Monday Poster Session
Category: Biliary/Pancreas
P2303 - A Rare Case of Biliary Obstruction Caused by Diffuse Large B-Cell Lymphoma
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Christina Sisliyan, DO
Olive View-UCLA Medical Center
Los Angeles, CA
Presenting Author(s)
Christina Sisliyan, DO1, Mark R. Baniqued, MD1, Sneha Dodaballapur, MD2, Eeman Khorramian, MD3
1Olive View-UCLA Medical Center, Los Angeles, CA; 2Olive View-UCLA Medical Center, Van Nuys, CA; 3Olive View-UCLA Medical Center, Sylmar, CA
Introduction: Biliary obstruction is most commonly caused by gallstones, strictures, pancreatic or biliary malignancies. Invasion by lymphoma is rare. In one study, lymphoma accounted for only 0.6% of cases of biliary obstruction. Diffuse large B-cell lymphoma (DLBCL) is the main subtype of Non-Hodgkin lymphoma (NHL). The gastrointestinal (GI) tract is the primary site of extranodal NHL, and is often linked to a poor prognosis. We present a case of biliary obstruction caused by biopsy-confirmed high-grade DLBCL.
Case Description/
Methods: A 55-year-old male with no past medical history presented with jaundice, melena, fever and weight loss over three weeks. On arrival, he was tachycardic and labs showed transaminitis with direct hyperbilirubinemia, anemia, and elevated INR. CT of the abdomen and pelvis found a 17 cm mass [Figure 1]. Due to the melena, Gastroenterology recommended esophagogastroduodenoscopy (EGD) to evaluate for tumor bleeding and diagnostic biopsies. He was started on a proton pump inhibitor (PPI) twice daily. EGD showed an invasive gastric mass [Figure 2]. The biopsies showed advanced DLBCL confirmed by chromosomal studies. Due to hepatic insufficiency, biliary decompression was recommended but a target was not found for percutaneous drainage. Gastroenterology planned to relieve the obstruction with stenting via endoscopic retrograde cholangiopancreatography (ERCP). An abdominal MRI was performed to delineate the anatomy and showed extensive infiltration and obstruction of multiple bile ducts. ERCP was deferred due to high perforation risk. Oncology postponed standard chemotherapy due to hepatically metabolized agents. Steroids and cycle one of Rituxan were started followed by a non-traditional regimen of gemcitabine and oxaliplatin. He tolerated chemotherapy and was discharged with Oncology follow-up. On discharge, melena had resolved, and plan was to continue PPI twice daily.
Discussion: GI DLBCL can present with abdominal pain, B-symptoms, and mild bleeding due to its ulcerative features. Severe symptoms like obstruction, perforation, or profuse bleeding signify advanced disease. PPIs protect the gastric mucosa to prevent significant bleeding. Endoscopy is diagnostic but often delayed until severe symptoms present, limiting treatment and interventions. Timely symptom recognition prompts diagnostics, like EGD and endoscopic ultrasound, to facilitate early disease detection. ERCP interventions can then be pursued with fewer complication risks, enhancing subsequent chemotherapy efficacy.
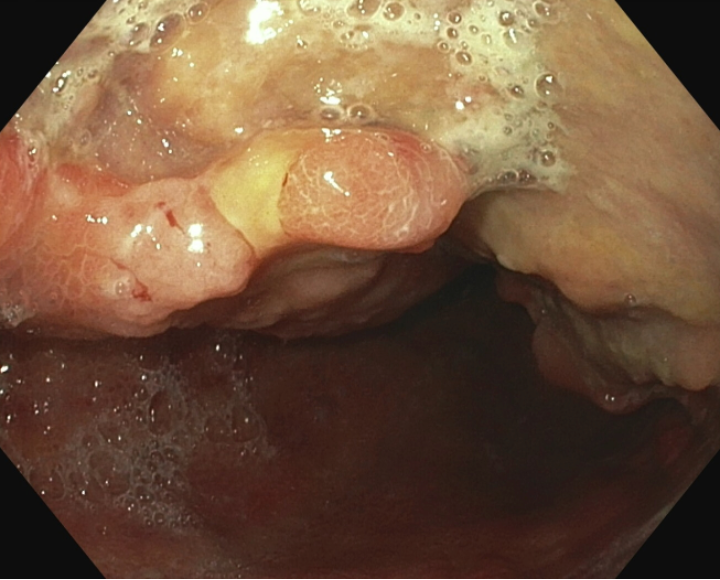
Figure: Figure 1A: Large mass with areas of internal necrosis extends from the left hepatic lobe to the lesser curvature of the stomach and spans from the anterior abdomen to the front of the abdominal aorta, measuring 17 x 11 x 10 cm. 1B: The mass involves the gallbladder, pancreas, stomach, and surrounding vessels. Intrahepatic bile duct dilation measuring up to 7 mm is noted in the right hepatic lobe.
