Monday Poster Session
Category: Biliary/Pancreas
P2283 - Isolated Pancreatic Metastasis of Renal Cell Carcinoma Without a Renal Primary
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Cathy Zheng, MD
University of Miami Miller School of Medicine
Miami, FL
Presenting Author(s)
Cathy Zheng, MD1, Sunil Amin, MD, MPH2, Marijo Bilusic, MD, PhD1, Oleksandr N. Kryvenko, MD2, Patricia D. Jones, MD, MSCR1
1University of Miami Miller School of Medicine, Miami, FL; 2University of Miami Health System, Miami, FL
Introduction: Pancreatic metastases account for 2-5% of pancreatic malignancies, with renal cell carcinoma (RCC) being a common source. While pancreatic metastases from RCC often present years after nephrectomy, isolated pancreatic RCC metastasis without a detectable renal primary is exceedingly rare. We present such a case.
Case Description/
Methods: A 70-year-old man with treated hepatitis C, well-compensated cirrhosis, and history of hepatocellular carcinoma (HCC) treated with stereotactic body radiation therapy (SBRT) had surveillance imaging, which incidentally revealed pancreatic cysts in the uncinate process and neck. Magnetic resonance cholangiopancreatography showed interval growth of the pancreatic head/neck lesion to 1.6 cm (from 0.7 cm eight months prior), with stable uncinate cyst. Endoscopic ultrasound (EUS) confirmed both cysts as intraductal papillary mucinous neoplasms. Unexpectedly, EUS identified a 1.8 x 1.7 cm lesion in the pancreatic body. Fine needle biopsy revealed clear cell renal cell carcinoma, positive for keratin 8/18, CA-IX, vimentin, and PAX8, and negative for keratin 7. Compared to the patient’s prior liver biopsy, which favored poorly differentiated HCC due to weakly positive Glypican 3, the pancreatic lesion was histologically distinct. Pancreas protocol CT localized the lesion to the superior border of the pancreas, abutting the main pancreatic duct. No renal masses were found aside from simple left renal cysts, and cyst biopsy was negative for malignancy. No other metastases were identified. The patient had no history of renal disease or malignancy-related symptoms. Distal pancreatectomy and splenectomy were considered but precluded by clinically significant portal hypertension. He was treated with SBRT (40 Gy/5 fractions) and opted for surveillance imaging every 3 months over adjuvant pembrolizumab.
Discussion: This case highlights a rare isolated pancreatic RCC metastasis without a known primary. Few such cases have been reported, with other sites including adrenal glands, bone, lung, muscle, and liver. Only one other case reports a solitary pancreatic metastasis. Although pancreatic involvement is uncommon (0.25-3% of metastatic RCC cases), metastatic RCC should be considered in the differential diagnosis of pancreatic lesions. This case also highlights the benefit of EUS. Distinguishing primary pancreatic cancer from metastasis can be challenging; tissue sampling with immunohistochemical studies is essential for accurate diagnosis and management.
