Monday Poster Session
Category: Biliary/Pancreas
P2179 - Procedural Trends and In-Hospital Outcomes of Biliary Acute Pancreatitis in HIV-Positive Patients: A National Inpatient Sample Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mohamed Karam Douedari, MD
Mount Sinai Medical Center
Miami Beach, FL
Presenting Author(s)
Mohamed Karam Douedari, MD1, Mohammad Asfari, MD2
1Mount Sinai Medical Center, Miami Beach, FL; 2Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL
Introduction: Growing evidence suggests that HIV infection may influence the presentation of acute pancreatitis (AP) [1], but nationally representative data on biliary AP outcomes remain limited. Using the National Inpatient Sample (NIS), this study aims to assess in-hospital outcomes, including mortality, complications, procedural rates, length of stay, and hospital charges among HIV-positive adults admitted with biliary AP.
Methods: We conducted a retrospective cohort study using the 2019–2022 National Inpatient Sample. Adults with a principal diagnosis of biliary AP and comorbid HIV were identified using ICD-10-CM codes. The primary outcome was in-hospital mortality. Secondary outcomes included complications, ERCP and cholecystectomy rates, length of stay, and hospital charges. Multivariable regression adjusted for demographics, comorbidities, hospital, and socioeconomic factors (Table 1).
Results: Among 176,734 adult biliary AP admissions, 677 had HIV (0.38%). Compared to HIV-negative patients, those with HIV were younger, more likely to be male and Black, and had a higher burden of comorbidities (Table 1). There was no significant difference in in-hospital mortality, necrotizing AP, AKI, or shock between HIV-positive and HIV-negative patients. However, HIV-positive patients had higher odds of respiratory failure (OR = 2.08, 95% CI: 1.04–4.16, p = 0.039). HIV-positive patients had higher odds of undergoing ERCP (OR = 1.56, p = 0.040) but lower odds of same-admission cholecystectomy (OR = 0.62, p = 0.016) (Figure 1). HIV-positive patients had a longer hospital stay (7.39 vs 4.82 days) and higher total hospitalization charges ($97,453 vs $67,822), though the differences in length of stay and charges were not statistically significant after adjustment.
