Tuesday Poster Session
Category: Stomach and Spleen
P6349 - Conservative Rescue of a Full-Thickness Buried Bumper Syndrome: Avoiding Surgery With Delayed Re-Placement
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- HN
Hao The Nguyen
Rocky Vista University
waldorf, MD
Presenting Author(s)
Hao The Nguyen, 1, Toma Evanoff, 1, Jaren Yatsu, 1, Michelle Hor, MD2
1Rocky Vista University, Colorado Springs, CO; 2University of Colorado School of Medicine, Colorado Springs, CO
Introduction: Buried bumper syndrome (BBS) is an uncommon but serious complication of percutaneous endoscopic gastrostomy (PEG) tube placement, where the internal bumper migrates into the gastric wall or beyond, usually due to excessive pressure between the internal and external bumpers. Complications include bleeding, perforation, peritonitis, and death. Treatment is typically endoscopic, with surgery reserved for severe cases. We report a case of BBS with full-thickness gastric wall penetration managed conservatively, delaying replacement until after mucosal healing.
Case Description/
Methods: A 21-year-old male with Batten’s disease and seizure disorder presented to the ED with pain, swelling, and leakage around his PEG tube, which had been placed seven months earlier. Vital signs and labs were unremarkable. CT imaging suggested the PEG tube had migrated outside the gastric lumen. EGD revealed the balloon had deeply embedded into the anterior gastric wall. Upon removal, there was evidence of full-thickness penetration of the gastric wall into a fibrosed portion of the peritoneum. Given the risk of iatrogenic injury from replacement through inflamed tissue, a delayed replacement strategy was selected. The patient was started on TPN and a PPI to facilitate ulcer healing. Follow-up EGD performed eight days later revealed a well-healed gastric mucosa, with only a single, non-bleeding 8mm ulcer remaining. A new PEG tube was successfully placed under endoscopic and guide wire assistance. The patient tolerated the procedure well and was discharged three days later.
Discussion: Buried bumper syndrome is a potentially life-threatening complication of PEG tube use, with a reported incidence of 0.3% to 2.4%. Endoscopic management is the preferred approach, though surgery may be necessary when endoscopy fails or complications are severe. There is limited literature describing cases where PEG tubes were fully removed and replaced at a later time, such as in this case. The mortality rate following PEG placement ranges from 5% to 15%, depending on the indication and patient comorbidities. Due to its iatrogenic potential, care teams must continue to be vigilant and implement strict preventive measures to minimize risk of BBS. While endoscopic intervention is standard, literature on delayed PEG replacement following full-thickness erosion is limited. Our case demonstrates that conservative management with nutritional support and acid suppression can allow for safe delayed re-intervention in select stable patients.
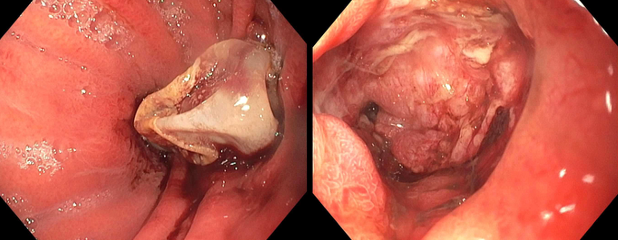
Figure: Initial endoscopy revealing full-thickness buried bumper syndrome.
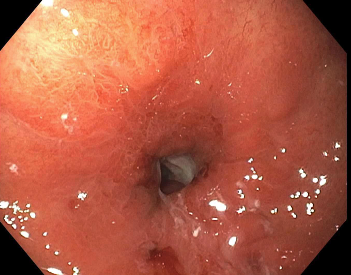
Figure: Endoscopy revealing healed mucosa following 8 days of initial PEG removal.
Disclosures:
Hao The Nguyen indicated no relevant financial relationships.
Toma Evanoff indicated no relevant financial relationships.
Jaren Yatsu indicated no relevant financial relationships.
Michelle Hor indicated no relevant financial relationships.
