Monday Poster Session
Category: Esophagus
P2753 - Comparative Outcomes of GE Junction Cancer in Patients With Barrett's Esophagus versus GERD: A Real-World Data Analysis Using the TriNetX Network
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ashujot K. Dang, MD
University of California Riverside School of Medicine
Riverside, CA
Presenting Author(s)
Ashujot K. Dang, MD1, Vikash Kumar, MD2, Aalam Sohal, MD2, Angad Mann, MD3, Pir Shah, MD4, Sunny Kumar, MD5, Indu Srinivasan, MD2, Wael Youssef, MD2
1University of California Riverside School of Medicine, Riverside, CA; 2Creighton University School of Medicine, Phoenix, AZ; 3University of California Riverside School of Medicine, Rancho Cucamonga, CA; 4Creighton University Medical Center, Phoenix, AZ; 5Wright Center for Graduate Medical Education, Scranton, PA
Introduction: Barrett’s esophagus (BE) is a known precursor to esophageal adenocarcinoma, yet the differential risk of gastroesophageal (GE) junction cancer in BE versus gastroesophageal reflux disease (GERD) without BE remains underexplored. This study aims to leverage a large multi-institutional database to assess the comparative incidence and outcomes of GE junction malignancies among these populations.
Methods: A retrospective cohort analysis was conducted using the TriNetX US Collaborative Network database comprising 69 healthcare organizations. Adults (≥18 years) with BE (Cohort 1, n=397,409) or GERD without BE (Cohort 2, n=9,824,193) were identified using ICD-10 codes. After 1:1 propensity score matching for demographics, diagnoses, and medications, each cohort included 391,695 patients. Outcomes analyzed included GE junction cancer, 5-year mortality, metastases, and chemotherapy use. Measures of association and Kaplan-Meier survival analyses were performed.
Results: Incidence of GE junction cancer was significantly higher in the BE cohort (1.9%) compared to GERD (0.3%), with a risk ratio of 5.86 (95% CI: 5.52–6.21, p< 0.001). Kaplan-Meier analysis showed lower survival probability in BE patients (96.37% vs. 99.37%, p< 0.001). Five-year mortality was slightly lower in BE (10.5%) versus GERD (11.4%) with a hazard ratio (HR) of 0.84 (95% CI: 0.83–0.85, p< 0.001). Metastatic disease was also slightly lower in BE (3.2% vs. 3.7%, HR: 0.82, p< 0.001). Chemotherapy use was marginally lower in BE (0.8% vs. 0.9%, HR: 0.85, p< 0.001).
Discussion: Patients with Barrett’s esophagus have a markedly higher risk of developing GE junction cancer compared to those with GERD alone, underscoring the need for vigilant surveillance. Interestingly, BE patients showed slightly better long-term survival outcomes and lower rates of metastases and chemotherapy utilization, warranting further investigation into disease biology and treatment patterns.
