Monday Poster Session
Category: Biliary/Pancreas
P2304 - Endoscopic Treatment of Gallstone Ileus: A Feasible and Effective Non-Surgical Approach
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Pooja Viswanath, MS, DO
University of New Mexico Health Sciences Center
Albuquerque, NM
Presenting Author(s)
Pooja Viswanath, MS, DO1, Udita Gupta, MD1, Alan Gabriel. Ortega Macias, MD2, David Jarava, MD2, Nicholas Volpicelli, MD2
1University of New Mexico Health Sciences Center, Albuquerque, NM; 2University of New Mexico, Albuquerque, NM
Introduction: Gallstone ileus (GI) is a rare but serious complication of cholelithiasis, accounting for 1-4% of non-strangulating mechanical small bowel obstructions (SBO). GI occurs when a gallstone enters the gastrointestinal tract via a biliary-enteric fistula, causing luminal obstruction. Risk factors include recurrent cholecystitis and stones > 2 cm. Diagnosis is often delayed due to vague symptoms from “tumbling” stones. We present a complex case of GI successfully managed with endoscopic retrieval.
Case Description/
Methods: An 82-year-old male with emphysematous cholecystitis treated a month earlier with a percutaneous cholecystostomy tube (PCT) presented with abdominal pain, vomiting, and increased PCT output. Initial CT showed a well-positioned drain, fluid collection in gallbladder fossa and a cholecystoduodenal fistula. On hospital day 3, he developed worsening abdominal pain and obstipation, became hypotensive, and exhibited rising leukocytosis. Physical exam revealed abdominal distention, and high-pitched bowel sounds. Repeat CT revealed a 3.0 × 2.1cm gallstone in the distal small bowel, with associated pneumobilia and pneumatosis of small bowel loops suggestive of GI (Fig-1). Surgery was consulted but deferred due to patient’s comorbidities. Given the distal location of the stone, endoscopic management was attempted. Colonoscopy identified an impacted gallstone at the ileocecal valve, which was dislodged and removed with a snare (Fig-2). Examination of the terminal ileum showed no additional stones. Post-procedure, the patient’s bowel obstruction was resolved. Gallstone cultures grew resistant Klebsiella oxytoca, requiring meropenem. For fistula closure and source control, ERCP was performed; an occluding cystic duct stent and a common bile duct stent for drainage were placed. The PCT was removed prior to discharge, and the patient had no recurrence of obstruction. Six months later, repeat ERCP showed fistula resolution and stents were removed.
Discussion: GI is an uncommon but potentially fatal complication of gallstone disease. Rigler’s triad—pneumobilia, ectopic gallstone, and small bowel obstruction—is diagnostic but often incomplete. While traditional management involves enterolithotomy with or without cholecystectomy and fistula repair, data on endoscopic management of GI are limited. This case underscores the importance of early recognition and highlights the feasibility of endoscopic treatment, especially for distal small bowel obstructions and stones impacted at the ileocecal valve.
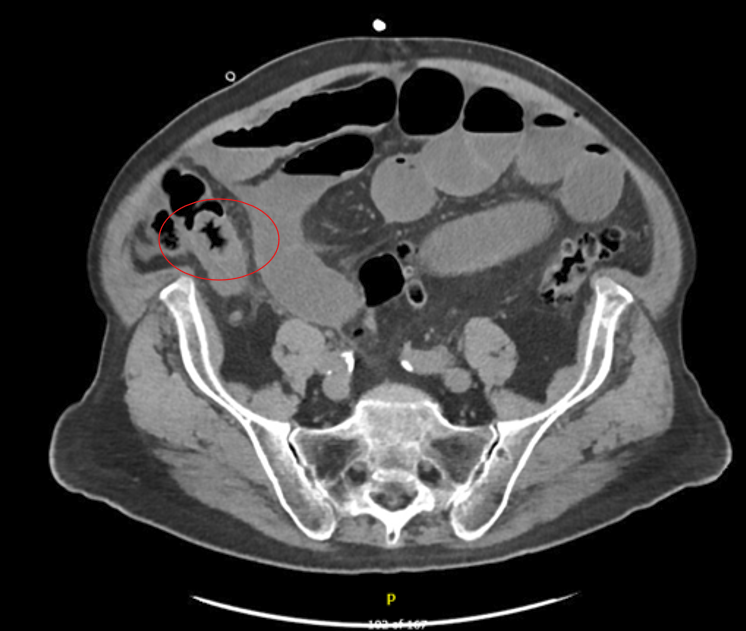
Figure: Figure 1: CT abdomen demonstrating "Gallstone Ileus" (3.0 x 2.1 cm gallstone in the distal small bowel with small bowel obstruction). Pneumatosis involving loops of small bowel in the right central abdomen with mesenteric edema. Pneumobilia.

Figure: Figure 2: Gallstone visualized at ileocecal valve during colonoscopy, dislodged and removed with snare.
Disclosures:
Pooja Viswanath indicated no relevant financial relationships.
Udita Gupta indicated no relevant financial relationships.
Alan Ortega Macias indicated no relevant financial relationships.
David Jarava indicated no relevant financial relationships.
Nicholas Volpicelli indicated no relevant financial relationships.
