Monday Poster Session
Category: Biliary/Pancreas
P2171 - Comparative Outcomes of Curative Vw Palliative Pancreatic Cancer Surgery: A Propensity Score-Matched National Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Iqra Arshad, MD, MPH (she/her/hers)
SSM Health Saint Louis University Hospital
Saint Louis, MO
Presenting Author(s)
Nehemias Guevara Rodriguez, MD1, Iqra Arshad, MD, MPH1, Ronald Blanco Montecino, MD2, Noemy Coreas, MD3, Noemy Coreas, MD4, Mahmoud Y. Madi, MD5, Syeda Ashna Kamal, MD1, Tarek Nammour, MD1
1SSM Health Saint Louis University Hospital, Saint Louis, MO; 2St. Barnabas Hospital, New York, NY; 3National University of El Salvador, El Salvador, San Salvador, El Salvador; 4National University of El salvador, El Salvador, American Samoa; 5University of Texas at Austin Dell Medical School, Austin, TX
Introduction: Surgical intervention remains a cornerstone of treatment for early-stage pancreatic cancer. In advanced stages, surgery is often performed with palliative intent, such as relieving symptoms of biliary and/or gastric outlet obstruction. However, national data comparing outcomes between curative and palliative surgical approaches remains limited. This study assessed differences in the in-hospital mortality, length of stay, healthcare resources utilization, and postoperative complications between these two groups using a nationally representative cohort.
Methods: We conducted a retrospective study using the Nationwide Readmissions Database from 2016 to 2019. Adult patients undergoing surgery for pancreatic cancer were identified and stratified by surgical intent (curative vs. palliative). Demographic, hospital, and clinical data were collected. Propensity score matching (1:1) was performed based on age, sex, insurance status, comorbidities, and hospital characteristics. Covariate balance was assessed using standardized differences (< 0.1 considered acceptable). Postoperative survival within 60 days was evaluated using Kaplan-Meier analysis.
Results: 4,295 matched patients were included (palliative: n=2,189; curative: n=2,106). Palliative patients were slightly older (mean age 69.2 vs. 67.5 years, p< 0.001), more likely to be covered by Medicaid (11.3% vs. 8.9%, p=0.01), and had higher rates of intensive care unit admission (84.8% vs. 80.9%, p=0.001). Postoperative complications were more frequent in the palliative group, including sepsis (11.7% vs. 3.9%, p< 0.001), respiratory failure (3.7% vs. 1.4%, p< 0.001), and pneumonia (2.7% vs. 1.5%, p =0.006). Furthermore, higher rates of pancreatic leaks were observed in patients undergoing palliative surgery (2.7% vs. 2.0%, p< 0.0001). The mean length of stay was also longer among patients undergoing palliative surgery (6.8 vs. 5.5 days, p< 0.001) (Table 1). Kaplan-Meier curves (Figure 1) showed reduced short-term survival in the palliative group.
Discussion: After adjustment for baseline characteristics, palliative pancreatic surgery was associated with higher complication rates, prolonged hospitalization, and reduced early survival. These findings underscore the complex clinical course and elevated perioperative risks of palliative surgical interventions. Early integration of palliative care and multidisciplinary decision-making may enhance patient selection and optimize outcomes.
