Tuesday Poster Session
Category: Stomach and Spleen
P6364 - The Diagnosis of Eosinophilic Gastritis and Hypereosinophilic Syndrome
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Helene Bloom, DO
Allegheny Health Network Medicine Institute
Pittsburgh, PA
Presenting Author(s)
Helene Bloom, DO1, Alexandra M. Johnston, DO2, Stacey B. Miller, MD3
1Allegheny Health Network Medicine Institute, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA; 3Allegheny Health Network, Wexford, PA
Introduction: Eosinophilic Gastritis is a rare disorder with evidence of endothelial injury and eosinophilic infiltrates within the lamina propria. It is seen in 6.3/100,000 people and presents in patients 20 to 50 years old with nonspecific symptoms such as abdominal pain, nausea, vomiting and malabsorption. There are no definitive standards for diagnosis; however, findings supportive of diagnosis include elevated eosinophils on biopsy with >30 eosinophils per/hpf in gastric glands, lack of other organ involvement and exclusion of other causes of eosinophilia.
Case Description/
Methods: A 33-year-old female with a past history of anorexia nervosa and constipation predominant IBS presenting with new concerns of diarrhea with nighttime awakenings, lower abdominal pain, and nausea. She had a prior EGD completed in 2016 which was consistent with findings for Celiac disease, although she did not complete serologic testing. A CBC was obtained and pertinent for an absolute eosinophil count (AEC) of 2428 (normal 15-500 cells/uL). An extensive workup was completed as reported in Table 1.
The patient initiated a gluten free diet without symptom resolution. She subsequently underwent repeat EGD, confirming Celiac disease as well as gastric mucosa with focal increased density of eosinophils up to 100/ hpf. She was initiated on Mepolizumab with improvement in her diffuse pain and resolution of AEC to 101.
Discussion: This patient presented with new onset diarrhea and abdominal pain with a history of constipation and anorexia nervosa. She was found to have significant peripheral eosinophilia. Upon further negative workup, Hypereosinophilic Syndrome (HES) was proposed although there was no apparent tissue damage required for diagnosis. Due to her GI symptoms, an EGD was performed. Gastric biopsies showed > 100 eosinophils /hpf confirming tissue damage and a diagnosis of HES, but also identifying a rare eosinophilic gastritis diagnosis. It was critical to identify a change in symptoms from the patient’s baseline as well as avoiding anchoring on prior diagnoses like IBS, anorexia, and Celiac disease to reach the diagnosis of HES and eosinophilic gastritis.
It is important to consider that greater than one diagnosis may be driving a patient's presentation, especially when an underlying functional GI condition has been diagnosed and there is a change in the frequency, severity or quality of symptoms. This case highlights the importance of maintaining a broad differential diagnosis when a change in symptoms develops.
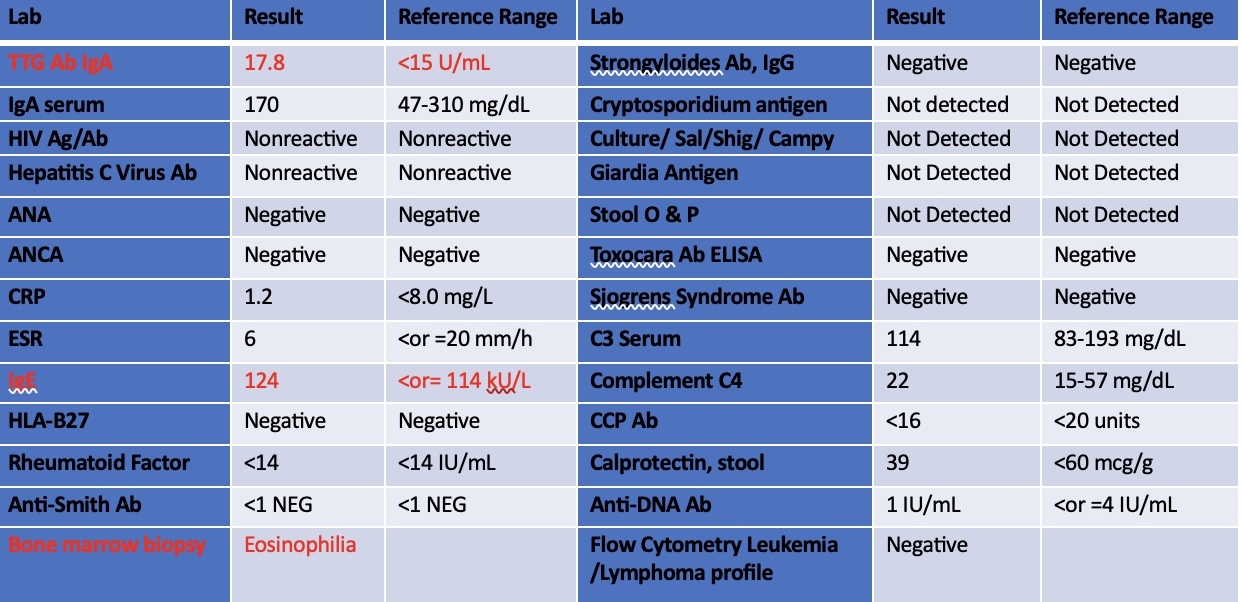
Figure: Table 1. Laboratory workup conducted to rule out other infectious, autoimmune and malignant causes of peripheral eosinophilia.

Figure: Figure 1. Gastric biopsy
Disclosures:
Helene Bloom indicated no relevant financial relationships.
Alexandra Johnston indicated no relevant financial relationships.
Stacey Miller indicated no relevant financial relationships.
