Monday Poster Session
Category: Colon
P2483 - Lymphocytic Colitis Evolving Into Collagenous Colitis: A Case Series

Yasaman Salahmand, MPH, BS
David Geffen School of Medicine at UCLA
Los Angeles, CA
Presenting Author(s)
1David Geffen School of Medicine at UCLA, Los Angeles, CA; 2University of California Los Angeles Medical Center, Los Angeles, CA
Introduction:
Microscopic colitis (MC), a recognized cause of chronic diarrhea, comprises two histologic subtypes: lymphocytic colitis (LC) and collagenous colitis (CC). While both share clinical features and response to budesonide, it remains unclear whether LC and CC represent distinct conditions or stages on a disease continuum. Clarifying this relationship may guide earlier intervention and disease monitoring. This case series describes three patients initially diagnosed with LC who later developed histologic features consistent with CC, suggesting progression across the MC spectrum.
Case Description/
Methods:
We retrospectively reviewed clinical and histopathologic data from three adult patients diagnosed with LC and CC at some point in time during their medical history, and who slod underwent serial colonoscopies with biopsies. We assessed clinical presentation, histologic features, treatment response, and evolution of LC to CC over time.
All three patients were initially diagnosed with LC based on elevated intraepithelial lymphocytes. Over time, repeat biopsies demonstrated thickened subepithelial collagen bands consistent with CC, indicating histologic progression. Case 1, a 77-year-old with celiac disease, initially showed LC transitioning to early CC. Despite clinical remission, repeat biopsies later confirmed CC. Case 2, a 21-year-old with common variable immunodeficiency, progressed from LC to CC within seven months. Case 3, an 84-year-old with longstanding reflux symptoms and diarrhea, declined pharmacologic therapy; repeat biopsies also confirmed progression to CC. Two patients responded to budesonide, while one opted for symptomatic management.