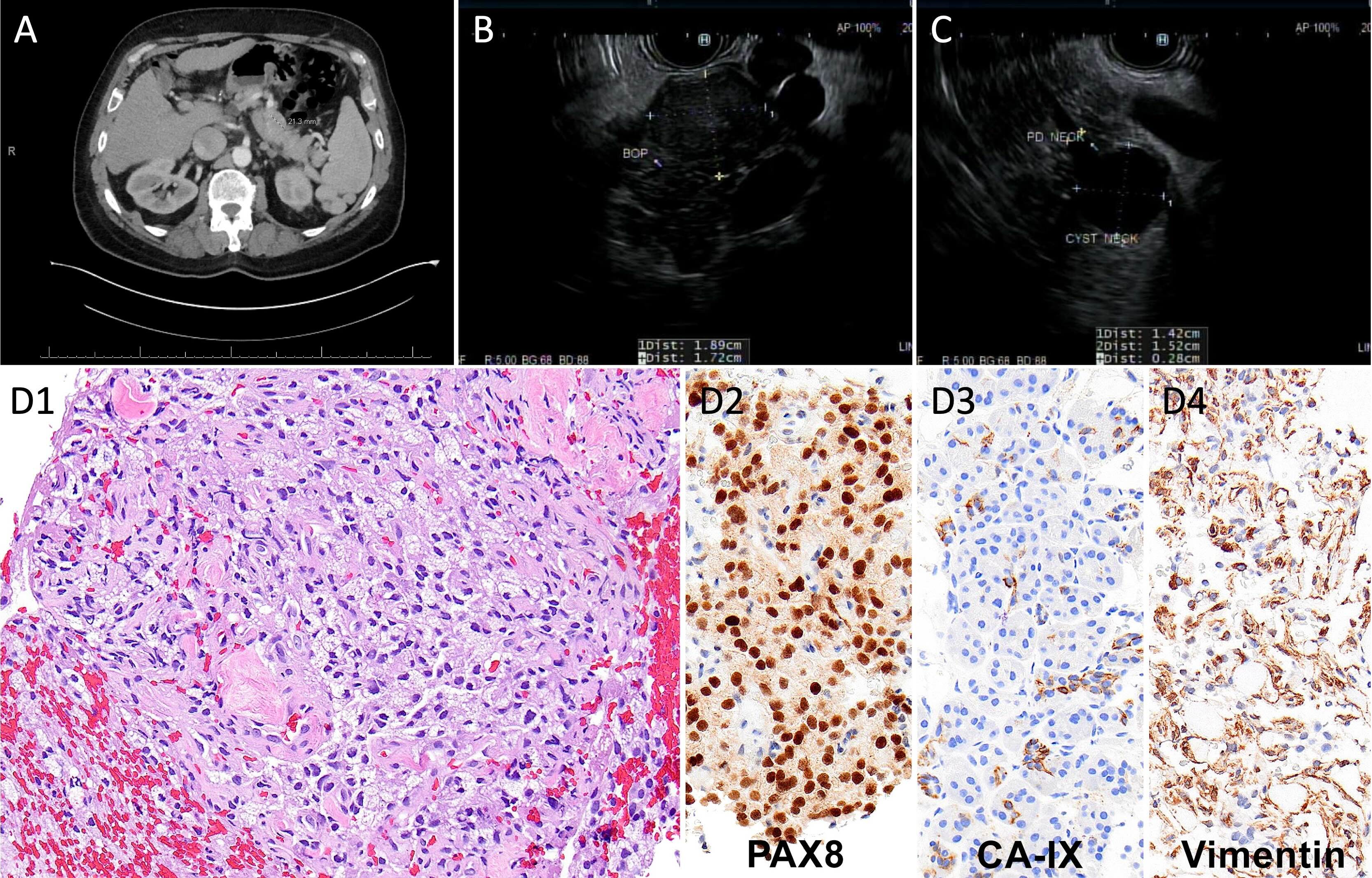
Figure: (A) CT abdomen and pelvis with contrast demonstrating an ill-defined, round soft tissue lesion measuring 21.3 mm located just above the distal body of the pancreas, representing pancreatic metastasis from renal cell carcinoma. (B) Endosonographic image of clear cell renal carcinoma presenting as a 19 mm x 17 mm hypoechoic mass in the body of pancreas. (C) Endosonographic image of a 14 mm x 15 mm cyst in the neck of the pancreas with clear communication with the pancreatic duct, consistent with branch-duct IPMN. (D) Histopathology of pancreatic clear cell renal cell carcinoma: hematoxylin and eosin stain (1), positive immunohistochemical staining for PAX-8 (2), CA-IX (3), and vimentin (4) at 20x magnification.
Disclosures:
Cathy Zheng indicated no relevant financial relationships.
Sunil Amin: 3D Matrix – Consultant. Boston Scientific – Consultant. Medtronic – Consultant.
Marijo Bilusic indicated no relevant financial relationships.
Oleksandr Kryvenko indicated no relevant financial relationships.
Patricia Jones indicated no relevant financial relationships.
