Monday Poster Session
Category: Colon
P2568 - Primary Colonic MALT Lymphoma
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rutvi Katariya, MD (she/her/hers)
Atrium Health Carolinas Medical Center
Charlotte, NC
Presenting Author(s)
Rutvi Katariya, MD, Jonathan Dvorak, MD, Paris Charilaou, MD
Atrium Health Carolinas Medical Center, Charlotte, NC
Introduction: Mucosal-associated lymph tissue (MALT) lymphoma, also known as extranodal marginal zone lymphoma (EMZL), is a rare type of B-cell non-Hodgkin lymphoma often found in the stomach. Colonic EMZL is very rare and only documented in case reports. Its pathogenesis remains unclear, although chronic antigenic stimulation, inflammatory bowel disease, and immune dysregulation are potential contributing factors. We present a case of isolated colonic EMZL.
Case Description/
Methods: A 48-year-old female with hypothyroidism presented for screening colonoscopy. She lost 15 lbs over 9 months while on semaglutide and reported nightly hot flashes with diaphoresis, which she attributed to menopause. Colonoscopy found five sub-centimeter sessile polyps in the cecum, transverse, and descending colon. Pathology revealed B-cell lymphoma (BCL) consistent with EMZL without diffuse large BCL (DLBCL) transformation. Upper endoscopy showed no pathologic evidence of H. Pylori infection. Primary colonic EMZL was diagnosed when workup revealed no extracolonic involvement on PET/CT and no bone marrow involvement. Oncologic evaluation deemed it to be a slow-growing, incurable, but treatable lymphoma. Given her staging, observation was favored over single-agent non-curative rituximab. She has had a normal one-year surveillance colonoscopy.
Discussion: Primary colonic EMZLs are extremely rare with presentations varying from asymptomatic to GI bleeding, ileocecal intussusception, and intestinal obstruction. The etiology of colonic EMZL is unclear. H. pylori has been linked to lymphomagenesis in gastric MALT lymphoma due to persistent inflammation, and its eradication can lead to lymphoma regression in a majority of early-stage cases. Other infectious agents include Chlamydia psittaci, Achromobacter xylosoxidans, and Hepatitis C in various different organs. A subset may also demonstrate BIRC3/MALT1 fusion and IGH/IGK gene rearrangements. Our patient had neither H. pylori nor genetic alterations.
There are no standardized treatment regimens. Endoscopic resection or systemic chemotherapy can be considered based on disease burden, systemic involvement, and DLBCL transformation. In a single case series, 80% of patients had no clinically evident disease after observation or radiation/chemotherapy. This case reminds endoscopists that not all mucosal polyps are adenomas or serrated lesions, and that MALT can exist exclusively in the colon even in the absence of H. pylori infection.
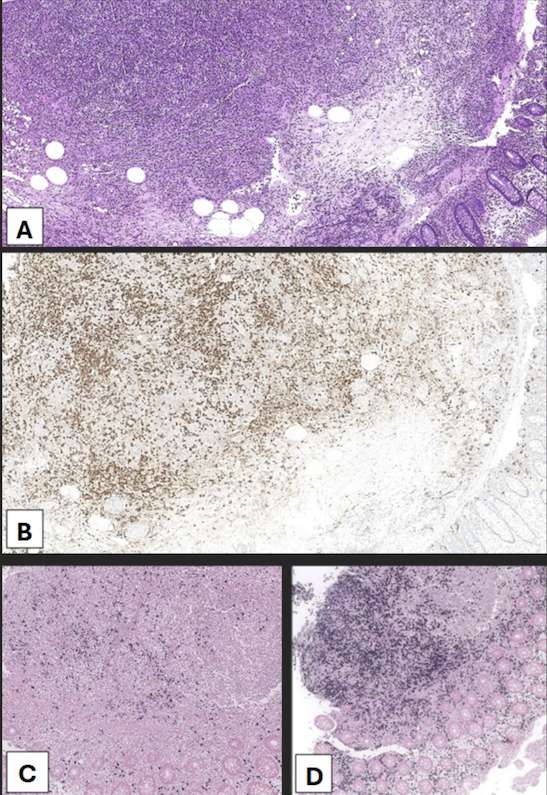
Figure: Figure 1. (A) A polypoid lesion with regular round pits uniformly distributed. (B) A polypoid lesion with asteroid/stellate pit pattern. (C) (D, with narrow-band imaging) Showing the same polypoid lesion with more irregularly shaped tubular pit pattern, with areas of absent pits and central foci of mucosal erosion.
