Monday Poster Session
Category: Colon
P2572 - Unusual Presentation of Cocaine-Induced Hematochezia from a Distal Rectal Vessel
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sebastian Hermida Velasquez, DO
Palmetto General Hospital
Miami, FL
Presenting Author(s)
Sebastian Hermida Velasquez, DO1, Salaah Siddiqui, DO2, Sanskriti Sharma, MD3, Adam Koller, DO2, Natalia Martin, DO4, Karthik Mohan, DO3
1Palmetto General Hospital, Hialeah, FL; 2Larkin Community Hospital, Miami, FL; 3Larkin Community Hospital, Hialeah, FL; 4Larkin Community Hospital, South Miami, FL
Introduction: Cocaine use is a well-documented risk factor for upper GI bleeding and ischemic colitis, but its association with isolated rectal vessel hemorrhage remains rare in occurrence. In clinical practice, one often encounters cocaine-related complications, yet lower GI bleeding from rectal source is exceptionally uncommon. Our patient’s presentation highlights how cocaine's vasoconstrictive effects may manifest unpredictably, challenging conventional diagnostic pathways. This atypical presentation serves as a reminder to reconsider the classic cocaine ischemic effect that is usually limited to watershed areas of the colon. This case emphasizes that even well-perfused rectal mucosa may be vulnerable to cocaine’s vasoactive properties.
Case Description/
Methods: This is a 47-year-old male with past medical history of substance abuse disorder and no prior episodes of melena, hematochezia or other any other GI symptoms. The patient was admitted due sudden onset hematochezia followed by a near-syncopal event. Upon admission, the patient experienced rapid hemoglobin decline (11 to 7.0 g/dL within hours). CT angiography of the abdomen and pelvis revealed active extravasation of contrast into the rectum, compatible with an acute GI bleed. The patient ultimately underwent colonoscopy where a large bleeding vessel was located 3 cm from the anal verge, subsequently treated with epinephrine injection and hemoclip placement. Throughout the course of his hospitalization, hemoglobin levels continued to decline post-procedure (7.8 to 7.0 g/dL) before stabilizing after additional blood transfusions. This delayed hemoglobin stabilization hinted at the possible cocaine prolonged vasoactive effects, warranting extended observation even after apparent hemostasis.
Discussion: This case challenges the usual textbook presentation of cocaine-related GI injury. Here we can see how distal rectal vessels can rupture under the vasoconstrictive effects of cocaine. From a practical standpoint, endoscopic hemostasis remains a viable intervention for many patients, though one should anticipate the possibility of delayed hemoglobin stabilization; this could be in part from recurrent vasospasm or platelet dysfunction. GI bleeding events such as this one, should remind clinicians to keep a high index of suspicion for substance use in patients presenting with unexplained GI bleeding. We advocate for routine toxicology screening in similar cases, as early identification may guide both endoscopic and pharmacological intervention strategies.
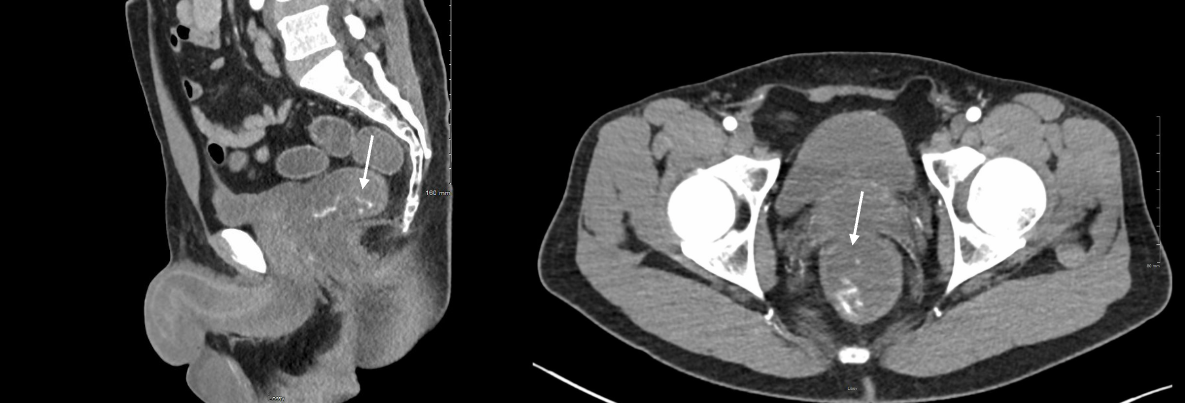
Figure: Axial and Sagittal CT Angiography Images Revealing Active Extravasation (Arrow) into the Rectum, Localizing the Source of Hematochezia.
Disclosures:
Sebastian Hermida Velasquez indicated no relevant financial relationships.
Salaah Siddiqui indicated no relevant financial relationships.
Sanskriti Sharma indicated no relevant financial relationships.
Adam Koller indicated no relevant financial relationships.
Natalia Martin indicated no relevant financial relationships.
Karthik Mohan indicated no relevant financial relationships.