Pooja Viswanath, MS, DO1, Udita Gupta, MD1, Alan Gabriel. Ortega Macias, MD2, David Jarava, MD2, Nicholas Volpicelli, MD2. P2304 - Endoscopic Treatment of Gallstone Ileus: A Feasible and Effective Non-Surgical Approach, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of New Mexico Health Sciences Center, Albuquerque, NM; 2University of New Mexico, Albuquerque, NM
Introduction: Gallstone ileus (GI) is a rare but serious complication of cholelithiasis, accounting for 1-4% of non-strangulating mechanical small bowel obstructions (SBO). GI occurs when a gallstone enters the gastrointestinal tract via a biliary-enteric fistula, causing luminal obstruction. Risk factors include recurrent cholecystitis and stones > 2 cm. Diagnosis is often delayed due to vague symptoms from “tumbling” stones. We present a complex case of GI successfully managed with endoscopic retrieval.
Case Description/
Methods: An 82-year-old male with emphysematous cholecystitis treated a month earlier with a percutaneous cholecystostomy tube (PCT) presented with abdominal pain, vomiting, and increased PCT output. Initial CT showed a well-positioned drain, fluid collection in gallbladder fossa and a cholecystoduodenal fistula. On hospital day 3, he developed worsening abdominal pain and obstipation, became hypotensive, and exhibited rising leukocytosis. Physical exam revealed abdominal distention, and high-pitched bowel sounds. Repeat CT revealed a 3.0 × 2.1cm gallstone in the distal small bowel, with associated pneumobilia and pneumatosis of small bowel loops suggestive of GI (Fig-1). Surgery was consulted but deferred due to patient’s comorbidities. Given the distal location of the stone, endoscopic management was attempted. Colonoscopy identified an impacted gallstone at the ileocecal valve, which was dislodged and removed with a snare (Fig-2). Examination of the terminal ileum showed no additional stones. Post-procedure, the patient’s bowel obstruction was resolved. Gallstone cultures grew resistant Klebsiella oxytoca, requiring meropenem. For fistula closure and source control, ERCP was performed; an occluding cystic duct stent and a common bile duct stent for drainage were placed. The PCT was removed prior to discharge, and the patient had no recurrence of obstruction. Six months later, repeat ERCP showed fistula resolution and stents were removed.
Discussion: GI is an uncommon but potentially fatal complication of gallstone disease. Rigler’s triad—pneumobilia, ectopic gallstone, and small bowel obstruction—is diagnostic but often incomplete. While traditional management involves enterolithotomy with or without cholecystectomy and fistula repair, data on endoscopic management of GI are limited. This case underscores the importance of early recognition and highlights the feasibility of endoscopic treatment, especially for distal small bowel obstructions and stones impacted at the ileocecal valve.
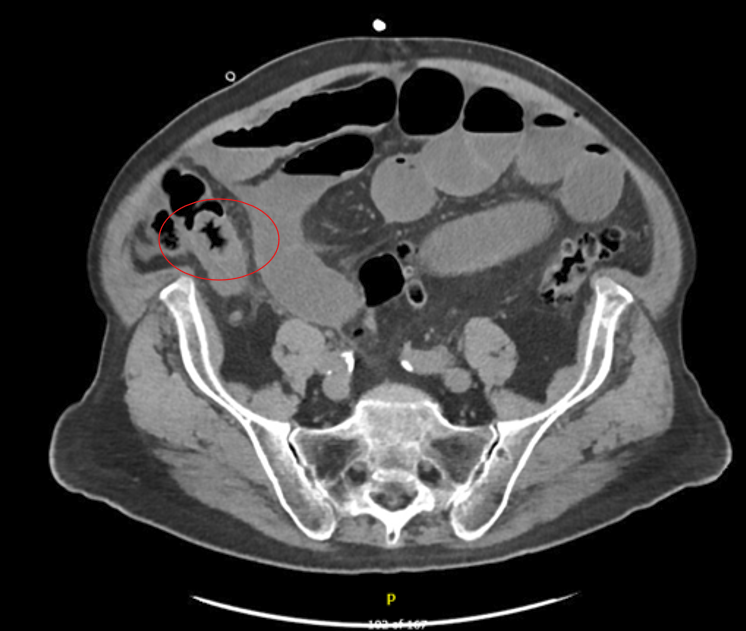
Figure: Figure 1: CT abdomen demonstrating "Gallstone Ileus" (3.0 x 2.1 cm gallstone in the distal small bowel with small bowel obstruction). Pneumatosis involving loops of small bowel in the right central abdomen with mesenteric edema. Pneumobilia.

Figure: Figure 2: Gallstone visualized at ileocecal valve during colonoscopy, dislodged and removed with snare.
Disclosures:
Pooja Viswanath indicated no relevant financial relationships.
Udita Gupta indicated no relevant financial relationships.
Alan Ortega Macias indicated no relevant financial relationships.
David Jarava indicated no relevant financial relationships.
Nicholas Volpicelli indicated no relevant financial relationships.
Pooja Viswanath, MS, DO1, Udita Gupta, MD1, Alan Gabriel. Ortega Macias, MD2, David Jarava, MD2, Nicholas Volpicelli, MD2. P2304 - Endoscopic Treatment of Gallstone Ileus: A Feasible and Effective Non-Surgical Approach, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