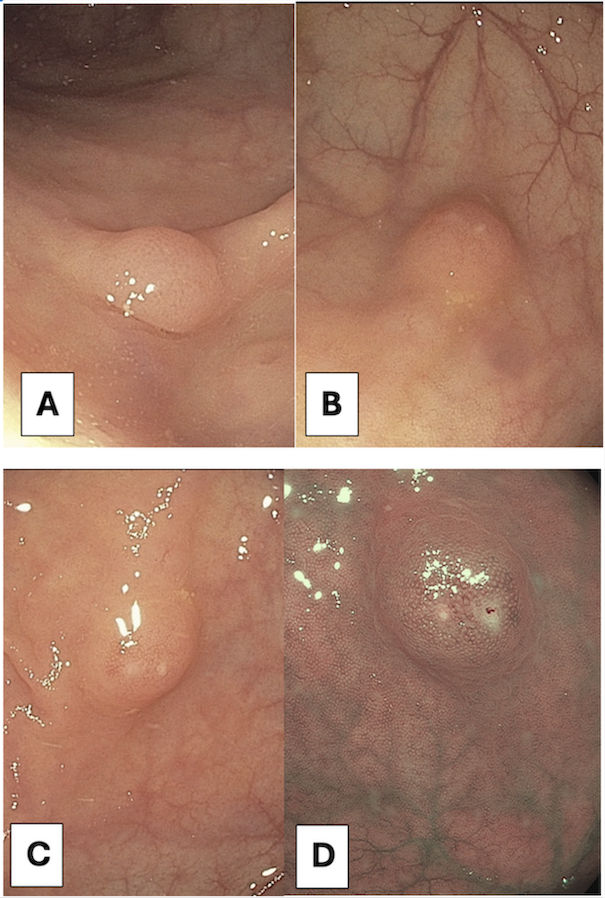
Figure: Figure 2. Pathology slides for primary colonic EMZL. (A) H&E stain to differentiate structures, for which key histologic features include lymphoepithelial lesions, centrocyte-like cells, and plasmacytic differentiation. (B) CD20 staining, indicating the presence of specific B-cell populations. (C) Kappa light chain and (D) Lambda light chains with varying distributions, supporting the diagnosis of MALT lymphoma rather than lymphoproliferative disorders.
Disclosures:
Rutvi Katariya indicated no relevant financial relationships.
Jonathan Dvorak indicated no relevant financial relationships.
Paris Charilaou: Abbvie Inc. – Advisory Committee/Board Member. Prometheus Biosciences – Consultant.
Rutvi Katariya, MD, Jonathan Dvorak, MD, Paris Charilaou, MD. P2568 - Primary Colonic MALT Lymphoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Atrium Health Carolinas Medical Center, Charlotte, NC
Introduction: Mucosal-associated lymph tissue (MALT) lymphoma, also known as extranodal marginal zone lymphoma (EMZL), is a rare type of B-cell non-Hodgkin lymphoma often found in the stomach. Colonic EMZL is very rare and only documented in case reports. Its pathogenesis remains unclear, although chronic antigenic stimulation, inflammatory bowel disease, and immune dysregulation are potential contributing factors. We present a case of isolated colonic EMZL.
Case Description/
Methods: A 48-year-old female with hypothyroidism presented for screening colonoscopy. She lost 15 lbs over 9 months while on semaglutide and reported nightly hot flashes with diaphoresis, which she attributed to menopause. Colonoscopy found five sub-centimeter sessile polyps in the cecum, transverse, and descending colon. Pathology revealed B-cell lymphoma (BCL) consistent with EMZL without diffuse large BCL (DLBCL) transformation. Upper endoscopy showed no pathologic evidence of H. Pylori infection. Primary colonic EMZL was diagnosed when workup revealed no extracolonic involvement on PET/CT and no bone marrow involvement. Oncologic evaluation deemed it to be a slow-growing, incurable, but treatable lymphoma. Given her staging, observation was favored over single-agent non-curative rituximab. She has had a normal one-year surveillance colonoscopy.
Discussion: Primary colonic EMZLs are extremely rare with presentations varying from asymptomatic to GI bleeding, ileocecal intussusception, and intestinal obstruction. The etiology of colonic EMZL is unclear. H. pylori has been linked to lymphomagenesis in gastric MALT lymphoma due to persistent inflammation, and its eradication can lead to lymphoma regression in a majority of early-stage cases. Other infectious agents include Chlamydia psittaci, Achromobacter xylosoxidans, and Hepatitis C in various different organs. A subset may also demonstrate BIRC3/MALT1 fusion and IGH/IGK gene rearrangements. Our patient had neither H. pylori nor genetic alterations.
