Monday Poster Session
Category: Biliary/Pancreas
P2309 - An Uncommon Presentation of a Cystic Pancreatic Neuroendocrine Tumor With Main Duct Dilatation Mimicking Intraductal Papillary Mucinous Neoplasm: A Diagnostic Pitfall
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nikita Garg, MD (she/her/hers)
Geisinger Wyoming Valley Medical Center
Wilkes-Barre, PA
Presenting Author(s)
Nikita Garg, MD1, Miles Graves, MD1, Tushar Abhinav, MD2, John K. Appiah, MD1, Danial Nadeem, MD1, Amit Sohagia, MD3, Nihaal Karnik, MD1
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2The Wright Center for Graduate Medical Education, Wilkes-Barre, PA; 3Geisinger Community Medical Center, Scranton, PA
Introduction: While pancreatic neuroendocrine tumors (PNETs) are rare and typically solid, 10-20% may present as cystic, making cystic PNETs an uncommon diagnostic challenge. Of these, very few present with intraductal growth, and the ones described thus far are most typically located in the tail of the pancreas. We present a case of a cystic neuroendocrine tumor at the pancreatic body with main pancreatic duct (MPD) dilatation, radiologically mimicking an intraductal papillary mucinous neoplasm (IPMN).
Case Description/
Methods: A 66-year-old male presented with abdominal pain and constipation. Contrast-enhanced abdominal computed tomography (CT) revealed an incidental 1 cm cystic lesion in the pancreatic body with upstream main pancreatic duct dilation to 7 mm. Follow-up abdominal magnetic resonance imaging (MRI) showed a 1.4 cm cystic lesion with 6 mm ductal dilation and no mural nodule, radiologically suspicious for mixed-type IPMN. Given the MPD dilatation, an endoscopic ultrasound was performed. EUS identified a 2.0 x 1.4 cm cystic lesion with a solid component, prompting fine needle aspiration (FNA). Cytology revealed a well-differentiated grade 1 PNET, positive for CAM5.2 and synaptophysin, Ki-67 < 3%. Gallium-68 DOTATATE PET demonstrated somatostatin receptor–positive, localized disease (Stage I: pT1, cN0, cM0). After a multidisciplinary discussion, the decision was made for a surgical resection given the solid component, main duct dilation, and interval growth on surveillance imaging. Histopathology confirmed a grade 2 NET with lymphovascular invasion and R0 resection. The patient remains under surveillance.
Discussion: Cystic PNETs are rare, and cystic variants may mimic IPMN especially when associated with MPD dilation. Of cystic PNETs described in the literature, the majority are located in the tail. CT and MRI are frequently used for initial evaluation of pancreatic cysts, but distinguishing cystic PNETs remains challenging. EUS-FNA plays a crucial role in diagnosis, especially when imaging reveals high-risk features. MPD dilation in PNETs is rare and may result from mass effect, or less commonly, ductal invasion. Our patient’s lesion showed interval growth, a solid component, and MPD involvement, prompting resection. Pathology showed lymphovascular invasion and borderline Ki-67, supporting the need for surgery. This case highlights the need to consider PNETs in cystic pancreatic lesion differentials and the value of multimodal assessment.
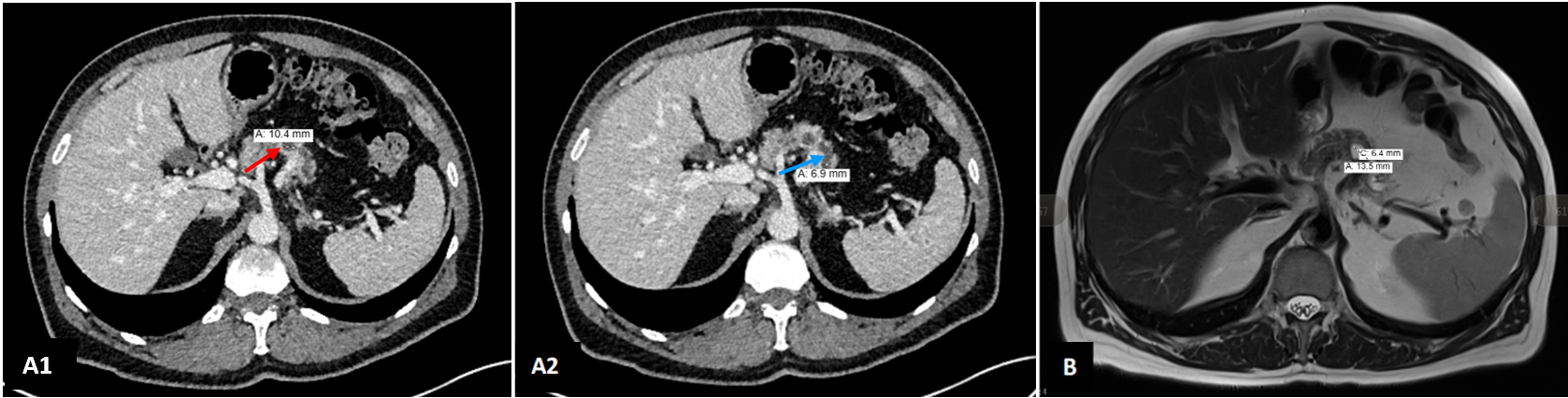
Figure: Figure 1: A1) Axial contrast-enhanced CT image showing a 10.4 mm cystic lesion in the pancreatic body (red arrow) A2) Axial CT image at a slightly lower level showing MPD dilation measuring 6.9 mm in diameter (blue arrow). B) Axial T2-weighted MRI showing 13.5 mm cystic lesion in the pancreatic body with associated upstream MPD measuring 6.4 mm.