Discussion: Our study demonstrates that HIV-positive patients admitted with biliary AP are at increased risk for severe complications, particularly respiratory failure. They also had significantly higher need for ERCP interventions. Notably, we observed a lower rate of same-admission cholecystectomy among HIV-positive patients. These findings underscore the need for heightened clinical vigilance and individualized management strategies in this population.
References:
1. Anderson F, et al. Predicting gallstone pancreatitis in HIV infected patients. S Afr J Surg. 2024 May;62(2):50–53.
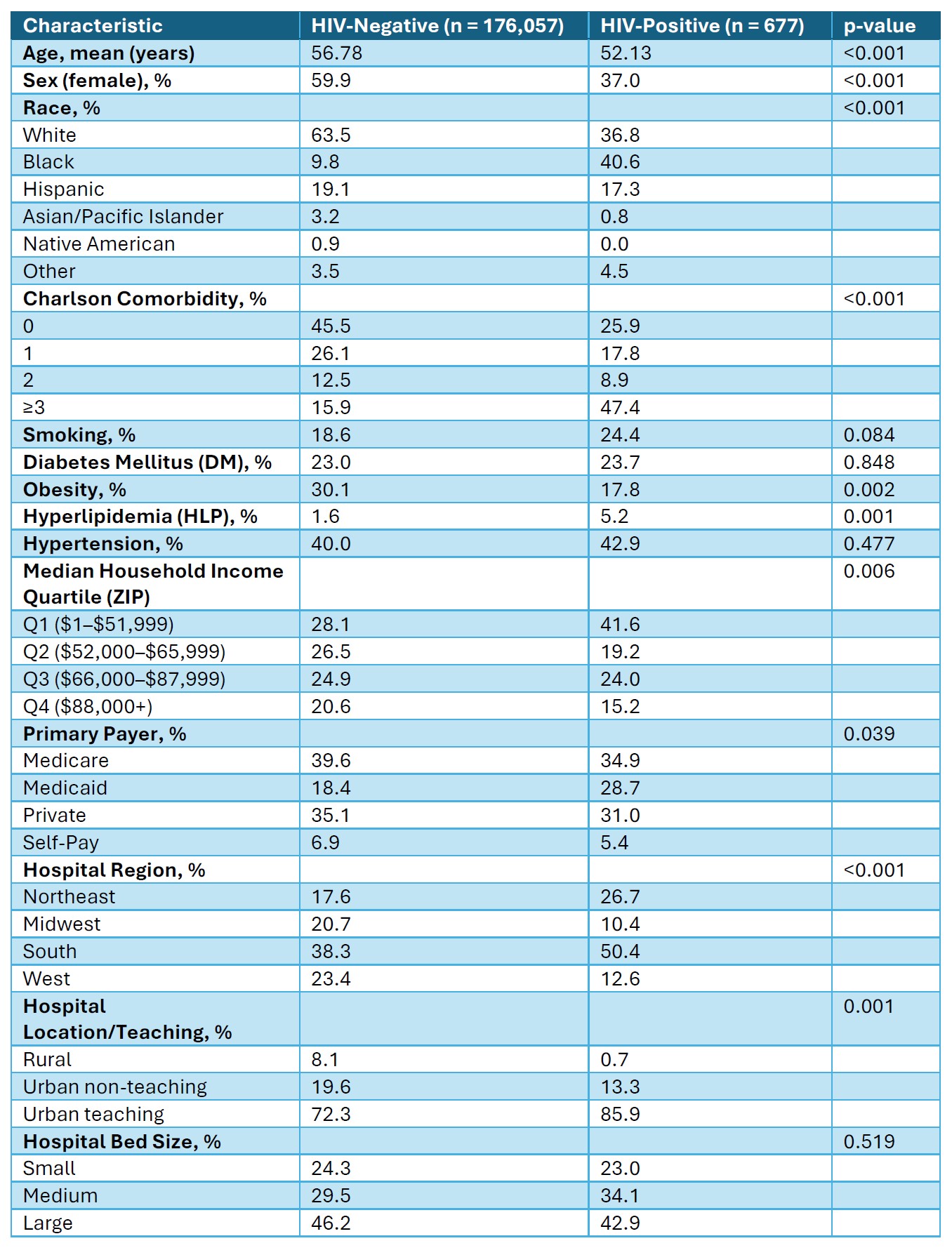
Figure: Table 1. Baseline Characteristics by HIV Status in Biliary Acute Pancreatitis
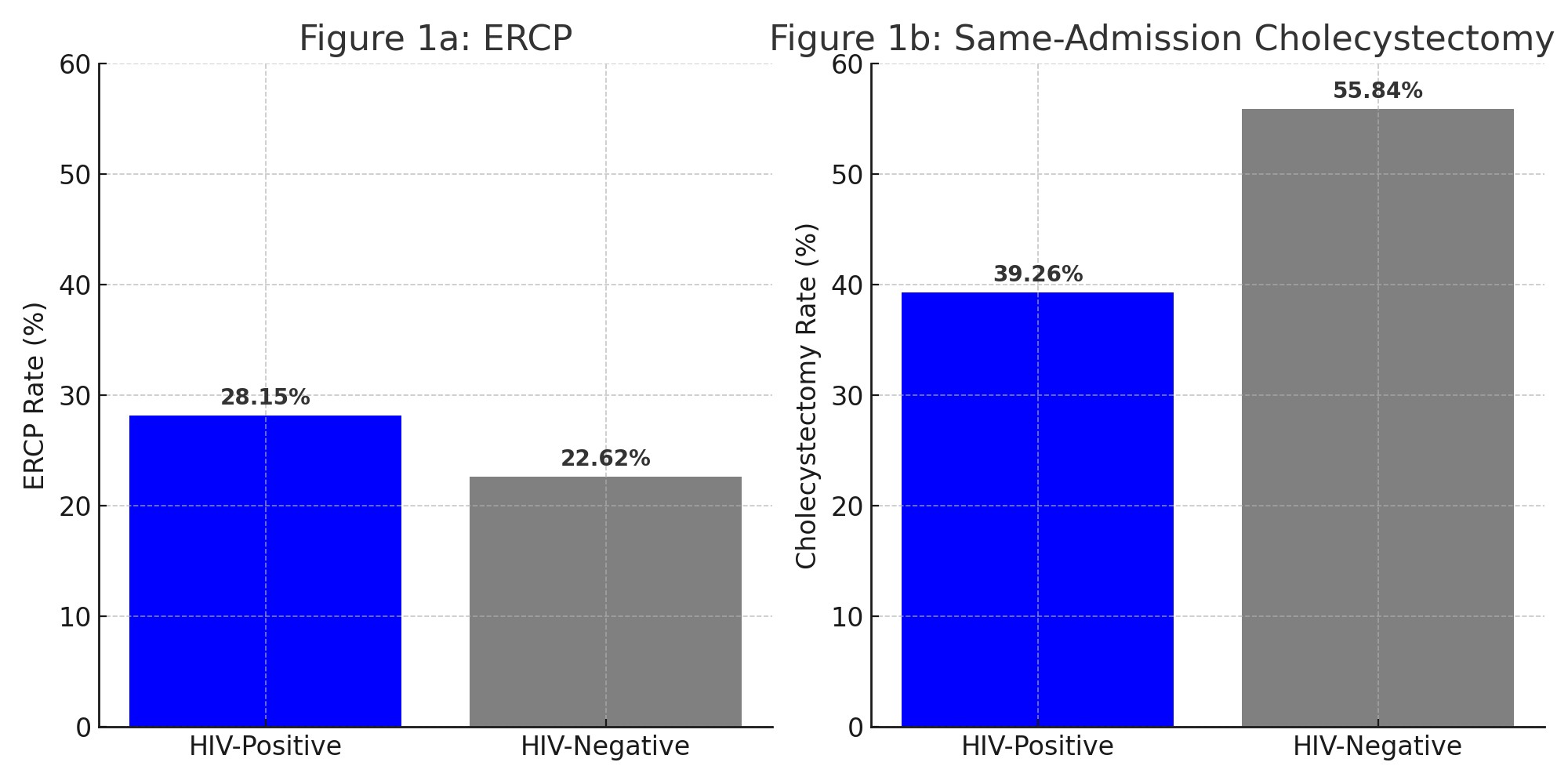
Figure: Figure 1: ERCP (1a) and Same-Admission Cholecystectomy (1b) Rates by HIV Status Among Adults Hospitalized with Biliary Acute Pancreatitis
Disclosures:
Mohamed Karam Douedari indicated no relevant financial relationships.
Mohammad Asfari indicated no relevant financial relationships.
Mohamed Karam Douedari, MD1, Mohammad Asfari, MD2. P2179 - Procedural Trends and In-Hospital Outcomes of Biliary Acute Pancreatitis in HIV-Positive Patients: A National Inpatient Sample Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mount Sinai Medical Center, Miami Beach, FL; 2Department of Gastroenterology and Hepatology, AdventHealth Orlando, Orlando, FL
Introduction: Growing evidence suggests that HIV infection may influence the presentation of acute pancreatitis (AP) [1], but nationally representative data on biliary AP outcomes remain limited. Using the National Inpatient Sample (NIS), this study aims to assess in-hospital outcomes, including mortality, complications, procedural rates, length of stay, and hospital charges among HIV-positive adults admitted with biliary AP.