Discussion:
This case series supports the hypothesis that LC may evolve into CC, suggesting these entities exist along a dynamic disease spectrum rather than as isolated conditions. Potential mechanisms include immune dysregulation, epithelial barrier dysfunction, collagen deposition due to chronic inflammation, medication side effects, or genetic predispositions. Given CC has worse symptoms and outcomes, recognizing LC as a potential precursor to CC has clinical implications, including closer surveillance and early treatment escalation. Further prospective studies are needed to confirm progression rates and identify risk factors for histologic transition.
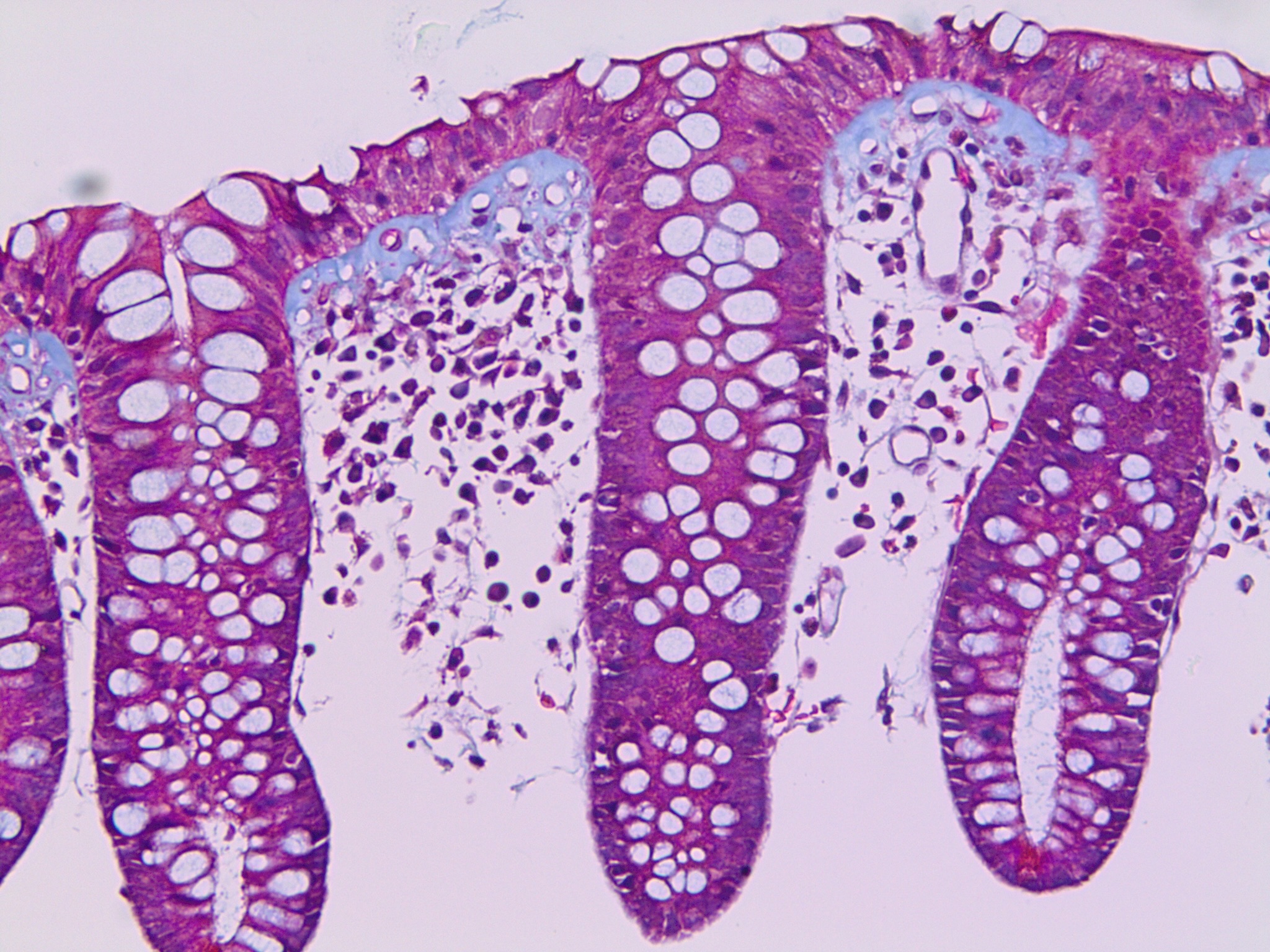
Figure: Case 1, Rectum, Trichrome Stain, 200X. Follow-up biopsy showing established collagenous colitis with a subepithelial collagen band measuring up to 20 microns.
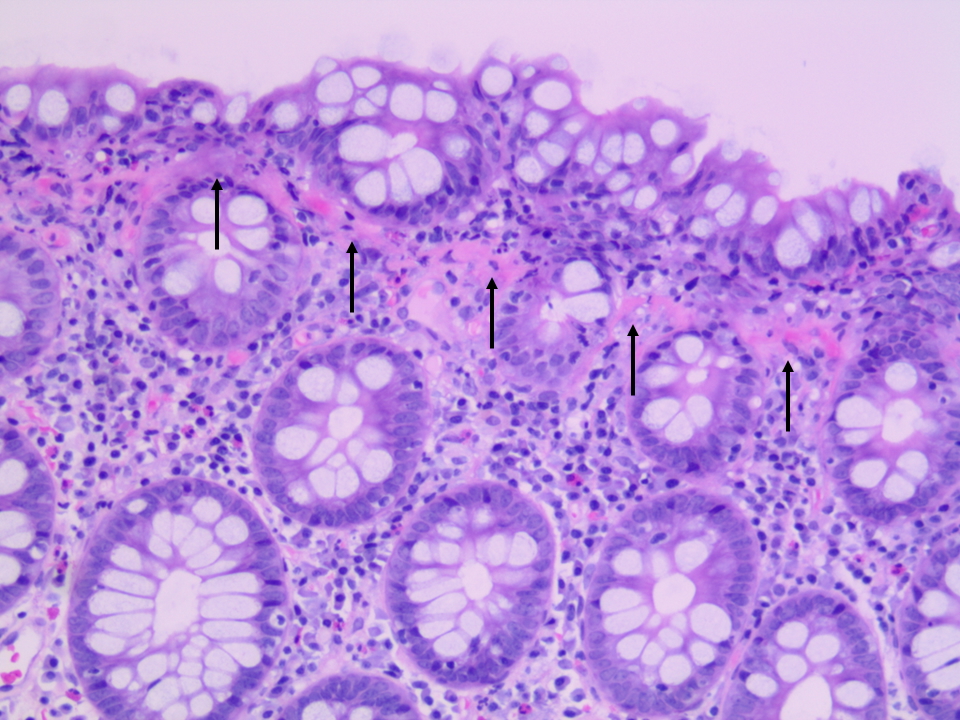
Figure: Case 3, Random Colon, H&E Stain, 200X. Lymphocytic colitis with a focal discrete subepithelial collagen band measuring approximately 7 microns, suggestive of evolution toward collagenous colitis.
Disclosures:
Yasaman Salahmand indicated no relevant financial relationships.
Guy Weiss: Guidepoint – Consultant. Regeneron – Consultant.
Jeffrey Goldstein: Amgen – Stock-publicly held company(excluding mutual/index funds). Bausch & Lomb – Stock-publicly held company(excluding mutual/index funds). Baxter – Stock-publicly held company(excluding mutual/index funds). Bristol Myers Squibb – Stock-publicly held company(excluding mutual/index funds). CVS – Stock-publicly held company(excluding mutual/index funds). Pfizer – Stock-publicly held company(excluding mutual/index funds). Target – Stock-publicly held company(excluding mutual/index funds). Wal Mart – Stock-publicly held company(excluding mutual/index funds).
Yasaman Salahmand, MPH, BS1, Guy A. Weiss, MD2, Jeffrey D. Goldstein, MD1. P2483 - Lymphocytic Colitis Evolving Into Collagenous Colitis: A Case Series, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
