Monday Poster Session
Category: Biliary/Pancreas
P2287 - Solid Pseudopapillary Neoplasm of the Pancreas: A Case Report
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nikolay Lifshaz, DO
HCA Healthcare
Overland Park, KS
Presenting Author(s)
Nikolay Lifshaz, DO, Shruti Verma, MD, Syed F. Jafri, MD
HCA Healthcare, Overland Park, KS
Introduction: Pancreatic Solid Pseudopapillary Neoplasm (pSPN) is a benign form of pancreatic neoplasm usually seen in young females. In contrast to the 1-2% survival rate of pancreatic carcinomas, the prognosis of pSPN is excellent with a 5-year survival rate of 97%. Here we present a unique case of pancreatic pseudopapillary neoplasm treated with resection.
Case Description/
Methods: A 20-year-old female with poorly controlled Type 1 Diabetes presented with epigastric and left upper quadrant abdominal pain radiating to the chest for two days. She endorsed insulin non-compliance for the last 3 months. Initial labs revealed a WBC 12.5, lipase 110, HbA1C 11.5, normal LFTs and lipid profile. CT scan of the abdomen and pelvis with contrast revealed a large complex cystic mass measuring 12.2 x 9.6 x 9.8 cm along the superior aspect of the pancreatic tail and focal fatty infiltration of the liver. CA 19-9 levels were normal at 41.4. Subsequent upper EUS revealed a cystic mass on the pancreatic tail suggestive of a serous cystadenoma or pseudopapillary cystic adenoma. FNA was performed and cytological analysis showed moderate cellular smears with groups and clusters of crowded epithelioid cells with minimal atypia. IHC staining for the evaluation of neoplastic cells showed positivity for Ꞵ-catenin, CD10, CD56, Progesterone receptor, Synaptophysin and Chromogranin. Histologic and IHC findings were consistent with pSPN. Open surgical distal pancreatectomy with en-bloc splenectomy was completed leading to subsequent symptom resolution. (Figures A&B)