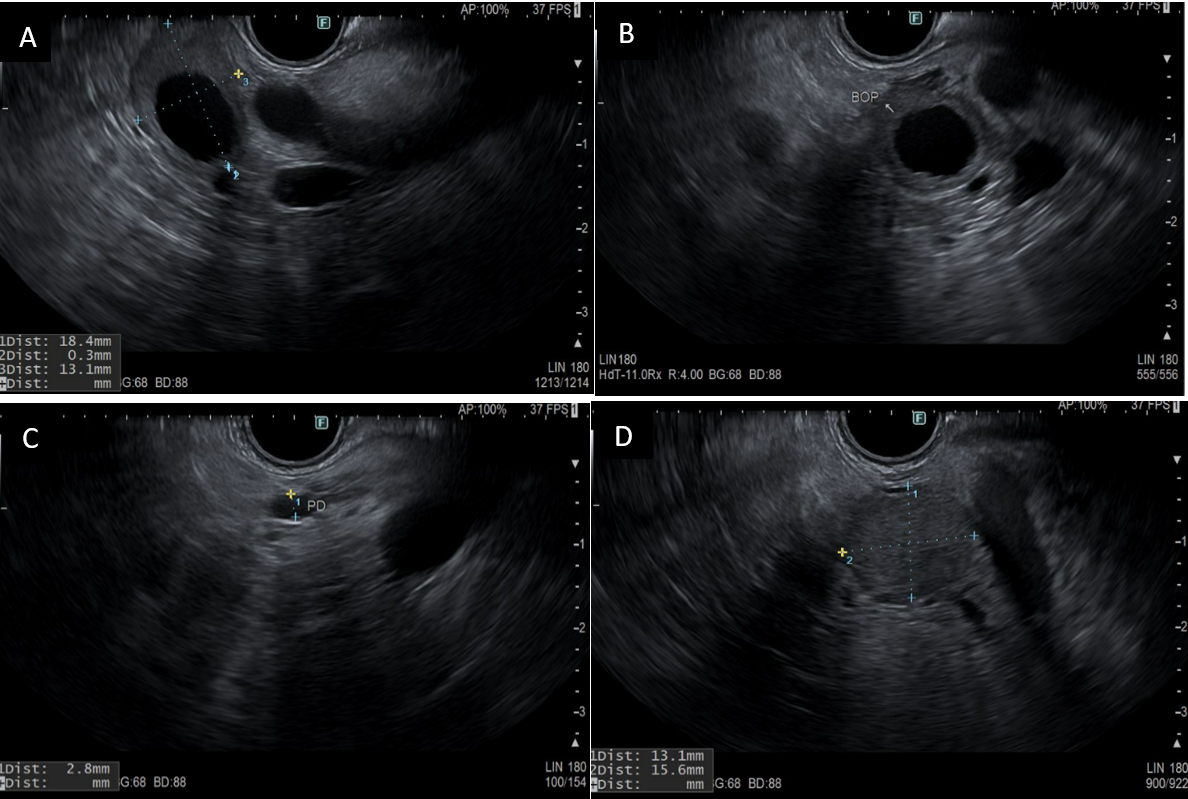
Figure: Figure 2. Endoscopic ultrasound (EUS) images demonstrating: (A, B) cystic component of the pancreatic neuroendocrine tumor (PNET); (C) dilatation of the main pancreatic duct; and (D) solid component of the PNET, delineated by calipers.
Disclosures:
Nikita Garg indicated no relevant financial relationships.
Miles Graves indicated no relevant financial relationships.
Tushar Abhinav indicated no relevant financial relationships.
John Appiah indicated no relevant financial relationships.
Danial Nadeem indicated no relevant financial relationships.
Amit Sohagia indicated no relevant financial relationships.
Nihaal Karnik indicated no relevant financial relationships.