Cathy Zheng, MD1, Sunil Amin, MD, MPH2, Marijo Bilusic, MD, PhD1, Oleksandr N. Kryvenko, MD2, Patricia D. Jones, MD, MSCR1. P2283 - Isolated Pancreatic Metastasis of Renal Cell Carcinoma Without a Renal Primary, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Miami Miller School of Medicine, Miami, FL; 2University of Miami Health System, Miami, FL
Introduction: Pancreatic metastases account for 2-5% of pancreatic malignancies, with renal cell carcinoma (RCC) being a common source. While pancreatic metastases from RCC often present years after nephrectomy, isolated pancreatic RCC metastasis without a detectable renal primary is exceedingly rare. We present such a case.
Case Description/
Methods: A 70-year-old man with treated hepatitis C, well-compensated cirrhosis, and history of hepatocellular carcinoma (HCC) treated with stereotactic body radiation therapy (SBRT) had surveillance imaging, which incidentally revealed pancreatic cysts in the uncinate process and neck. Magnetic resonance cholangiopancreatography showed interval growth of the pancreatic head/neck lesion to 1.6 cm (from 0.7 cm eight months prior), with stable uncinate cyst. Endoscopic ultrasound (EUS) confirmed both cysts as intraductal papillary mucinous neoplasms. Unexpectedly, EUS identified a 1.8 x 1.7 cm lesion in the pancreatic body. Fine needle biopsy revealed clear cell renal cell carcinoma, positive for keratin 8/18, CA-IX, vimentin, and PAX8, and negative for keratin 7. Compared to the patient’s prior liver biopsy, which favored poorly differentiated HCC due to weakly positive Glypican 3, the pancreatic lesion was histologically distinct. Pancreas protocol CT localized the lesion to the superior border of the pancreas, abutting the main pancreatic duct. No renal masses were found aside from simple left renal cysts, and cyst biopsy was negative for malignancy. No other metastases were identified. The patient had no history of renal disease or malignancy-related symptoms. Distal pancreatectomy and splenectomy were considered but precluded by clinically significant portal hypertension. He was treated with SBRT (40 Gy/5 fractions) and opted for surveillance imaging every 3 months over adjuvant pembrolizumab.