Discussion: pSPN is an exocrine neoplasm that is found to be 10 times more common in females compared to males, especially in the ages of 20-40 years. pSPN are often asymptomatic in most patients however can present with abdominal pain, distension, palpable mass, nausea/vomiting, back pain, weight loss, or jaundice. Immunochemistry evaluation is an invaluable diagnostic technique to distinguish pSPN from other pancreatic neoplasms including neuroendocrine tumors, pancreatoblastoma, and acinar cell carcinoma. This case demonstrates the value of utilizing a comprehensive array of histological evaluation when pSPN is considered among the differential diagnoses and prevent delay of curative treatment via complete surgical resection.
References
Cruz MAA et al. Solid Pseudopapillary Neoplasm of the Pancreas: Unfolding an Intriguing Condition. GE Port J Gastroenterol. 2021 Nov 19;29(3):151-162. doi: 10.1159/000519933. PMID: 35702168; PMCID: PMC9149554
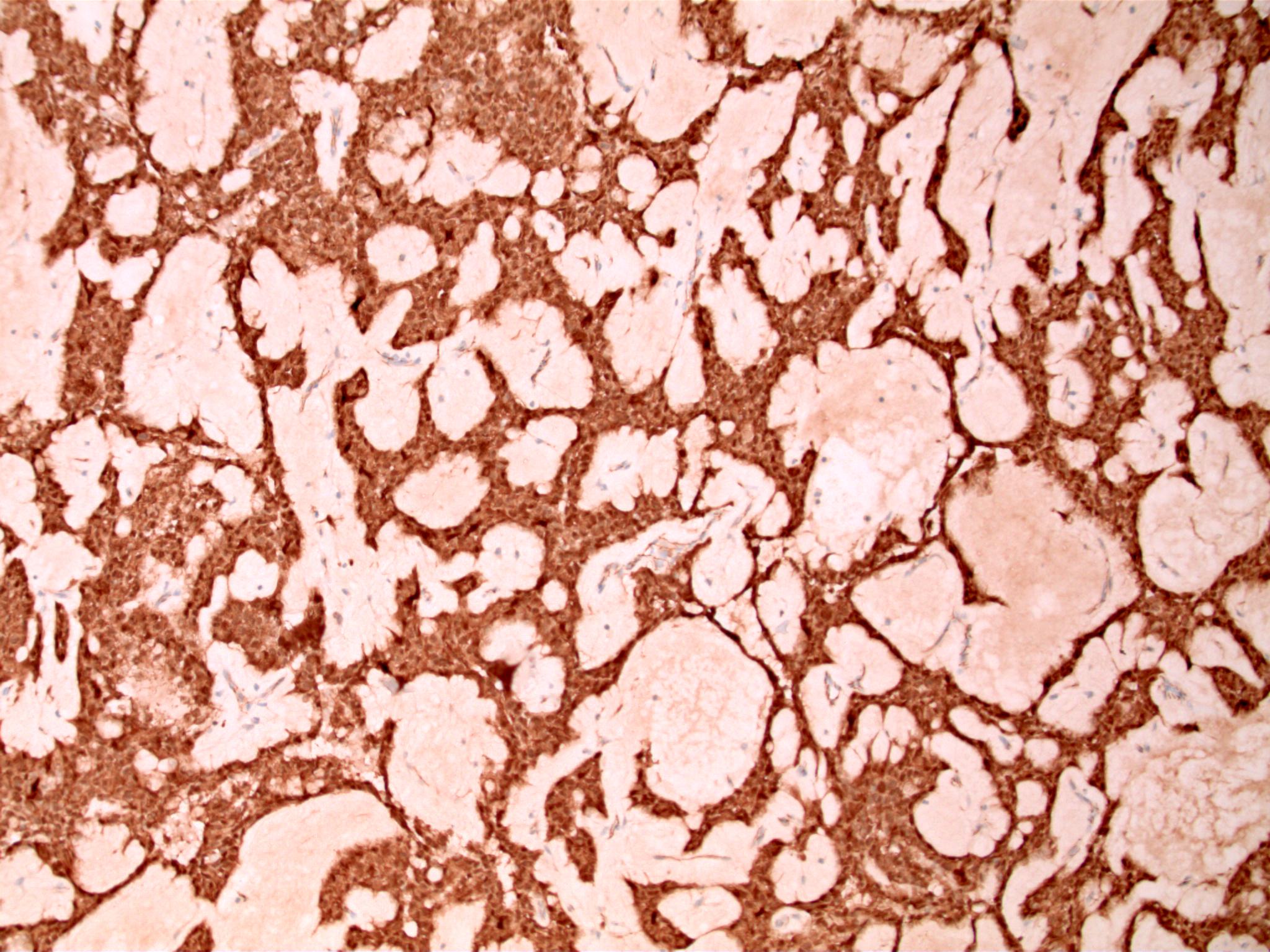
Figure: A) High power histological cross-section of pancreatic mass
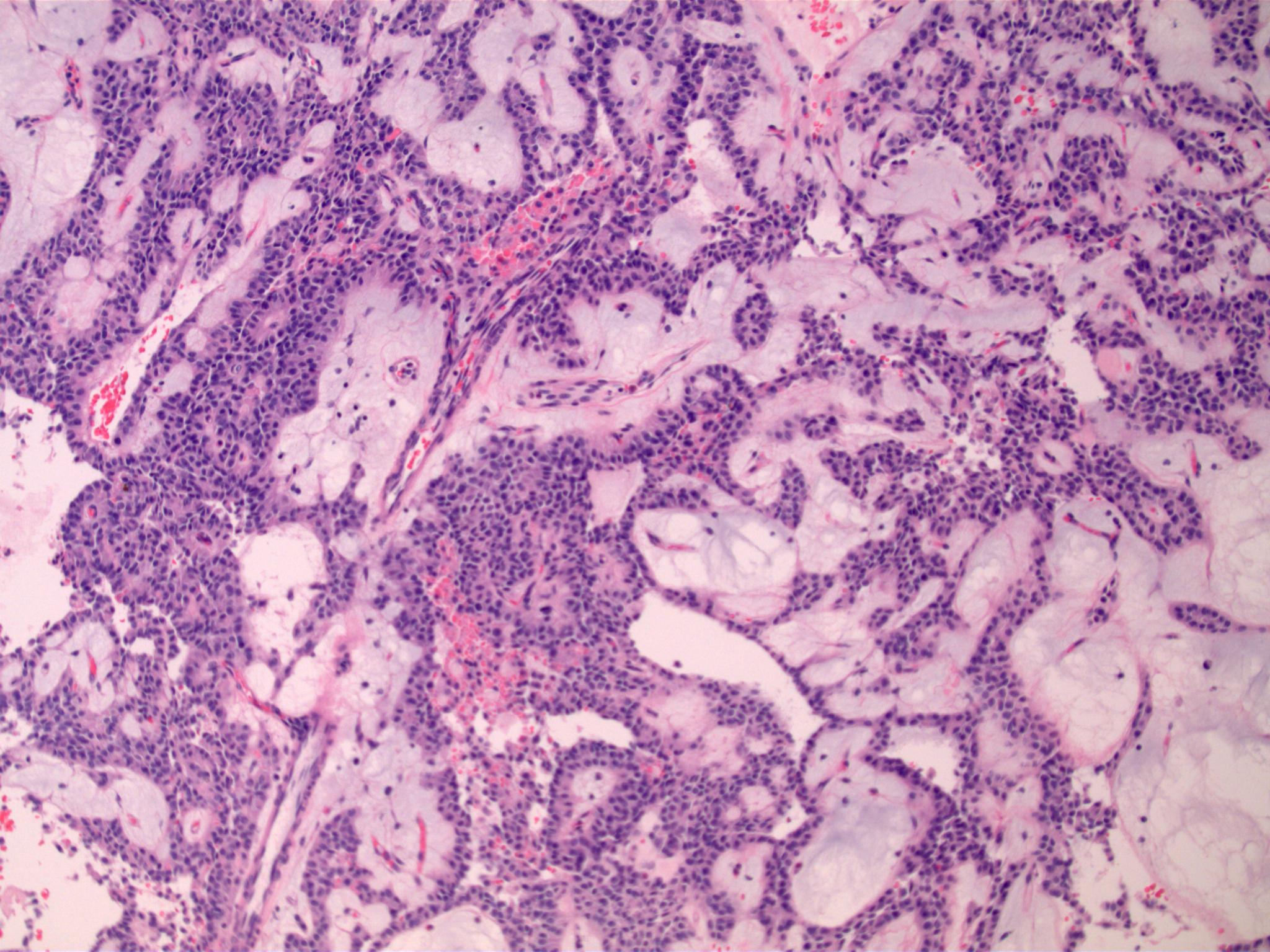
Figure: B) Beta-catenin positive staining of pancreatic mass aspirate
Disclosures:
Nikolay Lifshaz indicated no relevant financial relationships.
Shruti Verma indicated no relevant financial relationships.
Syed F. Jafri indicated no relevant financial relationships.
Nikolay Lifshaz, DO, Shruti Verma, MD, Syed F. Jafri, MD. P2287 - Solid Pseudopapillary Neoplasm of the Pancreas: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
HCA Healthcare, Overland Park, KS
Introduction: Pancreatic Solid Pseudopapillary Neoplasm (pSPN) is a benign form of pancreatic neoplasm usually seen in young females. In contrast to the 1-2% survival rate of pancreatic carcinomas, the prognosis of pSPN is excellent with a 5-year survival rate of 97%. Here we present a unique case of pancreatic pseudopapillary neoplasm treated with resection.
Case Description/