Nikita Garg, MD1, Miles Graves, MD1, Tushar Abhinav, MD2, John K. Appiah, MD1, Danial Nadeem, MD1, Amit Sohagia, MD3, Nihaal Karnik, MD1. P2309 - An Uncommon Presentation of a Cystic Pancreatic Neuroendocrine Tumor With Main Duct Dilatation Mimicking Intraductal Papillary Mucinous Neoplasm: A Diagnostic Pitfall, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2The Wright Center for Graduate Medical Education, Wilkes-Barre, PA; 3Geisinger Community Medical Center, Scranton, PA
Introduction: While pancreatic neuroendocrine tumors (PNETs) are rare and typically solid, 10-20% may present as cystic, making cystic PNETs an uncommon diagnostic challenge. Of these, very few present with intraductal growth, and the ones described thus far are most typically located in the tail of the pancreas. We present a case of a cystic neuroendocrine tumor at the pancreatic body with main pancreatic duct (MPD) dilatation, radiologically mimicking an intraductal papillary mucinous neoplasm (IPMN).
Case Description/
Methods: A 66-year-old male presented with abdominal pain and constipation. Contrast-enhanced abdominal computed tomography (CT) revealed an incidental 1 cm cystic lesion in the pancreatic body with upstream main pancreatic duct dilation to 7 mm. Follow-up abdominal magnetic resonance imaging (MRI) showed a 1.4 cm cystic lesion with 6 mm ductal dilation and no mural nodule, radiologically suspicious for mixed-type IPMN. Given the MPD dilatation, an endoscopic ultrasound was performed. EUS identified a 2.0 x 1.4 cm cystic lesion with a solid component, prompting fine needle aspiration (FNA). Cytology revealed a well-differentiated grade 1 PNET, positive for CAM5.2 and synaptophysin, Ki-67 < 3%. Gallium-68 DOTATATE PET demonstrated somatostatin receptor–positive, localized disease (Stage I: pT1, cN0, cM0). After a multidisciplinary discussion, the decision was made for a surgical resection given the solid component, main duct dilation, and interval growth on surveillance imaging. Histopathology confirmed a grade 2 NET with lymphovascular invasion and R0 resection. The patient remains under surveillance.
Discussion: Cystic PNETs are rare, and cystic variants may mimic IPMN especially when associated with MPD dilation. Of cystic PNETs described in the literature, the majority are located in the tail. CT and MRI are frequently used for initial evaluation of pancreatic cysts, but distinguishing cystic PNETs remains challenging. EUS-FNA plays a crucial role in diagnosis, especially when imaging reveals high-risk features. MPD dilation in PNETs is rare and may result from mass effect, or less commonly, ductal invasion. Our patient’s lesion showed interval growth, a solid component, and MPD involvement, prompting resection. Pathology showed lymphovascular invasion and borderline Ki-67, supporting the need for surgery. This case highlights the need to consider PNETs in cystic pancreatic lesion differentials and the value of multimodal assessment.
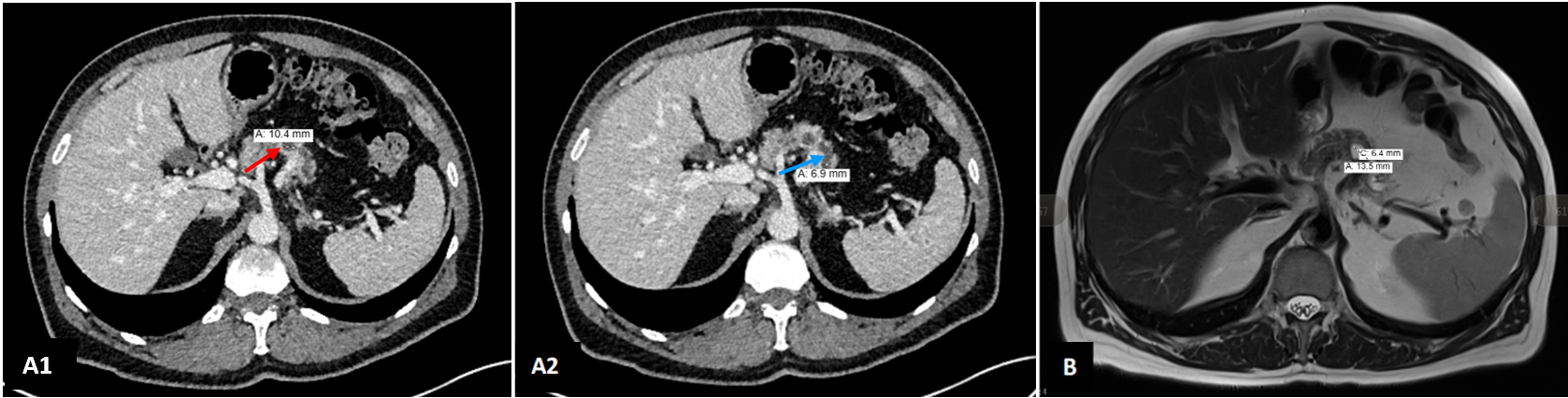
Figure: Figure 1: A1) Axial contrast-enhanced CT image showing a 10.4 mm cystic lesion in the pancreatic body (red arrow) A2) Axial CT image at a slightly lower level showing MPD dilation measuring 6.9 mm in diameter (blue arrow). B) Axial T2-weighted MRI showing 13.5 mm cystic lesion in the pancreatic body with associated upstream MPD measuring 6.4 mm.