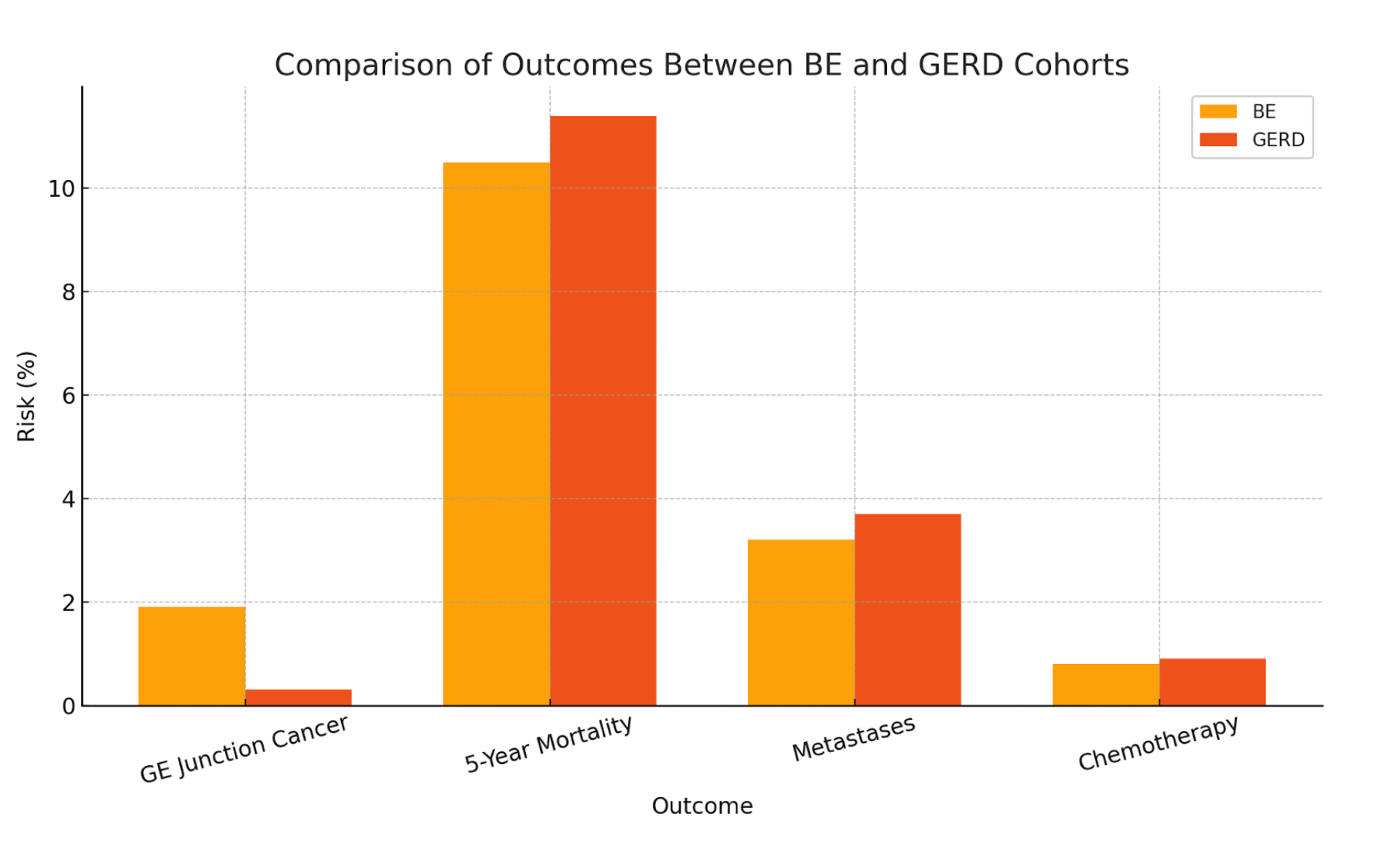
Figure: Comparison of outcomes between BE and GERD cohorts
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Angad Mann indicated no relevant financial relationships.
Pir Shah indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Wael Youssef indicated no relevant financial relationships.
Ashujot K. Dang, MD1, Vikash Kumar, MD2, Aalam Sohal, MD2, Angad Mann, MD3, Pir Shah, MD4, Sunny Kumar, MD5, Indu Srinivasan, MD2, Wael Youssef, MD2. P2753 - Comparative Outcomes of GE Junction Cancer in Patients With Barrett's Esophagus versus GERD: A Real-World Data Analysis Using the TriNetX Network, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Riverside School of Medicine, Riverside, CA; 2Creighton University School of Medicine, Phoenix, AZ; 3University of California Riverside School of Medicine, Rancho Cucamonga, CA; 4Creighton University Medical Center, Phoenix, AZ; 5Wright Center for Graduate Medical Education, Scranton, PA
Introduction: Barrett’s esophagus (BE) is a known precursor to esophageal adenocarcinoma, yet the differential risk of gastroesophageal (GE) junction cancer in BE versus gastroesophageal reflux disease (GERD) without BE remains underexplored. This study aims to leverage a large multi-institutional database to assess the comparative incidence and outcomes of GE junction malignancies among these populations.
Methods: A retrospective cohort analysis was conducted using the TriNetX US Collaborative Network database comprising 69 healthcare organizations. Adults (≥18 years) with BE (Cohort 1, n=397,409) or GERD without BE (Cohort 2, n=9,824,193) were identified using ICD-10 codes. After 1:1 propensity score matching for demographics, diagnoses, and medications, each cohort included 391,695 patients. Outcomes analyzed included GE junction cancer, 5-year mortality, metastases, and chemotherapy use. Measures of association and Kaplan-Meier survival analyses were performed.
Results: Incidence of GE junction cancer was significantly higher in the BE cohort (1.9%) compared to GERD (0.3%), with a risk ratio of 5.86 (95% CI: 5.52–6.21, p< 0.001). Kaplan-Meier analysis showed lower survival probability in BE patients (96.37% vs. 99.37%, p< 0.001). Five-year mortality was slightly lower in BE (10.5%) versus GERD (11.4%) with a hazard ratio (HR) of 0.84 (95% CI: 0.83–0.85, p< 0.001). Metastatic disease was also slightly lower in BE (3.2% vs. 3.7%, HR: 0.82, p< 0.001). Chemotherapy use was marginally lower in BE (0.8% vs. 0.9%, HR: 0.85, p< 0.001).
