Monday Poster Session
Category: Biliary/Pancreas
P2169 - Etiology-Based Outcomes of Acute Pancreatitis: A Multi-Center Real-World Analysis From a Nationwide EMR Network
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ashujot K. Dang, MD
University of California Riverside School of Medicine
Riverside, CA
Presenting Author(s)
Ashujot K. Dang, MD1, Vikash Kumar, MD2, Aalam Sohal, MD2, Avinash Nankani, MBBS3, Indu Srinivasan, MD2, Dalbir Sandhu, MD2
1University of California Riverside School of Medicine, Riverside, CA; 2Creighton University School of Medicine, Phoenix, AZ; 3Dow University of Health Sciences, Karachi, Sindh, Pakistan
Introduction: Acute pancreatitis (AP) exhibits heterogeneity in presentation, complications, and outcomes depending on etiology. There are only limited large-scale comparative studies that exist evaluating outcomes across biliary, alcoholic, hypertriglyceridemia-induced, and idiopathic/other causes of AP. This study aims to compare outcomes based on different etiologies of AP to improve overall patient outcomes.
Methods: We conducted a retrospective cohort analysis using the TriNetX US Collaborative Network, comprising 67 healthcare organizations. Inclusion criteria included Adults (≥18 years) with AP who were stratified into four cohorts by etiology: biliary (n=79,993), alcohol-induced (n=55,880), hypertriglyceridemia-induced (n=34,505), and idiopathic/other (n=8,157). Outcomes were assessed 1 year post-index diagnosis and included Recurrence of pancreatitis, Chronic pancreatitis, Pancreatic pseudocyst/fluid collections, Exocrine pancreatic insufficiency (EPI), and One-year mortality.