Discussion: This case highlights a rare isolated pancreatic RCC metastasis without a known primary. Few such cases have been reported, with other sites including adrenal glands, bone, lung, muscle, and liver. Only one other case reports a solitary pancreatic metastasis. Although pancreatic involvement is uncommon (0.25-3% of metastatic RCC cases), metastatic RCC should be considered in the differential diagnosis of pancreatic lesions. This case also highlights the benefit of EUS. Distinguishing primary pancreatic cancer from metastasis can be challenging; tissue sampling with immunohistochemical studies is essential for accurate diagnosis and management.
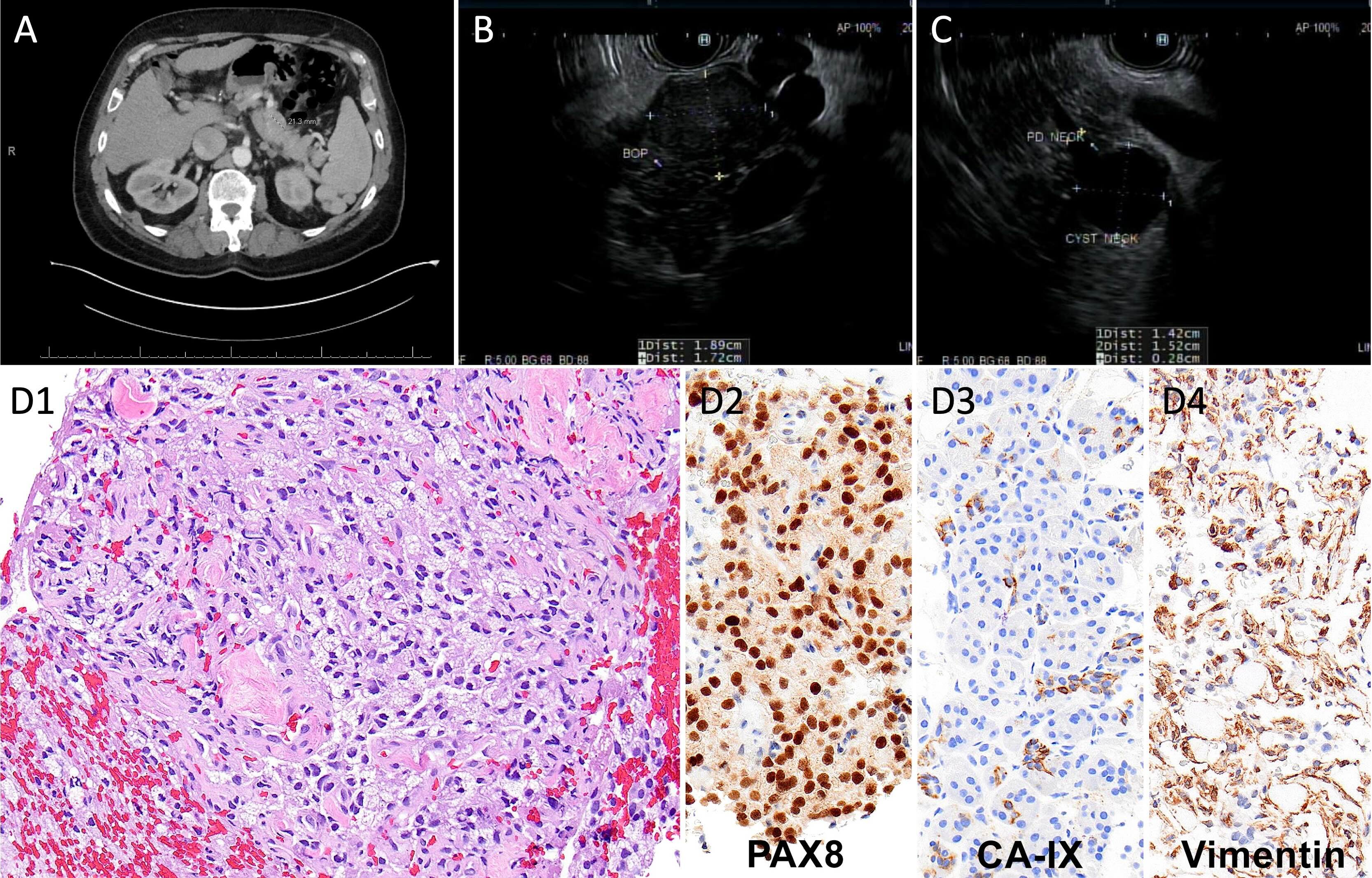
Figure: (A) CT abdomen and pelvis with contrast demonstrating an ill-defined, round soft tissue lesion measuring 21.3 mm located just above the distal body of the pancreas, representing pancreatic metastasis from renal cell carcinoma. (B) Endosonographic image of clear cell renal carcinoma presenting as a 19 mm x 17 mm hypoechoic mass in the body of pancreas. (C) Endosonographic image of a 14 mm x 15 mm cyst in the neck of the pancreas with clear communication with the pancreatic duct, consistent with branch-duct IPMN. (D) Histopathology of pancreatic clear cell renal cell carcinoma: hematoxylin and eosin stain (1), positive immunohistochemical staining for PAX-8 (2), CA-IX (3), and vimentin (4) at 20x magnification.
Disclosures:
Cathy Zheng indicated no relevant financial relationships.
Sunil Amin: 3D Matrix – Consultant. Boston Scientific – Consultant. Medtronic – Consultant.
Marijo Bilusic indicated no relevant financial relationships.
Oleksandr Kryvenko indicated no relevant financial relationships.
Patricia Jones indicated no relevant financial relationships.
Cathy Zheng, MD1, Sunil Amin, MD, MPH2, Marijo Bilusic, MD, PhD1, Oleksandr N. Kryvenko, MD2, Patricia D. Jones, MD, MSCR1. P2283 - Isolated Pancreatic Metastasis of Renal Cell Carcinoma Without a Renal Primary, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