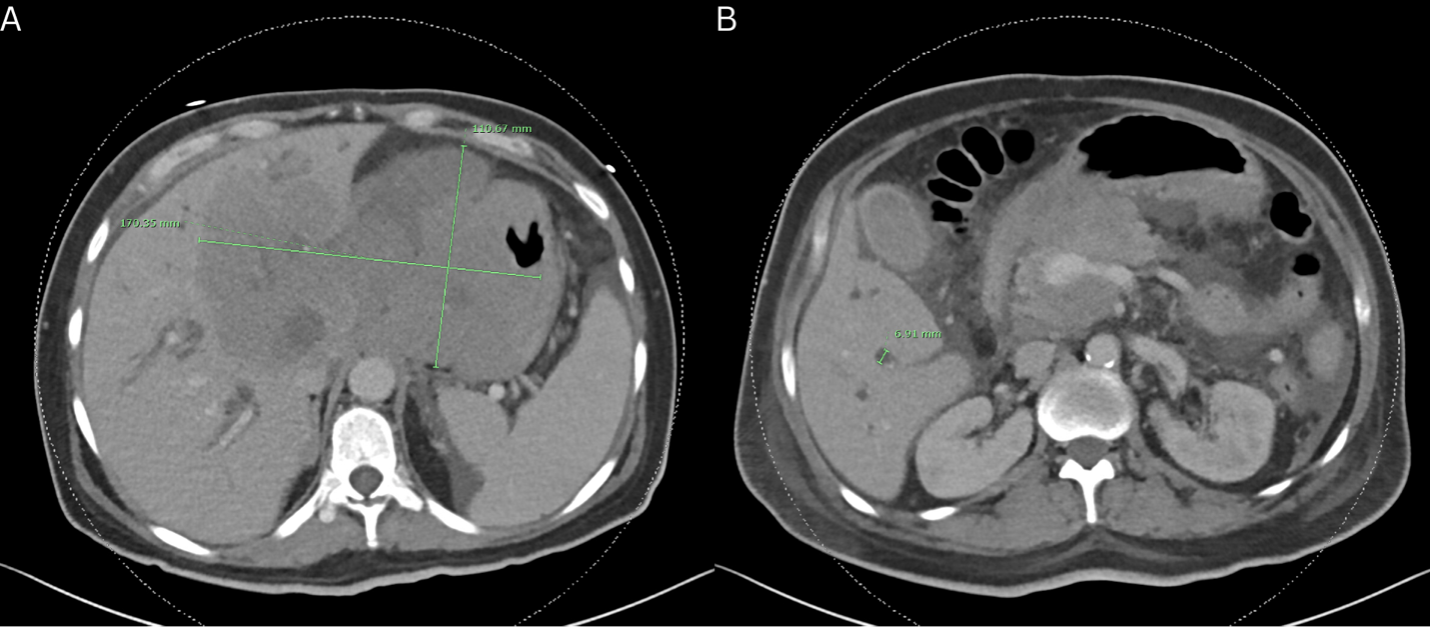
Figure: Figure 2: EGD shows protruding lesions in the stomach. A large infiltrative, ulcerated, fungating, and necrotic mass with a malignant appearance was found in the body of the stomach. The mass was hemi-circumferential along the lesser curve and anterior wall. The scope traversed the lesion.
Disclosures:
Christina Sisliyan indicated no relevant financial relationships.
Mark Baniqued indicated no relevant financial relationships.
Sneha Dodaballapur indicated no relevant financial relationships.
Eeman Khorramian indicated no relevant financial relationships.