Results: After comparing different cohorts, outcomes varied significantly by etiology. Firstly, the recurrence of AP was highest in idiopathic/other (76.4%), followed by alcohol (54.4%), hypertriglyceridemia (48.5%), and lowest in biliary (59.0%) with Median time to recurrence; 14 days (idiopathic), 19 days (biliary), 85 days (alcohol), 284 days (hypertriglyceridemia). Secondly, Chronic pancreatitis was most frequent in idiopathic/other (18.0%) and alcohol (10.3%) groups compared to hypertriglyceridemia (8.7%) and biliary (4.7%). Furthermore, Pseudocyst/fluid collection was more common in idiopathic/other (18.9%) and alcohol (9.8%) than in biliary (6.2%) and hypertriglyceridemia (7.2%). However, exocrine pancreatic insufficiency was rare across all groups (≤0.3%). One-year mortality was seen highest in idiopathic/other (5.2%) and lowest in alcohol (3.9%). Mortality in the biliary and hypertriglyceridemia cohorts was 4.3% and 4.4%, respectively.
Discussion: This study indicates that the etiology of AP is a significant determinant of clinical outcomes. Idiopathic and alcohol-related AP are associated with higher recurrence and chronicity, while biliary and hypertriglyceridemia-related AP have relatively favorable survival profiles. Etiology-specific care pathways and preventive strategies may reduce morbidity and mortality in high-risk groups. Further studies are warranted to develop guidelines for cause-specific management of AP to overall improve patient outcomes.
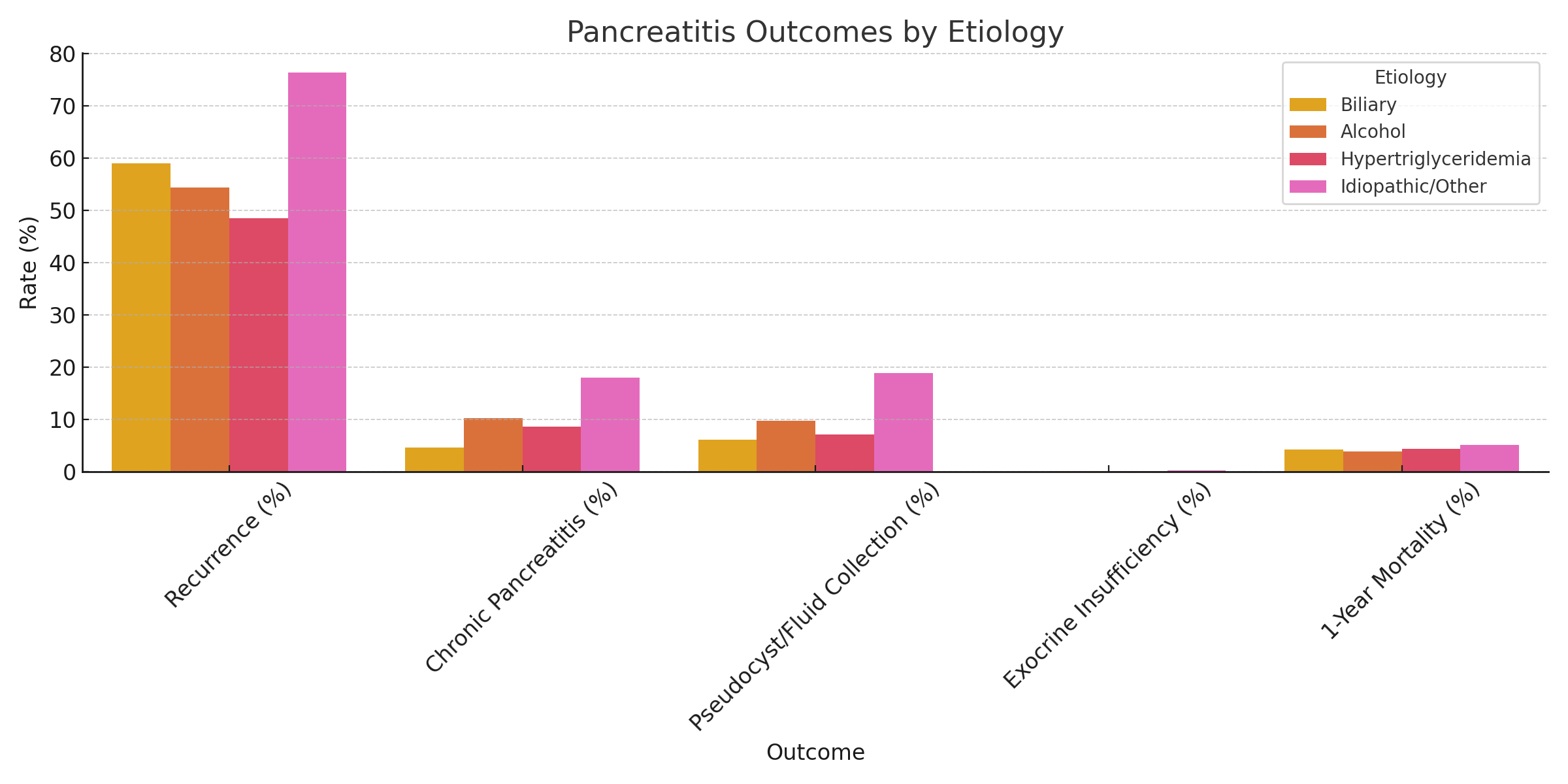
Figure: A table comparing the incidence of different outcomes based on etiology of acute pancreatitis
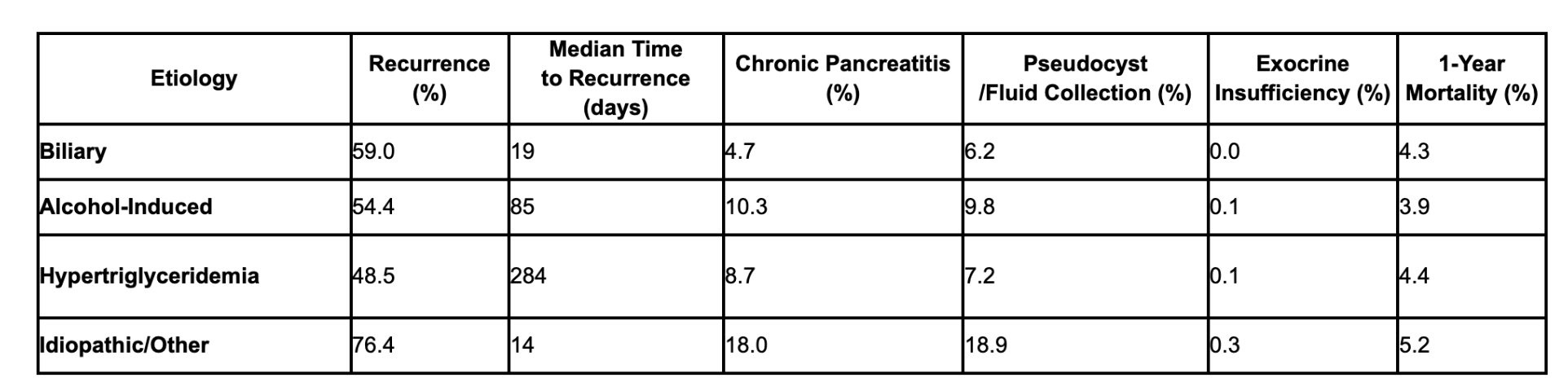
Figure: Figure depicting different etiologies and its comparison of outcomes
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Avinash Nankani indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Dalbir Sandhu indicated no relevant financial relationships.
