Monday Poster Session
Category: Colorectal Cancer Prevention
P2656 - Use of Stool-Based Tests Is Associated With Increased Uptake of the 2021 USPSTF Colorectal Cancer Screening Guidelines
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sarah Householder, MD (she/her/hers)
Yale New Haven Hospital
New Haven, CT
Presenting Author(s)
Sarah Householder, MD1, Andrew Loza, MD, PhD2, Jason Dominitz, MD, MHS3, Louise Davies, MD, MS4, Amy Justice, MD, PhD2, Christopher Rentsch, PhD2
1Yale New Haven Hospital, New Haven, CT; 2Yale University School of Medicine, New Haven, CT; 3University of Washington School of Medicine and VA Puget Sound Health Care System, Seattle, WA; 4Dartmouth Hitchcock Medical Center, White River Junction, VT
Introduction: In response to rising rates of colorectal cancer (CRC) in individuals younger than 50, the United States Preventative Services Task Force lowered the recommended screening initiation age for adults with average CRC risk from 50 to 45 years of age in 2021. This change is anticipated to prevent 1 death per 1000 persons screened, however, uptake of this practice is uncertain. Additionally, there is rising patient preference for non-endoscopic based methods particularly for newly eligible 50-52 year-old adults, but it is unknown whether modality of screening affects uptake in the 45-year-old cohort. Here we examine uptake of the new CRC screening in 45-year-olds within the Department of Veteran Affairs (VA) and associations with stool-based versus endoscopic-based modalities.
Methods: The Veterans Aging Cohort Study-National represents all individuals who have accessed VA care since 2000. All care delivered within the VA system is stored in a central repository called the Corporate Data Warehouse.
The study included all individuals who turned 45 years of age on or after May 21, 2021 and met criteria for average risk of CRC. Analyses focused on individuals engaged in clinical care, defined as having a visit within the two years prior to becoming eligible for screening. The cohort was stratified by the year after May 21, 2021 in which individuals turned 45. Cumulative incidence for screening completion and screening completion by stool-based and endoscopic-based modalities were calculated using the cmprsk package in R.
Results: 182,616 patients met study inclusion criteria. Cumulative incidence of completed screening showed year-on-year increases (Figure 1). This increase was predominantly due to a change in cumulative incidence of screening completion through stool-based testing (p< 0.001), with cumulative incidence of screening completion by endoscopic methods remaining similar across groups (p=0.53).
Discussion: Adherence to guidelines in screening of newly eligible 45-year-olds has increased since the recommendation change in 2021. Year-on-year improvements are associated with increased use of stool-based testing. These findings are likely multifactorial and may be driven by changes in patient and provider awareness, screening programs, and changes in access to preferred screening methods. Future work should investigate whether this uptake is uniform across subpopulations and extends beyond first time screening to re-screening.
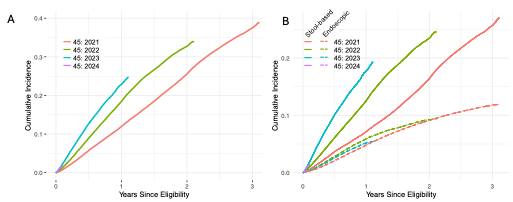
Figure: Cumulative incidence of screening across age cohorts. A. Cumulative incidence of screening completion across all modalities. B. Modality-specific cumulative incidence for stool-based (solid) and endoscopic (dashed) methods.
Disclosures:
Sarah Householder indicated no relevant financial relationships.
Andrew Loza indicated no relevant financial relationships.
Jason Dominitz indicated no relevant financial relationships.
Louise Davies indicated no relevant financial relationships.
Amy Justice indicated no relevant financial relationships.
Christopher Rentsch indicated no relevant financial relationships.
Sarah Householder, MD1, Andrew Loza, MD, PhD2, Jason Dominitz, MD, MHS3, Louise Davies, MD, MS4, Amy Justice, MD, PhD2, Christopher Rentsch, PhD2. P2656 - Use of Stool-Based Tests Is Associated With Increased Uptake of the 2021 USPSTF Colorectal Cancer Screening Guidelines, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Yale New Haven Hospital, New Haven, CT; 2Yale University School of Medicine, New Haven, CT; 3University of Washington School of Medicine and VA Puget Sound Health Care System, Seattle, WA; 4Dartmouth Hitchcock Medical Center, White River Junction, VT
Introduction: In response to rising rates of colorectal cancer (CRC) in individuals younger than 50, the United States Preventative Services Task Force lowered the recommended screening initiation age for adults with average CRC risk from 50 to 45 years of age in 2021. This change is anticipated to prevent 1 death per 1000 persons screened, however, uptake of this practice is uncertain. Additionally, there is rising patient preference for non-endoscopic based methods particularly for newly eligible 50-52 year-old adults, but it is unknown whether modality of screening affects uptake in the 45-year-old cohort. Here we examine uptake of the new CRC screening in 45-year-olds within the Department of Veteran Affairs (VA) and associations with stool-based versus endoscopic-based modalities.
Methods: The Veterans Aging Cohort Study-National represents all individuals who have accessed VA care since 2000. All care delivered within the VA system is stored in a central repository called the Corporate Data Warehouse.
The study included all individuals who turned 45 years of age on or after May 21, 2021 and met criteria for average risk of CRC. Analyses focused on individuals engaged in clinical care, defined as having a visit within the two years prior to becoming eligible for screening. The cohort was stratified by the year after May 21, 2021 in which individuals turned 45. Cumulative incidence for screening completion and screening completion by stool-based and endoscopic-based modalities were calculated using the cmprsk package in R.
Results: 182,616 patients met study inclusion criteria. Cumulative incidence of completed screening showed year-on-year increases (Figure 1). This increase was predominantly due to a change in cumulative incidence of screening completion through stool-based testing (p< 0.001), with cumulative incidence of screening completion by endoscopic methods remaining similar across groups (p=0.53).
Discussion: Adherence to guidelines in screening of newly eligible 45-year-olds has increased since the recommendation change in 2021. Year-on-year improvements are associated with increased use of stool-based testing. These findings are likely multifactorial and may be driven by changes in patient and provider awareness, screening programs, and changes in access to preferred screening methods. Future work should investigate whether this uptake is uniform across subpopulations and extends beyond first time screening to re-screening.
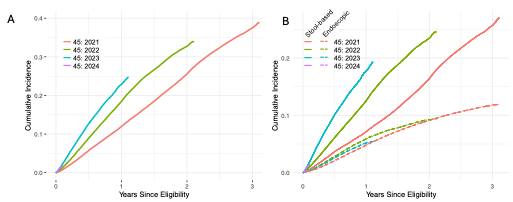
Figure: Cumulative incidence of screening across age cohorts. A. Cumulative incidence of screening completion across all modalities. B. Modality-specific cumulative incidence for stool-based (solid) and endoscopic (dashed) methods.
Disclosures:
Sarah Householder indicated no relevant financial relationships.
Andrew Loza indicated no relevant financial relationships.
Jason Dominitz indicated no relevant financial relationships.
Louise Davies indicated no relevant financial relationships.
Amy Justice indicated no relevant financial relationships.
Christopher Rentsch indicated no relevant financial relationships.
Sarah Householder, MD1, Andrew Loza, MD, PhD2, Jason Dominitz, MD, MHS3, Louise Davies, MD, MS4, Amy Justice, MD, PhD2, Christopher Rentsch, PhD2. P2656 - Use of Stool-Based Tests Is Associated With Increased Uptake of the 2021 USPSTF Colorectal Cancer Screening Guidelines, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