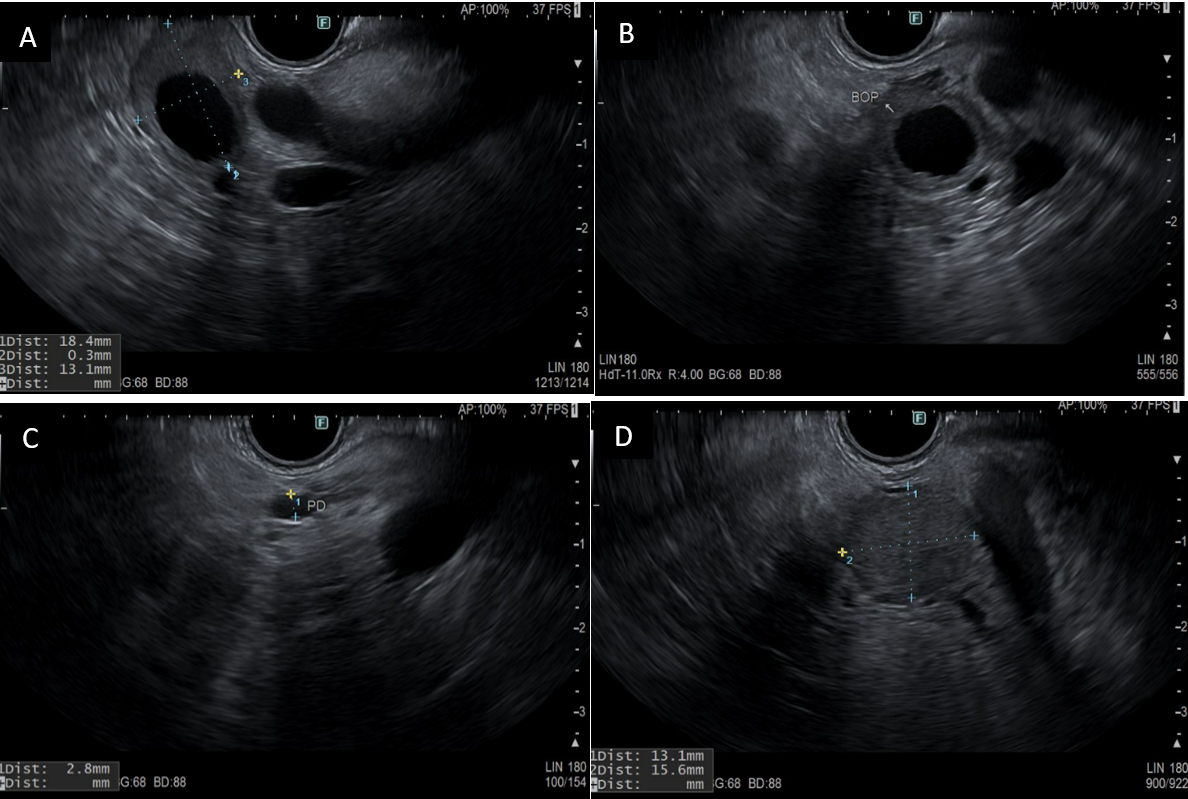
Figure: Figure 2. Endoscopic ultrasound (EUS) images demonstrating: (A, B) cystic component of the pancreatic neuroendocrine tumor (PNET); (C) dilatation of the main pancreatic duct; and (D) solid component of the PNET, delineated by calipers.
Disclosures:
Nikita Garg indicated no relevant financial relationships.
Miles Graves indicated no relevant financial relationships.
Tushar Abhinav indicated no relevant financial relationships.
John Appiah indicated no relevant financial relationships.
Danial Nadeem indicated no relevant financial relationships.
Amit Sohagia indicated no relevant financial relationships.
Nihaal Karnik indicated no relevant financial relationships.
Nikita Garg, MD1, Miles Graves, MD1, Tushar Abhinav, MD2, John K. Appiah, MD1, Danial Nadeem, MD1, Amit Sohagia, MD3, Nihaal Karnik, MD1. P2309 - An Uncommon Presentation of a Cystic Pancreatic Neuroendocrine Tumor With Main Duct Dilatation Mimicking Intraductal Papillary Mucinous Neoplasm: A Diagnostic Pitfall, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