There are no standardized treatment regimens. Endoscopic resection or systemic chemotherapy can be considered based on disease burden, systemic involvement, and DLBCL transformation. In a single case series, 80% of patients had no clinically evident disease after observation or radiation/chemotherapy. This case reminds endoscopists that not all mucosal polyps are adenomas or serrated lesions, and that MALT can exist exclusively in the colon even in the absence of H. pylori infection.
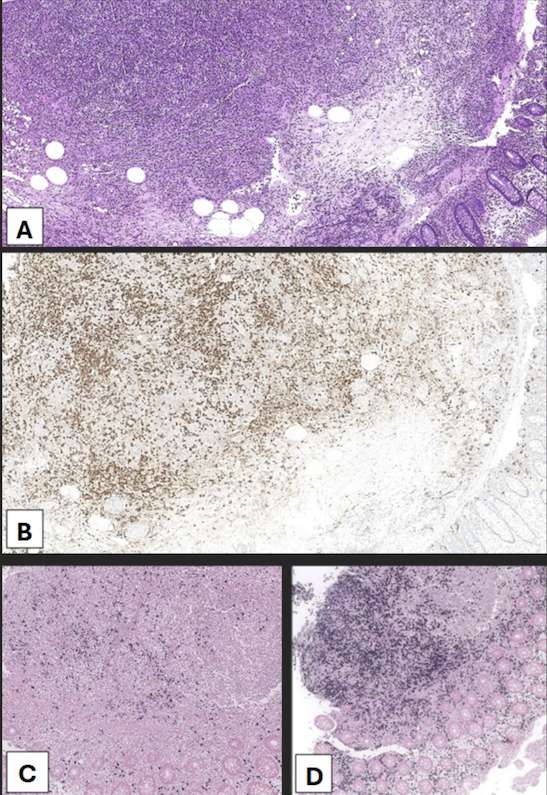
Figure: Figure 1. (A) A polypoid lesion with regular round pits uniformly distributed. (B) A polypoid lesion with asteroid/stellate pit pattern. (C) (D, with narrow-band imaging) Showing the same polypoid lesion with more irregularly shaped tubular pit pattern, with areas of absent pits and central foci of mucosal erosion.
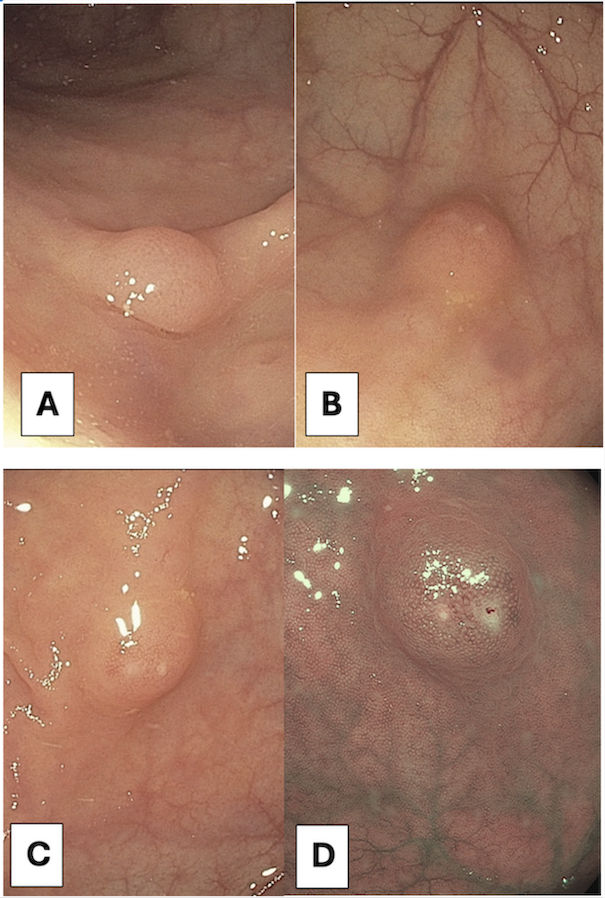
Figure: Figure 2. Pathology slides for primary colonic EMZL. (A) H&E stain to differentiate structures, for which key histologic features include lymphoepithelial lesions, centrocyte-like cells, and plasmacytic differentiation. (B) CD20 staining, indicating the presence of specific B-cell populations. (C) Kappa light chain and (D) Lambda light chains with varying distributions, supporting the diagnosis of MALT lymphoma rather than lymphoproliferative disorders.
Disclosures:
Rutvi Katariya indicated no relevant financial relationships.
Jonathan Dvorak indicated no relevant financial relationships.
Paris Charilaou: Abbvie Inc. – Advisory Committee/Board Member. Prometheus Biosciences – Consultant.
Rutvi Katariya, MD, Jonathan Dvorak, MD, Paris Charilaou, MD. P2568 - Primary Colonic MALT Lymphoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