Methods: We conducted a retrospective cohort study using the 2019–2022 National Inpatient Sample. Adults with a principal diagnosis of biliary AP and comorbid HIV were identified using ICD-10-CM codes. The primary outcome was in-hospital mortality. Secondary outcomes included complications, ERCP and cholecystectomy rates, length of stay, and hospital charges. Multivariable regression adjusted for demographics, comorbidities, hospital, and socioeconomic factors (Table 1).
Results: Among 176,734 adult biliary AP admissions, 677 had HIV (0.38%). Compared to HIV-negative patients, those with HIV were younger, more likely to be male and Black, and had a higher burden of comorbidities (Table 1). There was no significant difference in in-hospital mortality, necrotizing AP, AKI, or shock between HIV-positive and HIV-negative patients. However, HIV-positive patients had higher odds of respiratory failure (OR = 2.08, 95% CI: 1.04–4.16, p = 0.039). HIV-positive patients had higher odds of undergoing ERCP (OR = 1.56, p = 0.040) but lower odds of same-admission cholecystectomy (OR = 0.62, p = 0.016) (Figure 1). HIV-positive patients had a longer hospital stay (7.39 vs 4.82 days) and higher total hospitalization charges ($97,453 vs $67,822), though the differences in length of stay and charges were not statistically significant after adjustment.
Discussion: Our study demonstrates that HIV-positive patients admitted with biliary AP are at increased risk for severe complications, particularly respiratory failure. They also had significantly higher need for ERCP interventions. Notably, we observed a lower rate of same-admission cholecystectomy among HIV-positive patients. These findings underscore the need for heightened clinical vigilance and individualized management strategies in this population.
