation, the disease may mimic eosinophilic gastritis, checkpoint inhibitor-induced ulcer disease, ischemia, & other conditions. We present a case of a double-channel pylorus from peptic ulcer disease, which was initially suspected to be from eosinophilic gastritis.
Case Description/
Methods: A 57-year-old gentleman was referred for esophagogastroduodenoscopy (EGD) after undergoing a computed tomography (CT) scan of the abdomen and pelvis with intravenous contrast, which revealed prominent circumferential wall thickening involving the peripyloric region of the stomach, with fat stranding & multiple enlarged perigastric lymph nodes. During evaluation, the patient endorsed multiple episodes of nausea and vomiting, upper quadrant abdominal pain over the last two months, & 30 pounds of weight loss. At endoscopy, a large, deep prepyloric ulcer approximately 3 cm was observed, with a clean base, borderline extension to the bulb, leading to a protruding prepyloric deformity (Fig. 1),& granular mucosa changes in the stomach. Multiple biopsies were obtained from the edge of the ulcer. Histopathology revealed gastric mucosa with ulceration and mixed inflammation characterized by increased eosinophils (up to 105/HPF), with no evidence of malignancy, & a negative H. pylori stain. Gastric biopsies showed increased eosinophils, up to 23/HPF, & duodenal mucosa with only focal erosions. The patient was started on proton pump inhibitors twice daily. A repeat EGD revealed a two-channel opening into the duodenal bulb. The previous ulcer had formed in the post-pyloric channel, extending into the duodenal bulb with healed margins. (Fig. 2) Upon discussion with the pathologist, the repeat biopsies revealed healed ulcers & no eosinophilic infiltration, indicating that eosinophilia was likely a reactive response. Consequently, the possibility of eosinophilic gastritis was low, but peptic ulcer disease was more likely.
Discussion: This case highlights the importance of a multidisciplinary approach in managing patients with complex findings during endoscopy & histology. Eosinophilic gastritis exhibits nonspecific endoscopic findings, including nodular and polypoid mucosa, and, in rare cases, deep ulceration, and gastric eosinophilia is greater than 30/HPF. Discussion with a pathologist is essential when the diagnosis is in question, as treatment modalities differ.
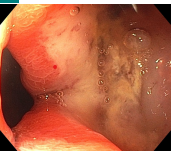
Figure: Double Channel Pylorus (Fig.2)
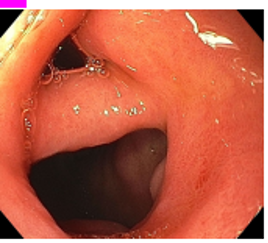
Figure: Pyloric ulcer (Fig.1)
Disclosures:
Kwabena Asafo-Agyei indicated no relevant financial relationships.
Angela Barnes indicated no relevant financial relationships.
Lakshmi Vemavarapu indicated no relevant financial relationships.
Leonard Little indicated no relevant financial relationships.
Kwabena Asafo-Agyei, MD1, Angela Barnes, MD2, Lakshmi Vemavarapu, MD3, Leonard Little, MD4. P6388 - Gastric Ulcer Presenting as a Double-Channel Pylorus: Could This Be Eosinophilic Gastritis?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Medical College of Georgia at Augusta University, Evans, GA; 2Medical College of Georgia at Augusta University, Augusta, GA; 3VA-Augusta, Augusta, GA; 4VA AUGUSTA, Augusta, GA
Introduction: Peptic ulcer disease is a common gastrointestinal disorder characterized by ulceration in the stomach & duodenum. However, during endoscopic and histological evaluation, the disease may mimic eosinophilic gastritis, checkpoint inhibitor-induced ulcer disease, ischemia, & other conditions. We present a case of a double-channel pylorus from peptic ulcer disease, which was initially suspected to be from eosinophilic gastritis.
Case Description/
Methods: A 57-year-old gentleman was referred for esophagogastroduodenoscopy (EGD) after undergoing a computed tomography (CT) scan of the abdomen and pelvis with intravenous contrast, which revealed prominent circumferential wall thickening involving the peripyloric region of the stomach, with fat stranding & multiple enlarged perigastric lymph nodes. During evaluation, the patient endorsed multiple episodes of nausea and vomiting, upper quadrant abdominal pain over the last two months, & 30 pounds of weight loss. At endoscopy, a large, deep prepyloric ulcer approximately 3 cm was observed, with a clean base, borderline extension to the bulb, leading to a protruding prepyloric deformity (Fig. 1),& granular mucosa changes in the stomach. Multiple biopsies were obtained from the edge of the ulcer. Histopathology revealed gastric mucosa with ulceration and mixed inflammation characterized by increased eosinophils (up to 105/HPF), with no evidence of malignancy, & a negative H. pylori stain. Gastric biopsies showed increased eosinophils, up to 23/HPF, & duodenal mucosa with only focal erosions. The patient was started on proton pump inhibitors twice daily. A repeat EGD revealed a two-channel opening into the duodenal bulb. The previous ulcer had formed in the post-pyloric channel, extending into the duodenal bulb with healed margins. (Fig. 2) Upon discussion with the pathologist, the repeat biopsies revealed healed ulcers & no eosinophilic infiltration, indicating that eosinophilia was likely a reactive response. Consequently, the possibility of eosinophilic gastritis was low, but peptic ulcer disease was more likely.
Discussion: This case highlights the importance of a multidisciplinary approach in managing patients with complex findings during endoscopy & histology. Eosinophilic gastritis exhibits nonspecific endoscopic findings, including nodular and polypoid mucosa, and, in rare cases, deep ulceration, and gastric eosinophilia is greater than 30/HPF. Discussion with a pathologist is essential when the diagnosis is in question, as treatment modalities differ.
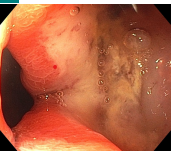
Figure: Double Channel Pylorus (Fig.2)
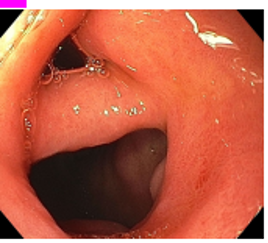
Figure: Pyloric ulcer (Fig.1)
Disclosures:
Kwabena Asafo-Agyei indicated no relevant financial relationships.
Angela Barnes indicated no relevant financial relationships.
Lakshmi Vemavarapu indicated no relevant financial relationships.
Leonard Little indicated no relevant financial relationships.
Kwabena Asafo-Agyei, MD1, Angela Barnes, MD2, Lakshmi Vemavarapu, MD3, Leonard Little, MD4. P6388 - Gastric Ulcer Presenting as a Double-Channel Pylorus: Could This Be Eosinophilic Gastritis?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

