Monday Poster Session
Category: Colon
P2564 - Atypical Presentation of IgA Vasculitis (Henoch-Schönlein Purpura) With Severe Colonic Ischemia and Perforation
- ME
Mishal Ejaz, MBBS
MedStar Georgetown University Hospital
Baltimore, MD
Presenting Author(s)
1MedStar Georgetown University Hospital, Baltimore, MD; 2MedStar Health, Baltimore, MD
Introduction:
Immunoglobulin A vasculitis (IgAV), formerly Henoch-Schönlein Purpura, is a rare small-vessel vasculitis characterized by IgA deposition. It typically presents with palpable purpura, arthralgia, and abdominal pain. The incidence in adults ranges from 0.1 to 0.8 per 100,000. GI involvement is variable and may affect any part of the tract. While some cases present with mild abdominal discomfort or elevated transaminases, others may develop life-threatening complications such as bowel ischemia, perforation, or peritonitis.
Case Description/
Methods:
A 43-year-old male with a history of IgAV diagnosed 13 years prior presented with bilateral lower extremity rash, arthralgia, and edema following a recent upper respiratory tract infection. On admission, he was tachycardic (HR 116) and hypertensive (BP 137/105). A palpable purpuric rash and painful small joint arthralgias were noted. He was diagnosed with recurrent IgAV with inflammatory arthritis and started on a steroid taper. On hospital day 2, he developed new-onset clear watery stools. CT abdomen showed colonic distention (cecum up to 10 cm) without mural thickening or signs of vasculitis. The next day, he developed sudden severe abdominal pain, diaphoresis, and peritoneal signs. Abdominal X-ray revealed distended bowel loops; chest X-ray showed free air under the diaphragm, indicating bowel perforation. Emergent surgery was performed. Exploratory laparotomy revealed bowel perforation, necessitating hemicolectomy with bowel left in discontinuity. He returned for re-exploration, washout, and end ileostomy. Skin biopsies confirmed leukocytoclastic vasculitis consistent with IgAV. Colectomy specimen pathology revealed widespread colonic and ileal inflammation, serositis, and vascular thrombi—findings compatible with IgAV-related bowel injury.
Discussion:
This case illustrates a rare, severe GI complication of recurrent adult IgAV. Though uncommon, adult-onset IgAV can progress rapidly from mild GI symptoms to life-threatening bowel ischemia and perforation. Diagnosis relies on clinical, imaging, and histologic data. While GI mortality in IgAV is low (0.7%-1%), complications such as mesenteric infarction and bowel perforation necessitate prompt recognition. Frequently reported symptoms are abdominal pain (79%), bleeding (38%), and nausea/vomiting (16%) in GI vasculitis. While corticosteroids are effective in many, surgical intervention may be required. Early multidisciplinary care is crucial in managing severe presentations.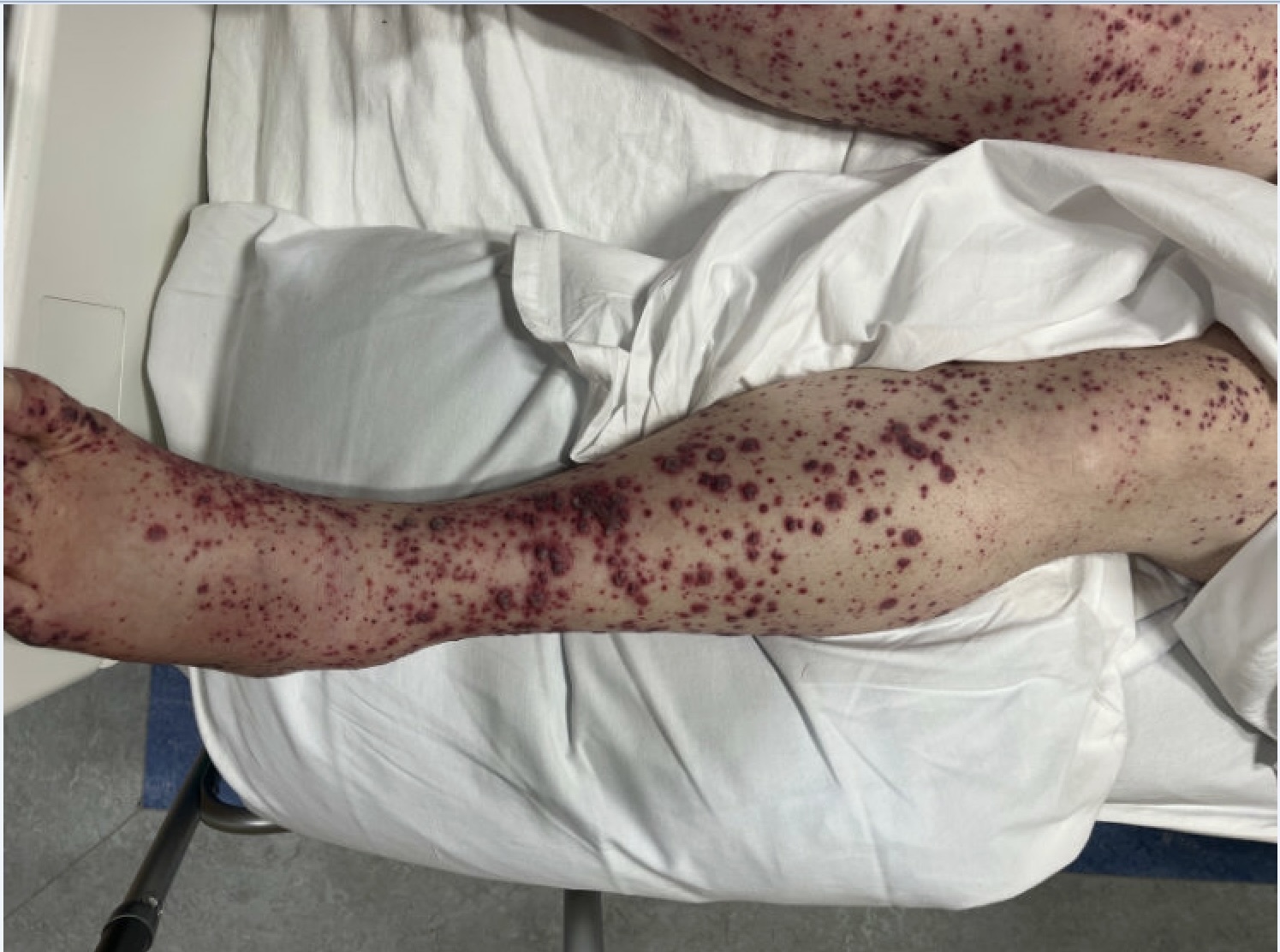
Figure: Palpable purpura on lower extremity
Disclosures:
Mishal Ejaz indicated no relevant financial relationships.
Brian R. Dyson indicated no relevant financial relationships.
Mishal Ejaz, MBBS1, Brian R. Dyson, DO2. P2564 - Atypical Presentation of IgA Vasculitis (Henoch-Schönlein Purpura) With Severe Colonic Ischemia and Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