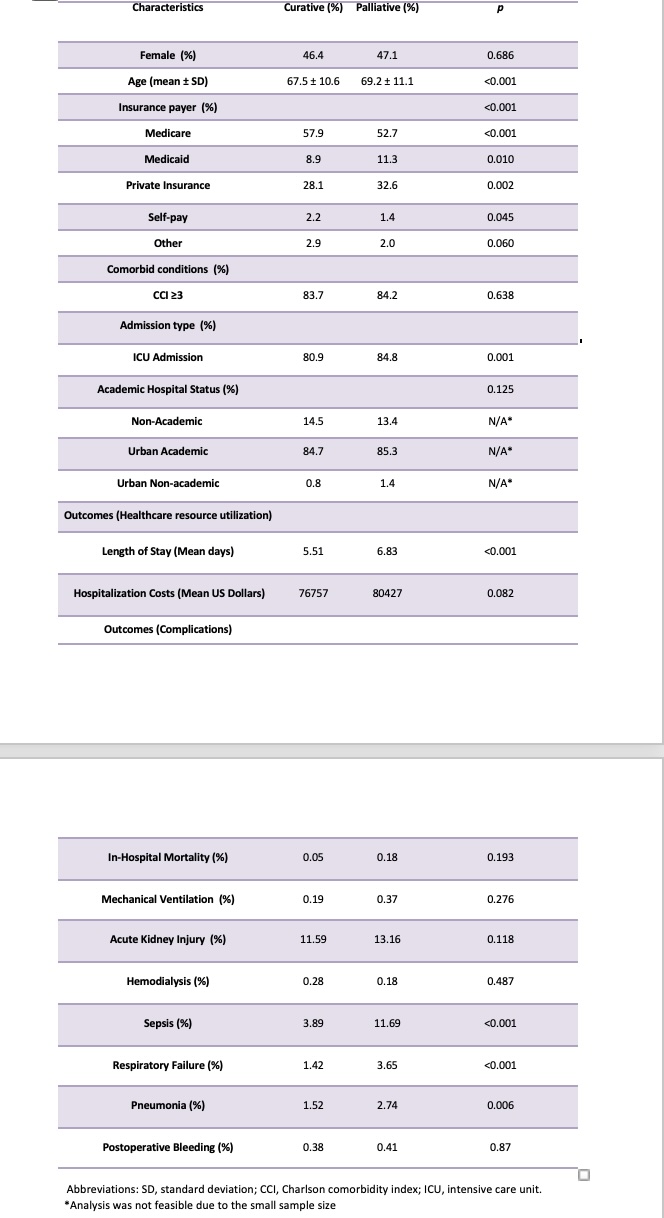
Figure: Table 1. Baseline Characteristics and Outcomes of Patients undergoing Curative Surgery for Pancreatic Cancer Compared to those undergoing Palliative Surgery
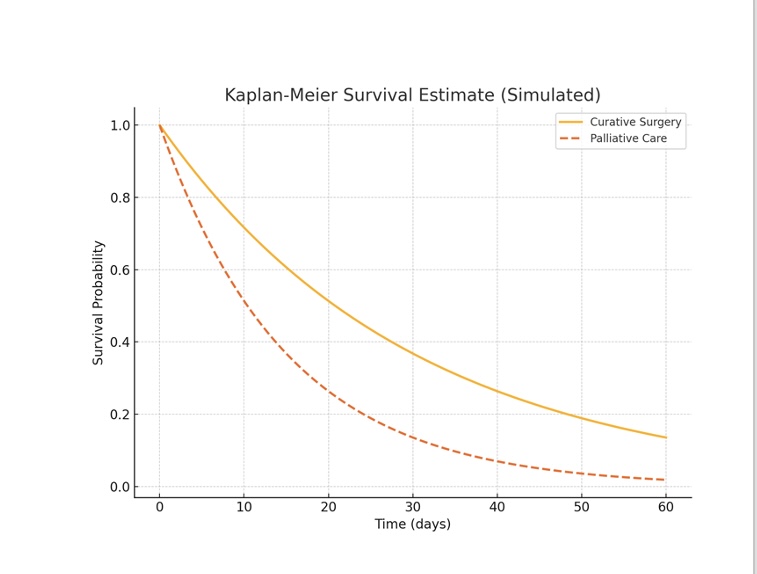
Figure: Figure 1. Kaplan-Meier Survival Curve Comparing The Two Groups
Disclosures:
Nehemias Guevara Rodriguez indicated no relevant financial relationships.
Iqra Arshad indicated no relevant financial relationships.
Ronald Blanco Montecino indicated no relevant financial relationships.
Noemy Coreas indicated no relevant financial relationships.
Noemy Coreas indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Syeda Ashna Kamal indicated no relevant financial relationships.
Tarek Nammour indicated no relevant financial relationships.