Methods: A 20-year-old female with poorly controlled Type 1 Diabetes presented with epigastric and left upper quadrant abdominal pain radiating to the chest for two days. She endorsed insulin non-compliance for the last 3 months. Initial labs revealed a WBC 12.5, lipase 110, HbA1C 11.5, normal LFTs and lipid profile. CT scan of the abdomen and pelvis with contrast revealed a large complex cystic mass measuring 12.2 x 9.6 x 9.8 cm along the superior aspect of the pancreatic tail and focal fatty infiltration of the liver. CA 19-9 levels were normal at 41.4. Subsequent upper EUS revealed a cystic mass on the pancreatic tail suggestive of a serous cystadenoma or pseudopapillary cystic adenoma. FNA was performed and cytological analysis showed moderate cellular smears with groups and clusters of crowded epithelioid cells with minimal atypia. IHC staining for the evaluation of neoplastic cells showed positivity for Ꞵ-catenin, CD10, CD56, Progesterone receptor, Synaptophysin and Chromogranin. Histologic and IHC findings were consistent with pSPN. Open surgical distal pancreatectomy with en-bloc splenectomy was completed leading to subsequent symptom resolution. (Figures A&B)
Discussion: pSPN is an exocrine neoplasm that is found to be 10 times more common in females compared to males, especially in the ages of 20-40 years. pSPN are often asymptomatic in most patients however can present with abdominal pain, distension, palpable mass, nausea/vomiting, back pain, weight loss, or jaundice. Immunochemistry evaluation is an invaluable diagnostic technique to distinguish pSPN from other pancreatic neoplasms including neuroendocrine tumors, pancreatoblastoma, and acinar cell carcinoma. This case demonstrates the value of utilizing a comprehensive array of histological evaluation when pSPN is considered among the differential diagnoses and prevent delay of curative treatment via complete surgical resection.