Ashujot K. Dang, MD1, Vikash Kumar, MD2, Aalam Sohal, MD2, Avinash Nankani, MBBS3, Indu Srinivasan, MD2, Dalbir Sandhu, MD2. P2169 - Etiology-Based Outcomes of Acute Pancreatitis: A Multi-Center Real-World Analysis From a Nationwide EMR Network, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Riverside School of Medicine, Riverside, CA; 2Creighton University School of Medicine, Phoenix, AZ; 3Dow University of Health Sciences, Karachi, Sindh, Pakistan
Introduction: Acute pancreatitis (AP) exhibits heterogeneity in presentation, complications, and outcomes depending on etiology. There are only limited large-scale comparative studies that exist evaluating outcomes across biliary, alcoholic, hypertriglyceridemia-induced, and idiopathic/other causes of AP. This study aims to compare outcomes based on different etiologies of AP to improve overall patient outcomes.
Methods: We conducted a retrospective cohort analysis using the TriNetX US Collaborative Network, comprising 67 healthcare organizations. Inclusion criteria included Adults (≥18 years) with AP who were stratified into four cohorts by etiology: biliary (n=79,993), alcohol-induced (n=55,880), hypertriglyceridemia-induced (n=34,505), and idiopathic/other (n=8,157). Outcomes were assessed 1 year post-index diagnosis and included Recurrence of pancreatitis, Chronic pancreatitis, Pancreatic pseudocyst/fluid collections, Exocrine pancreatic insufficiency (EPI), and One-year mortality.
Results: After comparing different cohorts, outcomes varied significantly by etiology. Firstly, the recurrence of AP was highest in idiopathic/other (76.4%), followed by alcohol (54.4%), hypertriglyceridemia (48.5%), and lowest in biliary (59.0%) with Median time to recurrence; 14 days (idiopathic), 19 days (biliary), 85 days (alcohol), 284 days (hypertriglyceridemia). Secondly, Chronic