Discussion: Patients with Barrett’s esophagus have a markedly higher risk of developing GE junction cancer compared to those with GERD alone, underscoring the need for vigilant surveillance. Interestingly, BE patients showed slightly better long-term survival outcomes and lower rates of metastases and chemotherapy utilization, warranting further investigation into disease biology and treatment patterns.
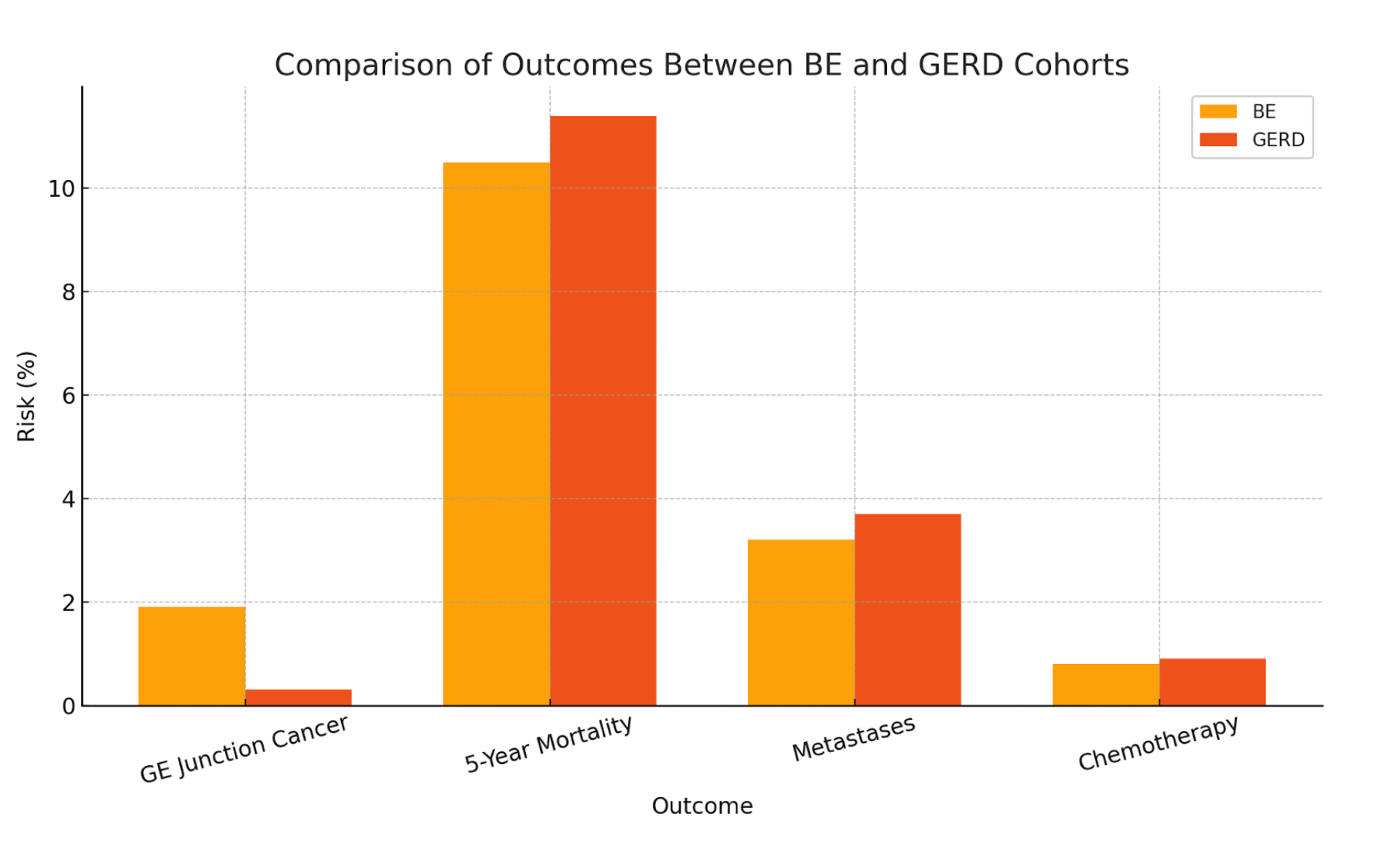
Figure: Comparison of outcomes between BE and GERD cohorts
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Angad Mann indicated no relevant financial relationships.
Pir Shah indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Wael Youssef indicated no relevant financial relationships.
Ashujot K. Dang, MD1, Vikash Kumar, MD2, Aalam Sohal, MD2, Angad Mann, MD3, Pir Shah, MD4, Sunny Kumar, MD5, Indu Srinivasan, MD2, Wael Youssef, MD2. P2753 - Comparative Outcomes of GE Junction Cancer in Patients With Barrett's Esophagus versus GERD: A Real-World Data Analysis Using the TriNetX Network, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