Sebastian Hermida Velasquez, DO1, Salaah Siddiqui, DO2, Sanskriti Sharma, MD3, Adam Koller, DO2, Natalia Martin, DO4, Karthik Mohan, DO3. P2572 - Unusual Presentation of Cocaine-Induced Hematochezia from a Distal Rectal Vessel, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Palmetto General Hospital, Hialeah, FL; 2Larkin Community Hospital, Miami, FL; 3Larkin Community Hospital, Hialeah, FL; 4Larkin Community Hospital, South Miami, FL
Introduction: Cocaine use is a well-documented risk factor for upper GI bleeding and ischemic colitis, but its association with isolated rectal vessel hemorrhage remains rare in occurrence. In clinical practice, one often encounters cocaine-related complications, yet lower GI bleeding from rectal source is exceptionally uncommon. Our patient’s presentation highlights how cocaine's vasoconstrictive effects may manifest unpredictably, challenging conventional diagnostic pathways. This atypical presentation serves as a reminder to reconsider the classic cocaine ischemic effect that is usually limited to watershed areas of the colon. This case emphasizes that even well-perfused rectal mucosa may be vulnerable to cocaine’s vasoactive properties.
Case Description/
Methods: This is a 47-year-old male with past medical history of substance abuse disorder and no prior episodes of melena, hematochezia or other any other GI symptoms. The patient was admitted due sudden onset hematochezia followed by a near-syncopal event. Upon admission, the patient experienced rapid hemoglobin decline (11 to 7.0 g/dL within hours). CT angiography of the abdomen and pelvis revealed active extravasation of contrast into the rectum, compatible with an acute GI bleed. The patient ultimately underwent colonoscopy where a large bleeding vessel was located 3 cm from the anal verge, subsequently treated with epinephrine injection and hemoclip placement. Throughout the course of his hospitalization, hemoglobin levels continued to decline post-procedure (7.8 to 7.0 g/dL) before stabilizing after additional blood transfusions. This delayed hemoglobin stabilization hinted at the possible cocaine prolonged vasoactive effects, warranting extended observation even after apparent hemostasis.
Discussion: This case challenges the usual textbook presentation of cocaine-related GI injury. Here we can see how distal rectal vessels can rupture under the vasoconstrictive effects of cocaine. From a practical standpoint, endoscopic hemostasis remains a viable intervention for many patients, though one should anticipate the possibility of delayed hemoglobin stabilization; this could be in part from recurrent vasospasm or platelet dysfunction. GI bleeding events such as this one, should remind clinicians to keep a high index of suspicion for substance use in patients presenting with unexplained GI bleeding. We advocate for routine toxicology screening in similar cases, as early identification may guide both endoscopic and pharmacological intervention strategies.
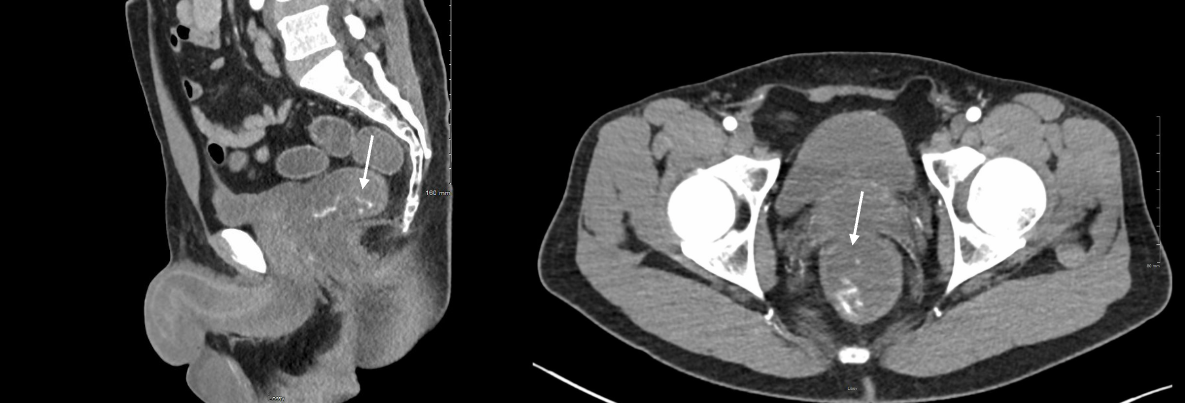
Figure: Axial and Sagittal CT Angiography Images Revealing Active Extravasation (Arrow) into the Rectum, Localizing the Source of Hematochezia.
Disclosures:
Sebastian Hermida Velasquez indicated no relevant financial relationships.
Salaah Siddiqui indicated no relevant financial relationships.
Sanskriti Sharma indicated no relevant financial relationships.
Adam Koller indicated no relevant financial relationships.
Natalia Martin indicated no relevant financial relationships.
Karthik Mohan indicated no relevant financial relationships.
Sebastian Hermida Velasquez, DO1, Salaah Siddiqui, DO2, Sanskriti Sharma, MD3, Adam Koller, DO2, Natalia Martin, DO4, Karthik Mohan, DO3. P2572 - Unusual Presentation of Cocaine-Induced Hematochezia from a Distal Rectal Vessel, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