References
Cruz MAA et al. Solid Pseudopapillary Neoplasm of the Pancreas: Unfolding an Intriguing Condition. GE Port J Gastroenterol. 2021 Nov 19;29(3):151-162. doi: 10.1159/000519933. PMID: 35702168; PMCID: PMC9149554
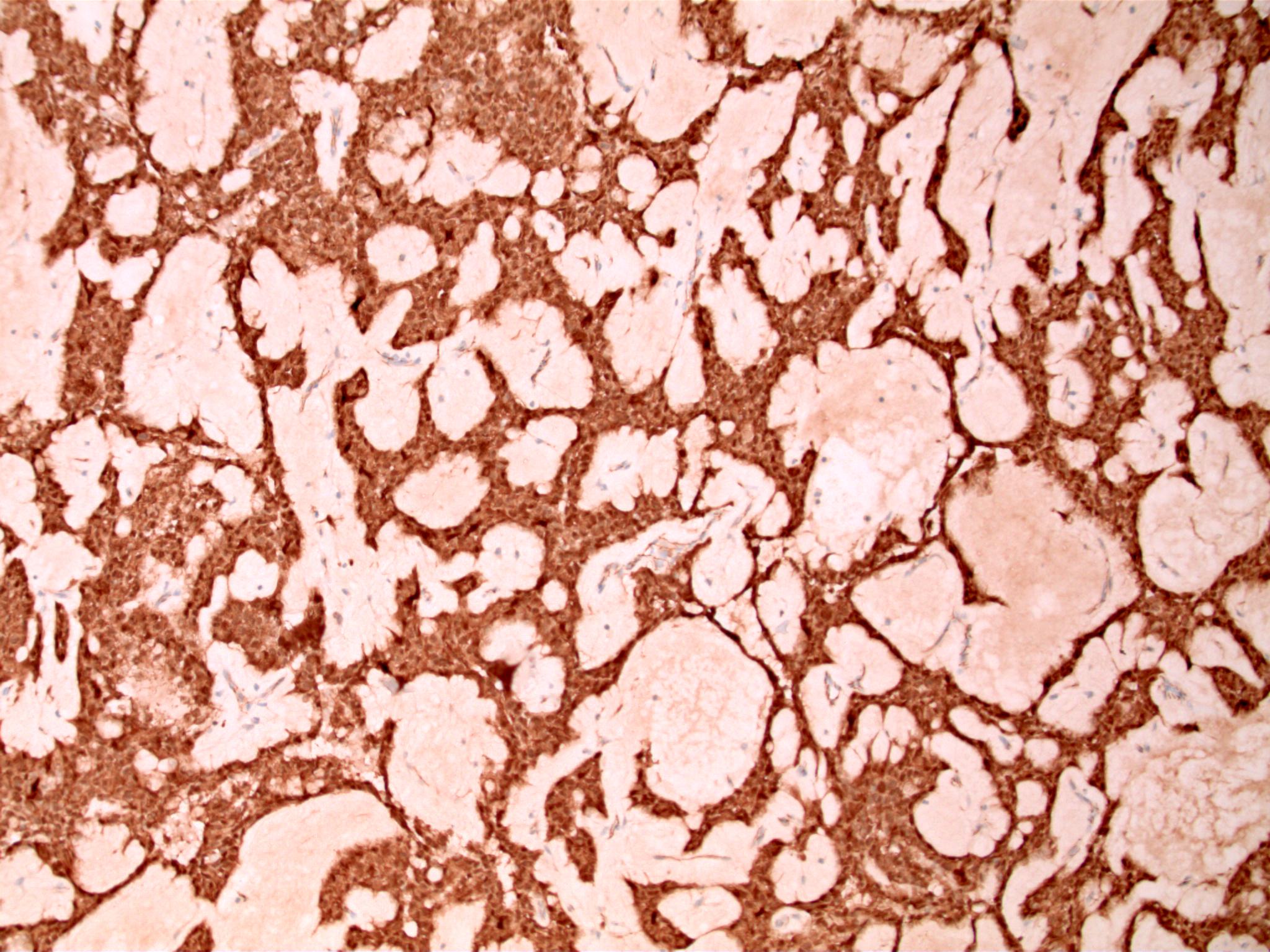
Figure: A) High power histological cross-section of pancreatic mass
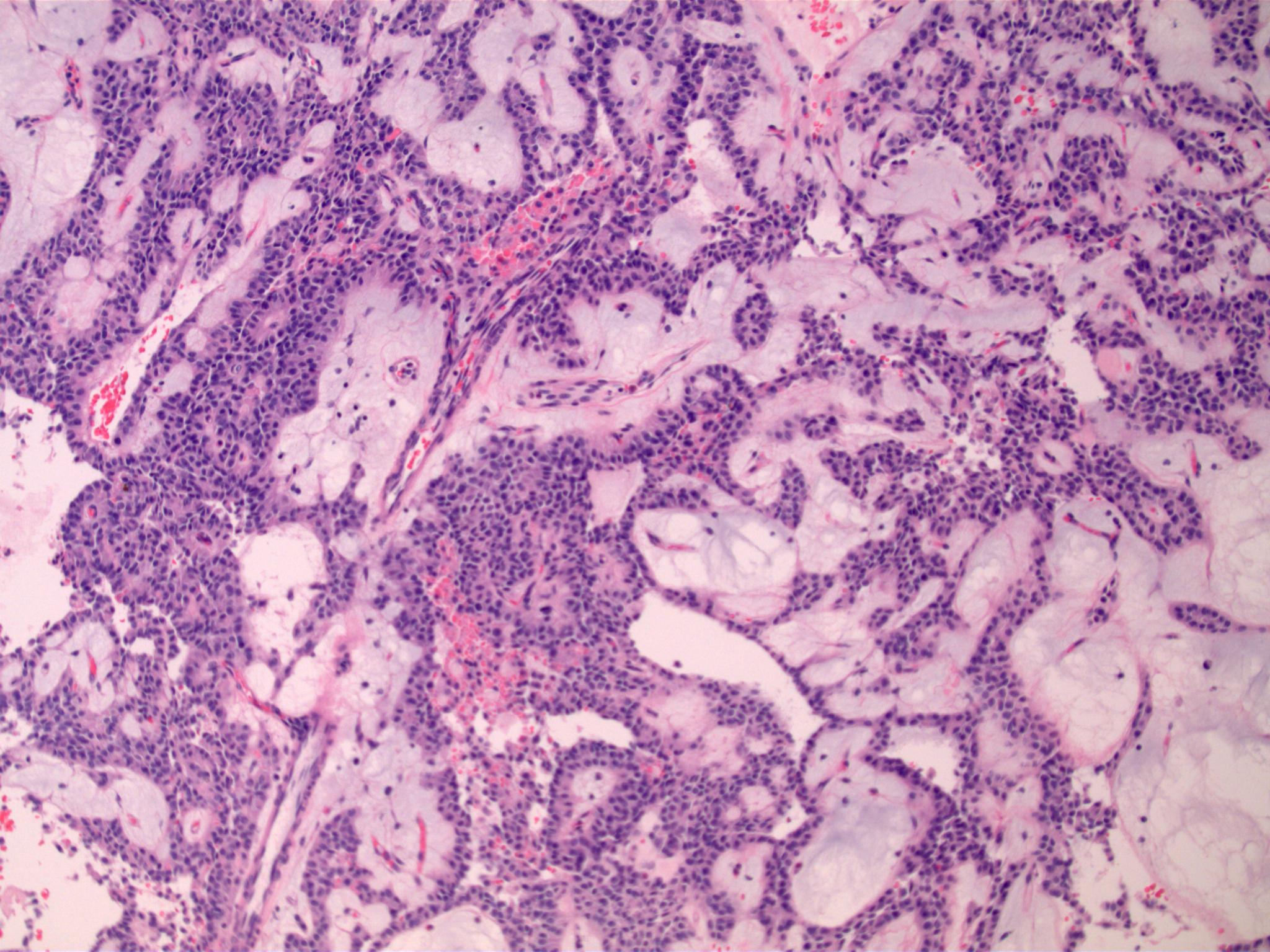
Figure: B) Beta-catenin positive staining of pancreatic mass aspirate
Disclosures:
Nikolay Lifshaz indicated no relevant financial relationships.
Shruti Verma indicated no relevant financial relationships.
Syed F. Jafri indicated no relevant financial relationships.
Nikolay Lifshaz, DO, Shruti Verma, MD, Syed F. Jafri, MD. P2287 - Solid Pseudopapillary Neoplasm of the Pancreas: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