Christina Sisliyan, DO1, Mark R. Baniqued, MD1, Sneha Dodaballapur, MD2, Eeman Khorramian, MD3. P2303 - A Rare Case of Biliary Obstruction Caused by Diffuse Large B-Cell Lymphoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Olive View-UCLA Medical Center, Los Angeles, CA; 2Olive View-UCLA Medical Center, Van Nuys, CA; 3Olive View-UCLA Medical Center, Sylmar, CA
Introduction: Biliary obstruction is most commonly caused by gallstones, strictures, pancreatic or biliary malignancies. Invasion by lymphoma is rare. In one study, lymphoma accounted for only 0.6% of cases of biliary obstruction. Diffuse large B-cell lymphoma (DLBCL) is the main subtype of Non-Hodgkin lymphoma (NHL). The gastrointestinal (GI) tract is the primary site of extranodal NHL, and is often linked to a poor prognosis. We present a case of biliary obstruction caused by biopsy-confirmed high-grade DLBCL.
Case Description/
Methods: A 55-year-old male with no past medical history presented with jaundice, melena, fever and weight loss over three weeks. On arrival, he was tachycardic and labs showed transaminitis with direct hyperbilirubinemia, anemia, and elevated INR. CT of the abdomen and pelvis found a 17 cm mass [Figure 1]. Due to the melena, Gastroenterology recommended esophagogastroduodenoscopy (EGD) to evaluate for tumor bleeding and diagnostic biopsies. He was started on a proton pump inhibitor (PPI) twice daily. EGD showed an invasive gastric mass [Figure 2]. The biopsies showed advanced DLBCL confirmed by chromosomal studies. Due to hepatic insufficiency, biliary decompression was recommended but a target was not found for percutaneous drainage. Gastroenterology planned to relieve the obstruction with stenting via endoscopic retrograde cholangiopancreatography (ERCP). An abdominal MRI was performed to delineate the anatomy and showed extensive infiltration and obstruction of multiple bile ducts. ERCP was deferred due to high perforation risk. Oncology postponed standard chemotherapy due to hepatically metabolized agents. Steroids and cycle one of Rituxan were started followed by a non-traditional regimen of gemcitabine and oxaliplatin. He tolerated chemotherapy and was discharged with Oncology follow-up. On discharge, melena had resolved, and plan was to continue PPI twice daily.
Discussion: GI DLBCL can present with abdominal pain, B-symptoms, and mild bleeding due to its ulcerative features. Severe symptoms like obstruction, perforation, or profuse bleeding signify advanced disease. PPIs protect the gastric mucosa to prevent significant bleeding. Endoscopy is diagnostic but often delayed until severe symptoms present, limiting treatment and interventions. Timely symptom recognition prompts diagnostics, like EGD and endoscopic ultrasound, to facilitate early disease detection. ERCP interventions can then be pursued with fewer complication risks, enhancing subsequent chemotherapy efficacy.
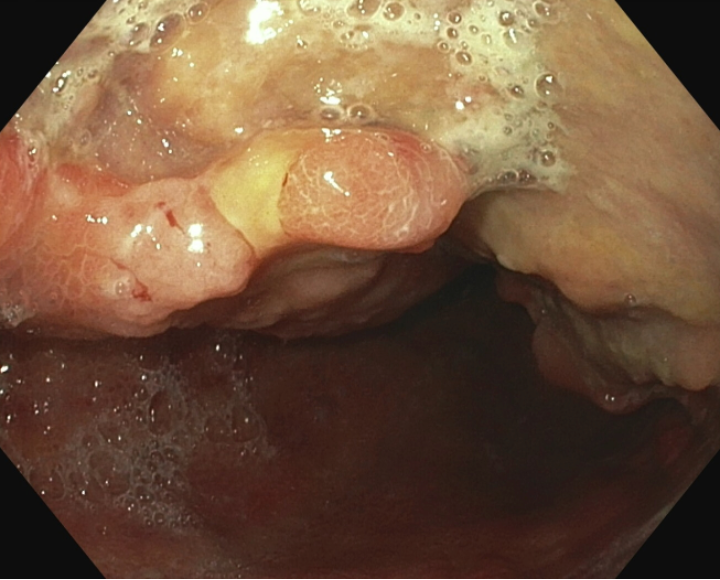
Figure: Figure 1A: Large mass with areas of internal necrosis extends from the left hepatic lobe to the lesser curvature of the stomach and spans from the anterior abdomen to the front of the abdominal aorta, measuring 17 x 11 x 10 cm. 1B: The mass involves the gallbladder, pancreas, stomach, and surrounding vessels. Intrahepatic bile duct dilation measuring up to 7 mm is noted in the right hepatic lobe.