References:
1. Anderson F, et al. Predicting gallstone pancreatitis in HIV infected patients. S Afr J Surg. 2024 May;62(2):50–53.
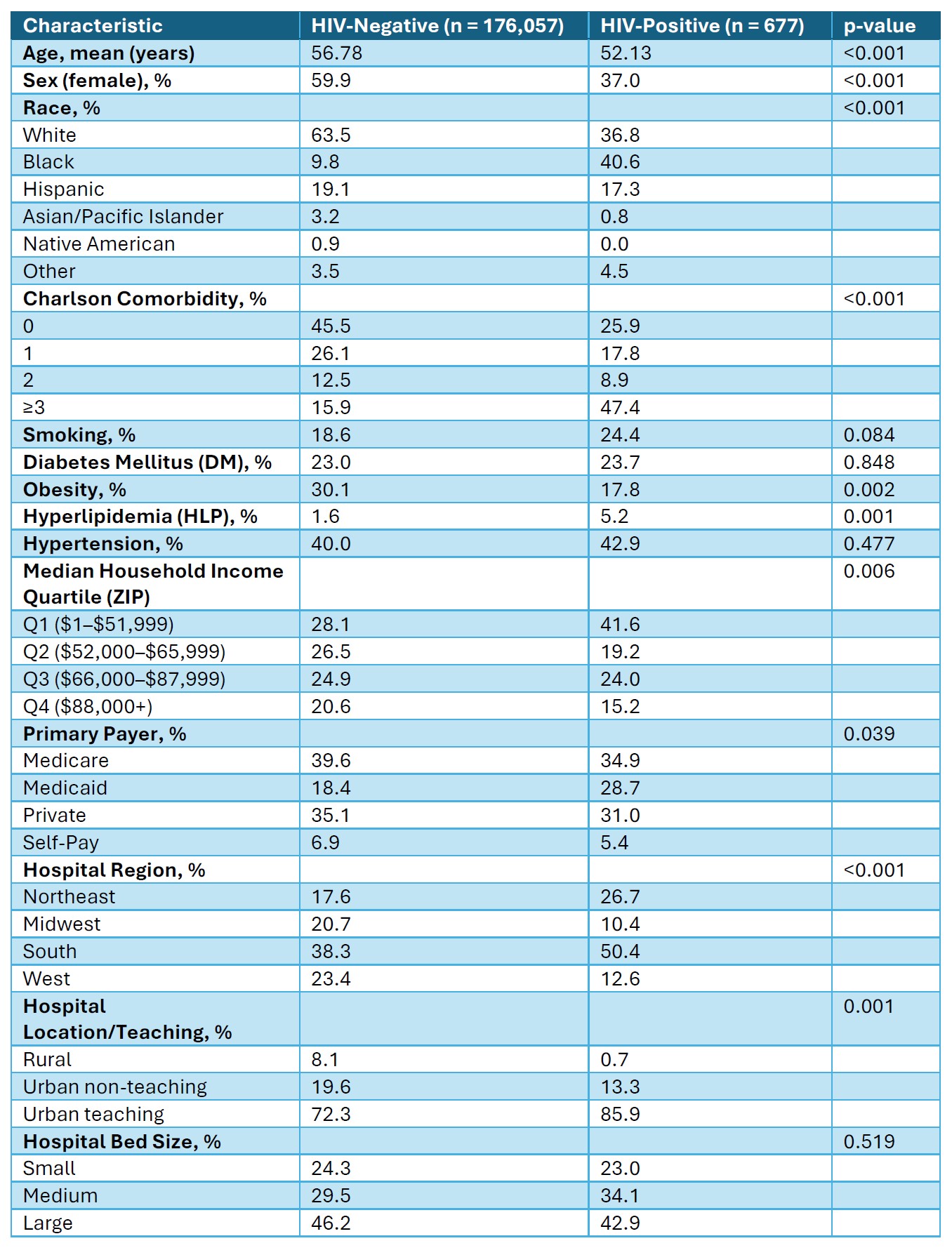
Figure: Table 1. Baseline Characteristics by HIV Status in Biliary Acute Pancreatitis
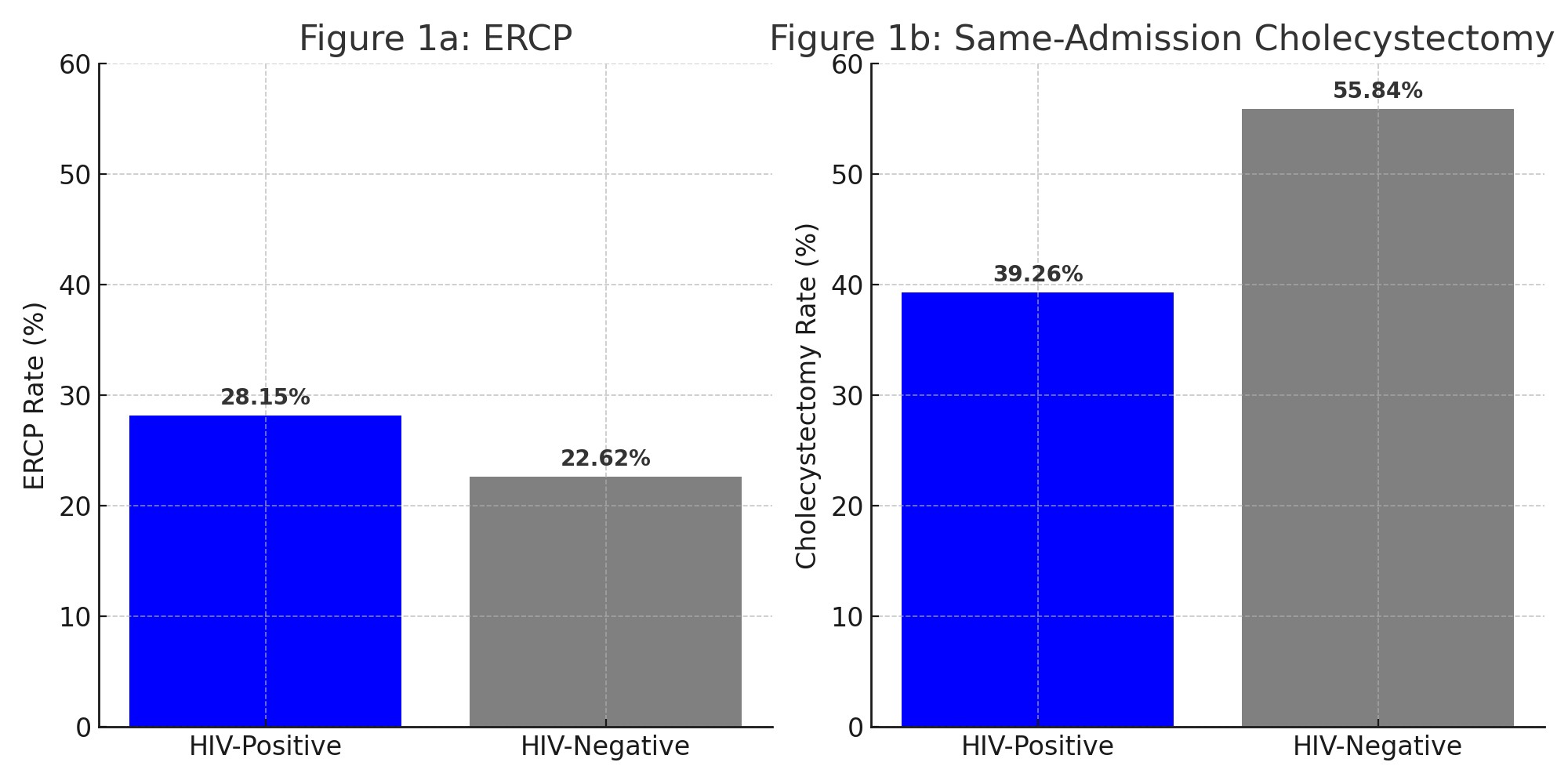
Figure: Figure 1: ERCP (1a) and Same-Admission Cholecystectomy (1b) Rates by HIV Status Among Adults Hospitalized with Biliary Acute Pancreatitis
Disclosures:
Mohamed Karam Douedari indicated no relevant financial relationships.
Mohammad Asfari indicated no relevant financial relationships.
Mohamed Karam Douedari, MD1, Mohammad Asfari, MD2. P2179 - Procedural Trends and In-Hospital Outcomes of Biliary Acute Pancreatitis in HIV-Positive Patients: A National Inpatient Sample Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