Nehemias Guevara Rodriguez, MD1, Iqra Arshad, MD, MPH1, Ronald Blanco Montecino, MD2, Noemy Coreas, MD3, Noemy Coreas, MD4, Mahmoud Y. Madi, MD5, Syeda Ashna Kamal, MD1, Tarek Nammour, MD1. P2171 - Comparative Outcomes of Curative Vw Palliative Pancreatic Cancer Surgery: A Propensity Score-Matched National Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SSM Health Saint Louis University Hospital, Saint Louis, MO; 2St. Barnabas Hospital, New York, NY; 3National University of El Salvador, El Salvador, San Salvador, El Salvador; 4National University of El salvador, El Salvador, American Samoa; 5University of Texas at Austin Dell Medical School, Austin, TX
Introduction: Surgical intervention remains a cornerstone of treatment for early-stage pancreatic cancer. In advanced stages, surgery is often performed with palliative intent, such as relieving symptoms of biliary and/or gastric outlet obstruction. However, national data comparing outcomes between curative and palliative surgical approaches remains limited. This study assessed differences in the in-hospital mortality, length of stay, healthcare resources utilization, and postoperative complications between these two groups using a nationally representative cohort.
Methods: We conducted a retrospective study using the Nationwide Readmissions Database from 2016 to 2019. Adult patients undergoing surgery for pancreatic cancer were identified and stratified by surgical intent (curative vs. palliative). Demographic, hospital, and clinical data were collected. Propensity score matching (1:1) was performed based on age, sex, insurance status, comorbidities, and hospital characteristics. Covariate balance was assessed using standardized differences (< 0.1 considered acceptable). Postoperative survival within 60 days was evaluated using Kaplan-Meier analysis.
Results: 4,295 matched patients were included (palliative: n=2,189; curative: n=2,106). Palliative patients were slightly older (mean age 69.2 vs. 67.5 years, p< 0.001), more likely to be covered by Medicaid (11.3% vs. 8.9%, p=0.01), and had higher rates of intensive care unit admission (84.8% vs. 80.9%, p=0.001). Postoperative complications were more frequent in the palliative group, including sepsis (11.7% vs. 3.9%, p< 0.001), respiratory failure (3.7% vs. 1.4%, p< 0.001), and pneumonia (2.7% vs. 1.5%, p =0.006). Furthermore, higher rates of pancreatic leaks were observed in patients undergoing palliative surgery (2.7% vs. 2.0%, p< 0.0001). The mean length of stay was also longer among patients undergoing palliative surgery (6.8 vs. 5.5 days, p< 0.001) (Table 1). Kaplan-Meier curves (Figure 1) showed reduced short-term survival in the palliative group.
Discussion: After adjustment for baseline characteristics, palliative pancreatic surgery was associated with higher complication rates, prolonged hospitalization, and reduced early survival. These findings underscore the complex clinical course and elevated perioperative risks of palliative surgical interventions. Early integration of palliative care and multidisciplinary decision-making may enhance patient selection and optimize outcomes.