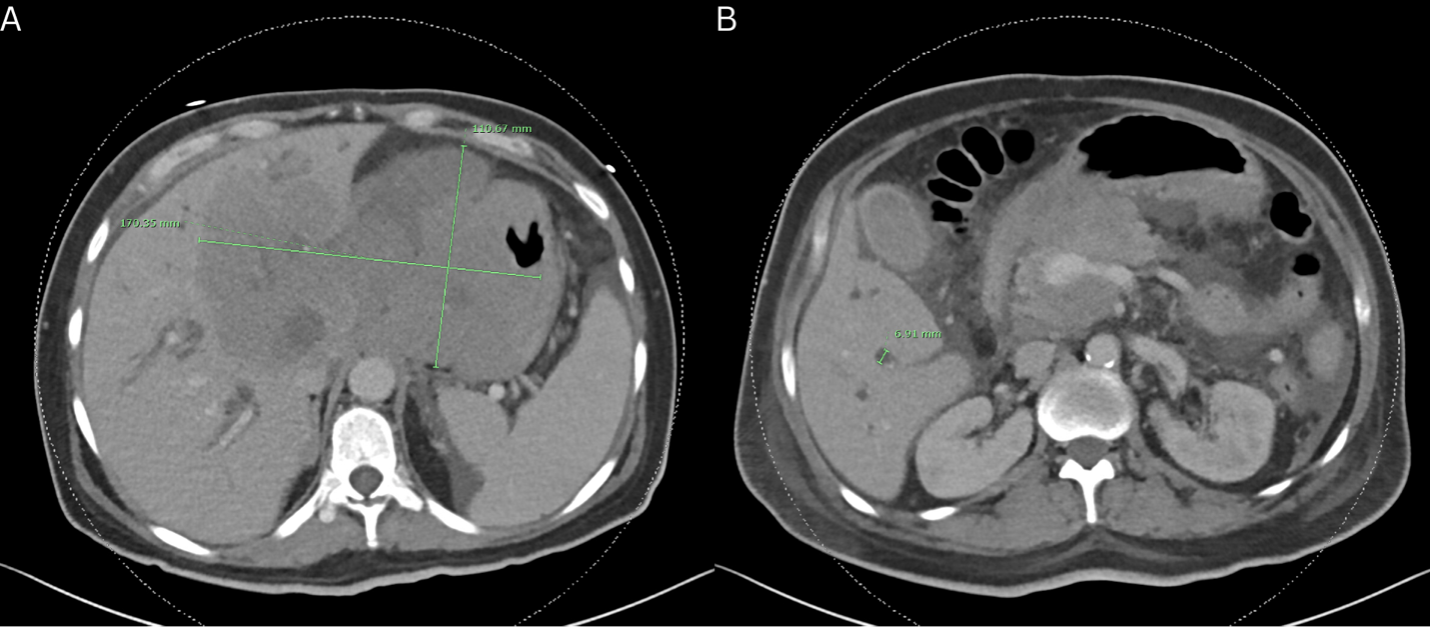
Figure: Figure 2: EGD shows protruding lesions in the stomach. A large infiltrative, ulcerated, fungating, and necrotic mass with a malignant appearance was found in the body of the stomach. The mass was hemi-circumferential along the lesser curve and anterior wall. The scope traversed the lesion.
Disclosures:
Christina Sisliyan indicated no relevant financial relationships.
Mark Baniqued indicated no relevant financial relationships.
Sneha Dodaballapur indicated no relevant financial relationships.
Eeman Khorramian indicated no relevant financial relationships.
Christina Sisliyan, DO1, Mark R. Baniqued, MD1, Sneha Dodaballapur, MD2, Eeman Khorramian, MD3. P2303 - A Rare Case of Biliary Obstruction Caused by Diffuse Large B-Cell Lymphoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