Hao The Nguyen, 1, Toma Evanoff, 1, Jaren Yatsu, 1, Michelle Hor, MD2. P6349 - Conservative Rescue of a Full-Thickness Buried Bumper Syndrome: Avoiding Surgery With Delayed Re-Placement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rocky Vista University, Colorado Springs, CO; 2University of Colorado School of Medicine, Colorado Springs, CO
Introduction: Buried bumper syndrome (BBS) is an uncommon but serious complication of percutaneous endoscopic gastrostomy (PEG) tube placement, where the internal bumper migrates into the gastric wall or beyond, usually due to excessive pressure between the internal and external bumpers. Complications include bleeding, perforation, peritonitis, and death. Treatment is typically endoscopic, with surgery reserved for severe cases. We report a case of BBS with full-thickness gastric wall penetration managed conservatively, delaying replacement until after mucosal healing.
Case Description/
Methods: A 21-year-old male with Batten’s disease and seizure disorder presented to the ED with pain, swelling, and leakage around his PEG tube, which had been placed seven months earlier. Vital signs and labs were unremarkable. CT imaging suggested the PEG tube had migrated outside the gastric lumen. EGD revealed the balloon had deeply embedded into the anterior gastric wall. Upon removal, there was evidence of full-thickness penetration of the gastric wall into a fibrosed portion of the peritoneum. Given the risk of iatrogenic injury from replacement through inflamed tissue, a delayed replacement strategy was selected. The patient was started on TPN and a PPI to facilitate ulcer healing. Follow-up EGD performed eight days later revealed a well-healed gastric mucosa, with only a single, non-bleeding 8mm ulcer remaining. A new PEG tube was successfully placed under endoscopic and guide wire assistance. The patient tolerated the procedure well and was discharged three days later.
Discussion: Buried bumper syndrome is a potentially life-threatening complication of PEG tube use, with a reported incidence of 0.3% to 2.4%. Endoscopic management is the preferred approach, though surgery may be necessary when endoscopy fails or complications are severe. There is limited literature describing cases where PEG tubes were fully removed and replaced at a later time, such as in this case. The mortality rate following PEG placement ranges from 5% to 15%, depending on the indication and patient comorbidities. Due to its iatrogenic potential, care teams must continue to be vigilant and implement strict preventive measures to minimize risk of BBS. While endoscopic intervention is standard, literature on delayed PEG replacement following full-thickness erosion is limited. Our case demonstrates that conservative management with nutritional support and acid suppression can allow for safe delayed re-intervention in select stable patients.
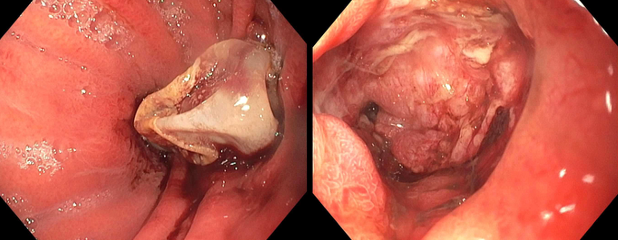
Figure: Initial endoscopy revealing full-thickness buried bumper syndrome.
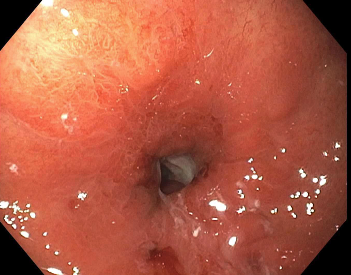
Figure: Endoscopy revealing healed mucosa following 8 days of initial PEG removal.
Disclosures:
Hao The Nguyen indicated no relevant financial relationships.
Toma Evanoff indicated no relevant financial relationships.
Jaren Yatsu indicated no relevant financial relationships.
Michelle Hor indicated no relevant financial relationships.
Hao The Nguyen, 1, Toma Evanoff, 1, Jaren Yatsu, 1, Michelle Hor, MD2. P6349 - Conservative Rescue of a Full-Thickness Buried Bumper Syndrome: Avoiding Surgery With Delayed Re-Placement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
