Monday Poster Session
Category: Biliary/Pancreas
P2296 - When Pancreatic Cyst Rupture Leads to Cytokine Storm: A Case of Secondary Hemophagocytic Lymphohistiocytosis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Lauren Healey, DO (she/her/hers)
University of South Alabama
Mobile, AL
Presenting Author(s)
Lauren Healey, DO1, Hobie L. Hughes, DO2, Katherine Glosemeyer, MD1
1University of South Alabama, Mobile, AL; 2Thomas Hospital, Fairhope, AL
Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a severe hyper-inflammatory syndrome that is caused by aberrantly activated cytotoxic T cells and macrophages that can result in multi-organ failure. The acquired form of HLH, or secondary HLH, is typically triggered by infection or malignancy. This hyper-inflammatory reaction presents with findings of high fever, splenomegaly, cytopenia, elevated aminotransferase, and ferritin. It can also cause coagulopathy, presenting a dilemma for management in a patient with an acute episode of gastrointestinal bleeding.
Case Description/
Methods: A 45-year-old female with past medical history significant for end-stage renal disease on dialysis, Systemic Lupus Erythematosus, and previous deep vein thrombus on Eliquis presented for spontaneous bleeding from her left upper extremity AV graft. Bleeding was able to be controlled with a hemostatic dressing; however, she ultimately went for right upper extremity graft revision. She was noted to have anemia on admission, which was attributed to her chronic kidney disease. However, it was noted her hemoglobin was trending down throughout her hospitalization. Initially, it was thought to be iatrogenic as she was getting frequent blood draws, but it continued to trend down following spacing out of labs. She had an episode of melena, so a computed tomography angiography with gastrointestinal protocol was ordered to rule out gastrointestinal bleeding. Initially, the scan was read as negative for acute bleeding, however on re-evaluation, bleeding was noted from a pancreatic cyst. She underwent embolization with interventional radiology. She continued to have episodes of melena with bi-cytopenia with anemia and thrombocytopenia that was refractory to transfusions. HLH workup was initiated, and she was found to meet criteria with a ferritin of 16500, fibrinogen of 154, triglycerides of 207, and recurrent fevers. Bone marrow biopsy pathology showed hemophagocytosis. She was ultimately transitioned to hospice care as the bleeding was unable to be controlled.
Discussion: This is a case of a patient with an autoimmune disorder, SLE, who had pancreatic cysts rupture leading to HLH. When a pancreatic cyst ruptures, it can release inflammatory markers, causing immune activation. In patients with underlying autoimmune conditions, rupture of cysts can cause catastrophic immune responses, as seen in this patient. It is especially important to keep HLH on the differential for patients who are critically ill and transfusion refractory.

Figure: Figure 1: Pancreatic Fluid Collection Prior to Drop in Hemoglobin
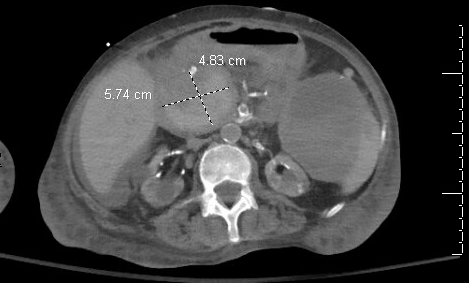
Figure: Figure 2: Pancreatic Fluid Collection After Drop in Hemoglobin Internal Hyperattenuation Likely Representing Blood
Disclosures:
Lauren Healey indicated no relevant financial relationships.
Hobie Hughes indicated no relevant financial relationships.
Katherine Glosemeyer indicated no relevant financial relationships.
Lauren Healey, DO1, Hobie L. Hughes, DO2, Katherine Glosemeyer, MD1. P2296 - When Pancreatic Cyst Rupture Leads to Cytokine Storm: A Case of Secondary Hemophagocytic Lymphohistiocytosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of South Alabama, Mobile, AL; 2Thomas Hospital, Fairhope, AL
Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a severe hyper-inflammatory syndrome that is caused by aberrantly activated cytotoxic T cells and macrophages that can result in multi-organ failure. The acquired form of HLH, or secondary HLH, is typically triggered by infection or malignancy. This hyper-inflammatory reaction presents with findings of high fever, splenomegaly, cytopenia, elevated aminotransferase, and ferritin. It can also cause coagulopathy, presenting a dilemma for management in a patient with an acute episode of gastrointestinal bleeding.
Case Description/
Methods: A 45-year-old female with past medical history significant for end-stage renal disease on dialysis, Systemic Lupus Erythematosus, and previous deep vein thrombus on Eliquis presented for spontaneous bleeding from her left upper extremity AV graft. Bleeding was able to be controlled with a hemostatic dressing; however, she ultimately went for right upper extremity graft revision. She was noted to have anemia on admission, which was attributed to her chronic kidney disease. However, it was noted her hemoglobin was trending down throughout her hospitalization. Initially, it was thought to be iatrogenic as she was getting frequent blood draws, but it continued to trend down following spacing out of labs. She had an episode of melena, so a computed tomography angiography with gastrointestinal protocol was ordered to rule out gastrointestinal bleeding. Initially, the scan was read as negative for acute bleeding, however on re-evaluation, bleeding was noted from a pancreatic cyst. She underwent embolization with interventional radiology. She continued to have episodes of melena with bi-cytopenia with anemia and thrombocytopenia that was refractory to transfusions. HLH workup was initiated, and she was found to meet criteria with a ferritin of 16500, fibrinogen of 154, triglycerides of 207, and recurrent fevers. Bone marrow biopsy pathology showed hemophagocytosis. She was ultimately transitioned to hospice care as the bleeding was unable to be controlled.
Discussion: This is a case of a patient with an autoimmune disorder, SLE, who had pancreatic cysts rupture leading to HLH. When a pancreatic cyst ruptures, it can release inflammatory markers, causing immune activation. In patients with underlying autoimmune conditions, rupture of cysts can cause catastrophic immune responses, as seen in this patient. It is especially important to keep HLH on the differential for patients who are critically ill and transfusion refractory.

Figure: Figure 1: Pancreatic Fluid Collection Prior to Drop in Hemoglobin
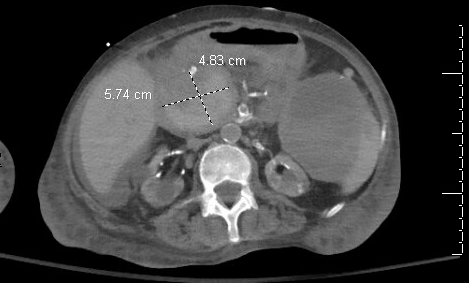
Figure: Figure 2: Pancreatic Fluid Collection After Drop in Hemoglobin Internal Hyperattenuation Likely Representing Blood
Disclosures:
Lauren Healey indicated no relevant financial relationships.
Hobie Hughes indicated no relevant financial relationships.
Katherine Glosemeyer indicated no relevant financial relationships.
Lauren Healey, DO1, Hobie L. Hughes, DO2, Katherine Glosemeyer, MD1. P2296 - When Pancreatic Cyst Rupture Leads to Cytokine Storm: A Case of Secondary Hemophagocytic Lymphohistiocytosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