pancreatitis was most frequent in idiopathic/other (18.0%) and alcohol (10.3%) groups compared to hypertriglyceridemia (8.7%) and biliary (4.7%). Furthermore, Pseudocyst/fluid collection was more common in idiopathic/other (18.9%) and alcohol (9.8%) than in biliary (6.2%) and hypertriglyceridemia (7.2%). However, exocrine pancreatic insufficiency was rare across all groups (≤0.3%). One-year mortality was seen highest in idiopathic/other (5.2%) and lowest in alcohol (3.9%). Mortality in the biliary and hypertriglyceridemia cohorts was 4.3% and 4.4%, respectively.
Discussion: This study indicates that the etiology of AP is a significant determinant of clinical outcomes. Idiopathic and alcohol-related AP are associated with higher recurrence and chronicity, while biliary and hypertriglyceridemia-related AP have relatively favorable survival profiles. Etiology-specific care pathways and preventive strategies may reduce morbidity and mortality in high-risk groups. Further studies are warranted to develop guidelines for cause-specific management of AP to overall improve patient outcomes.
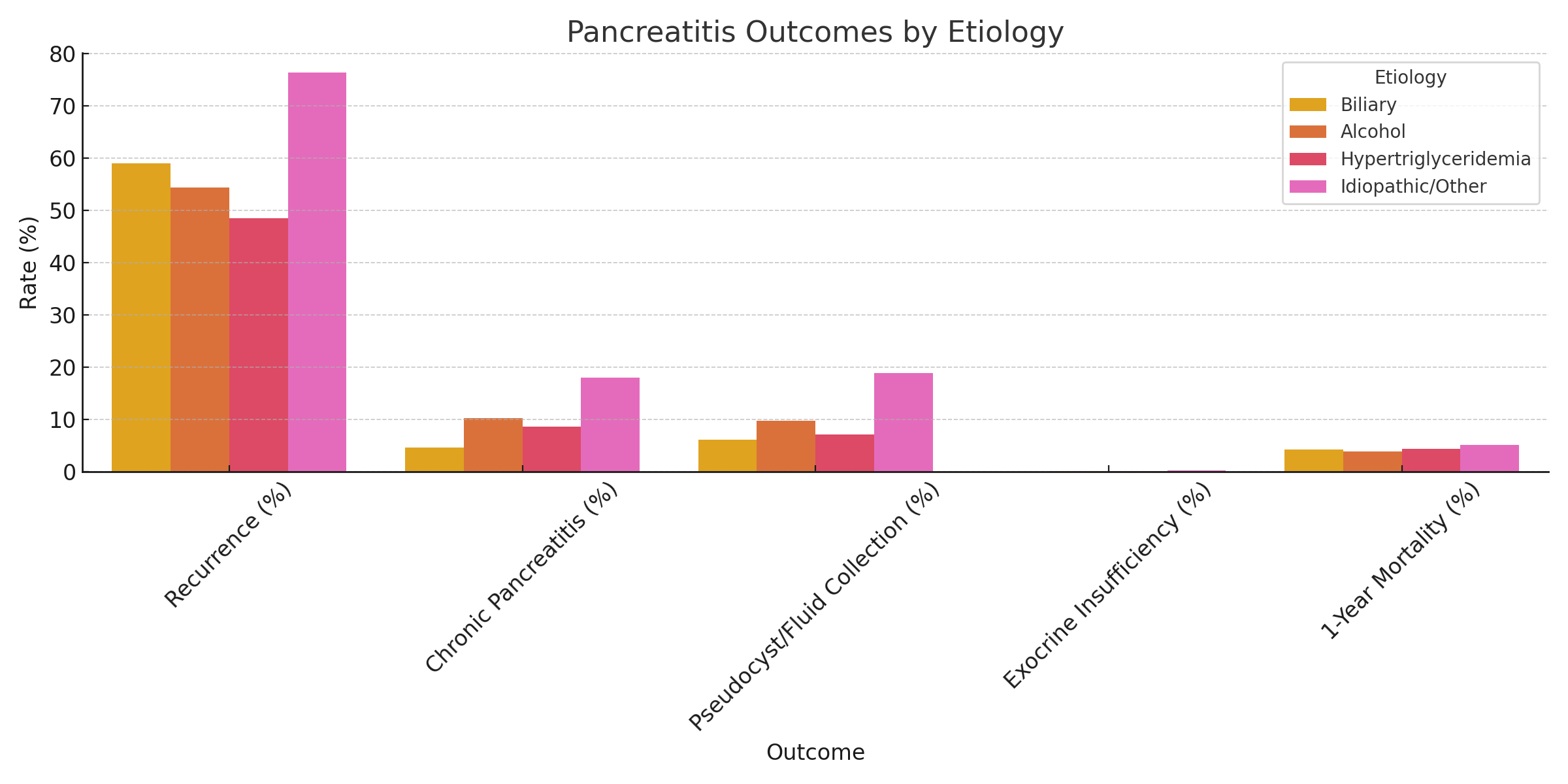
Figure: A table comparing the incidence of different outcomes based on etiology of acute pancreatitis
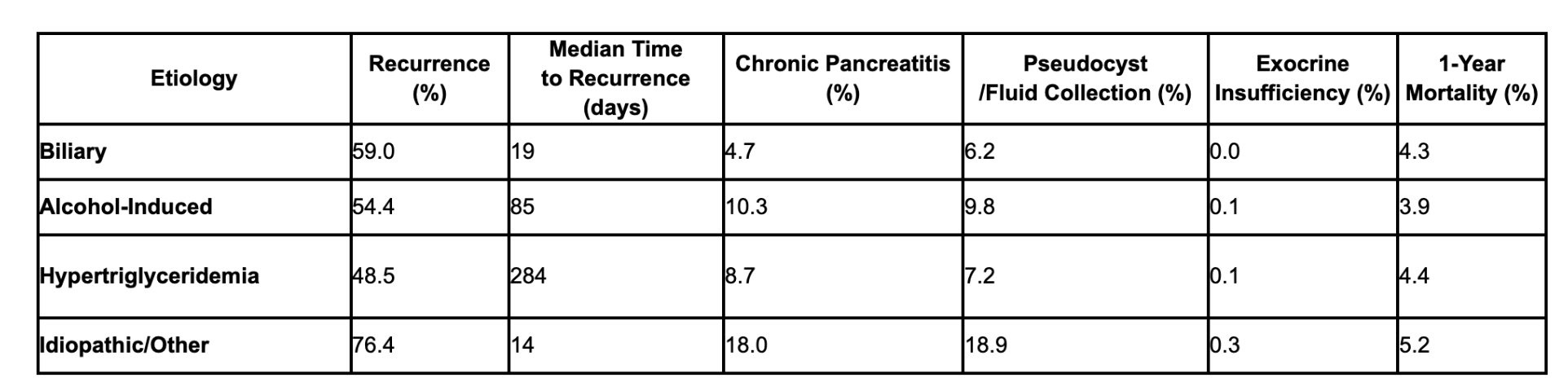
Figure: Figure depicting different etiologies and its comparison of outcomes
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Avinash Nankani indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Dalbir Sandhu indicated no relevant financial relationships.
Ashujot K. Dang, MD1, Vikash Kumar, MD2, Aalam Sohal, MD2, Avinash Nankani, MBBS3, Indu Srinivasan, MD2, Dalbir Sandhu, MD2. P2169 - Etiology-Based Outcomes of Acute Pancreatitis: A Multi-Center Real-World Analysis From a Nationwide EMR Network, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