Helene Bloom, DO1, Alexandra M. Johnston, DO2, Stacey B. Miller, MD3. P6364 - The Diagnosis of Eosinophilic Gastritis and Hypereosinophilic Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Allegheny Health Network Medicine Institute, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA; 3Allegheny Health Network, Wexford, PA
Introduction: Eosinophilic Gastritis is a rare disorder with evidence of endothelial injury and eosinophilic infiltrates within the lamina propria. It is seen in 6.3/100,000 people and presents in patients 20 to 50 years old with nonspecific symptoms such as abdominal pain, nausea, vomiting and malabsorption. There are no definitive standards for diagnosis; however, findings supportive of diagnosis include elevated eosinophils on biopsy with >30 eosinophils per/hpf in gastric glands, lack of other organ involvement and exclusion of other causes of eosinophilia.
Case Description/
Methods: A 33-year-old female with a past history of anorexia nervosa and constipation predominant IBS presenting with new concerns of diarrhea with nighttime awakenings, lower abdominal pain, and nausea. She had a prior EGD completed in 2016 which was consistent with findings for Celiac disease, although she did not complete serologic testing. A CBC was obtained and pertinent for an absolute eosinophil count (AEC) of 2428 (normal 15-500 cells/uL). An extensive workup was completed as reported in Table 1.
The patient initiated a gluten free diet without symptom resolution. She subsequently underwent repeat EGD, confirming Celiac disease as well as gastric mucosa with focal increased density of eosinophils up to 100/ hpf. She was initiated on Mepolizumab with improvement in her diffuse pain and resolution of AEC to 101.
Discussion: This patient presented with new onset diarrhea and abdominal pain with a history of constipation and anorexia nervosa. She was found to have significant peripheral eosinophilia. Upon further negative workup, Hypereosinophilic Syndrome (HES) was proposed although there was no apparent tissue damage required for diagnosis. Due to her GI symptoms, an EGD was performed. Gastric biopsies showed > 100 eosinophils /hpf confirming tissue damage and a diagnosis of HES, but also identifying a rare eosinophilic gastritis diagnosis. It was critical to identify a change in symptoms from the patient’s baseline as well as avoiding anchoring on prior diagnoses like IBS, anorexia, and Celiac disease to reach the diagnosis of HES and eosinophilic gastritis.
It is important to consider that greater than one diagnosis may be driving a patient's presentation, especially when an underlying functional GI condition has been diagnosed and there is a change in the frequency, severity or quality of symptoms. This case highlights the importance of maintaining a broad differential diagnosis when a change in symptoms develops.
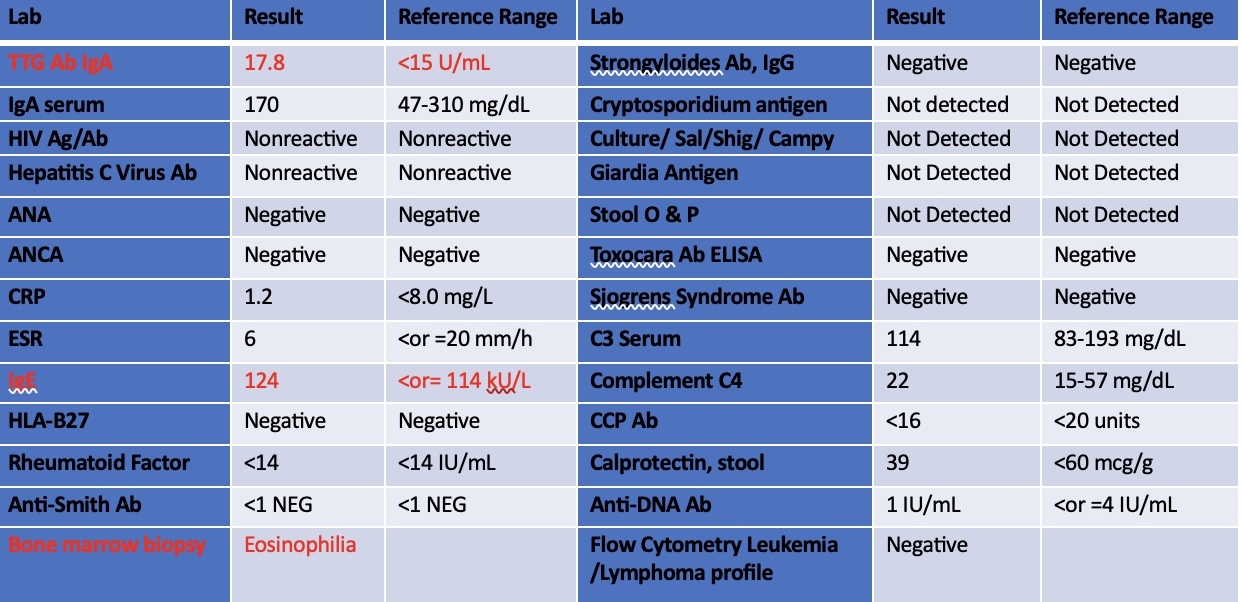
Figure: Table 1. Laboratory workup conducted to rule out other infectious, autoimmune and malignant causes of peripheral eosinophilia.

Figure: Figure 1. Gastric biopsy
Disclosures:
Helene Bloom indicated no relevant financial relationships.
Alexandra Johnston indicated no relevant financial relationships.
Stacey Miller indicated no relevant financial relationships.
Helene Bloom, DO1, Alexandra M. Johnston, DO2, Stacey B. Miller, MD3. P6364 - The Diagnosis of Eosinophilic Gastritis and Hypereosinophilic Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