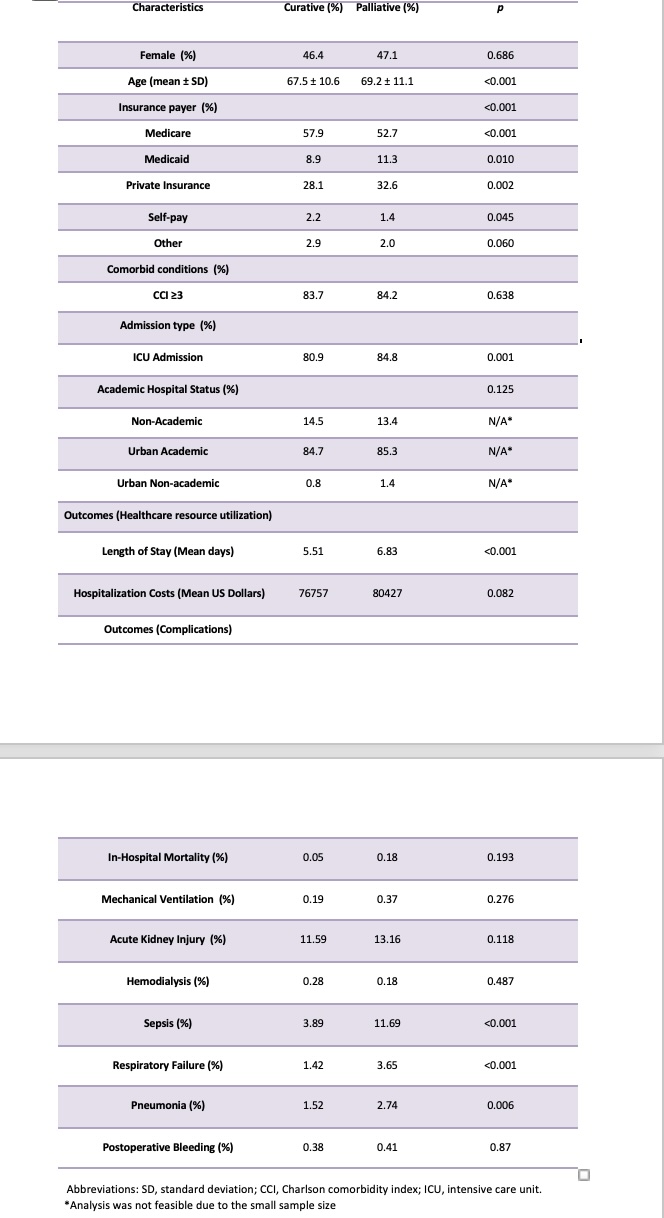
Figure: Table 1. Baseline Characteristics and Outcomes of Patients undergoing Curative Surgery for Pancreatic Cancer Compared to those undergoing Palliative Surgery
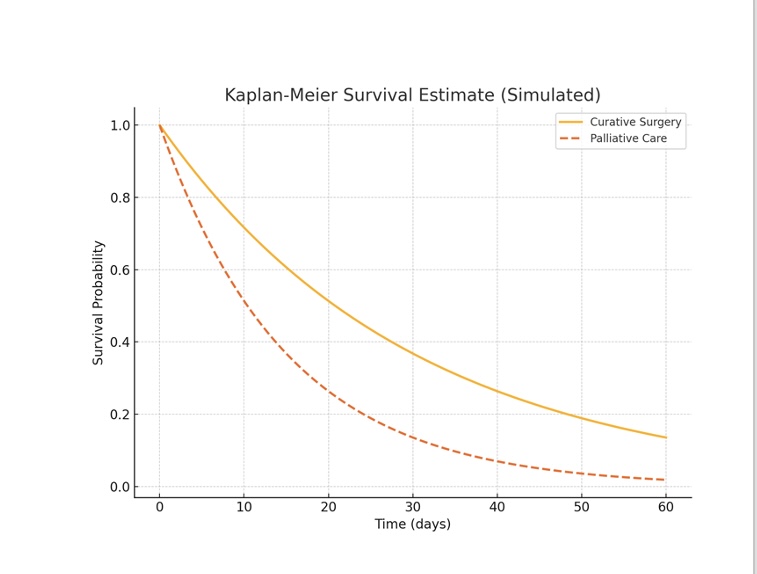
Figure: Figure 1. Kaplan-Meier Survival Curve Comparing The Two Groups
Disclosures:
Nehemias Guevara Rodriguez indicated no relevant financial relationships.
Iqra Arshad indicated no relevant financial relationships.
Ronald Blanco Montecino indicated no relevant financial relationships.
Noemy Coreas indicated no relevant financial relationships.
Noemy Coreas indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Syeda Ashna Kamal indicated no relevant financial relationships.
Tarek Nammour indicated no relevant financial relationships.
Nehemias Guevara Rodriguez, MD1, Iqra Arshad, MD, MPH1, Ronald Blanco Montecino, MD2, Noemy Coreas, MD3, Noemy Coreas, MD4, Mahmoud Y. Madi, MD5, Syeda Ashna Kamal, MD1, Tarek Nammour, MD1. P2171 - Comparative Outcomes of Curative Vw Palliative Pancreatic Cancer Surgery: A Propensity Score-Matched National Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
