Monday Poster Session
Category: Esophagus
P2750 - Assess Comparative Efficacy, Quality-of-life Impact, Safety Profile, and Onset of Action of Proton Pump Inhibitors (PPIs) vs Antacids in Adults with Rome IV-defined Non-erosive Reflux Disease (NERD): A Meta-Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Chanpreet Singh, MD (he/him/his)
South Texas Health System GME Consortium
McAllen, TX
Presenting Author(s)
Chanpreet Singh, MD1, Sai Nikhitha Malapati, MBBS2, Ibrahim Reyaz, MBBS3, Priya Kumari Maheshwari, MD4, Aasim Akthar Ahmed, MD5, Arghadip Das, MBBS6, Sheenam Garg, MBBS7, Saif Syed, MD8, Mohammad Ali, MBBS9, Binay Panjiyar, MD10, Omer Farooq Mohammed, MBBS11, Mourad M. Alsabbagh, MD12
1South Texas Health System GME Consortium, McAllen, TX; 2kamineni academy of medical sciences and research center, lb.nagar, hyderabad, india, Hyderabad, Telangana, India; 3Nassau University Medical Center, East Meadow, NY; 4University of Central Florida, HCA Healthcare GME, Pensacola, FL; 5St. Francis Medical Center, Monroe, LA; 6Nilratan Sircar Medical College and Hospital, Kolkata, West Bengal, India; 7Punjab Institute of Medical Sciences, Centreville, VA; 8Indiana University Health, Indiana, IN; 9Kakatiya Medical College, Hyderabad, Telangana, India; 10NorthShore University Hospital, Manhasset, NY; 11Osmania General Hospital and Medical College, Hyderabad, Telangana, India; 12South Texas Health System, Edinburg, TX
Introduction: To assess the comparative efficacy, quality-of-life impact, safety profile, and onset of action of proton pump inhibitors (PPIs) versus antacids in adults with Rome IV-defined non-erosive reflux disease (NERD), using only low-heterogeneity, low-bias randomized controlled trials (RCTs).
Methods: A systematic review and meta-analysis was conducted using PubMed, EMBASE, and Cochrane databases (2015–2023). Eligible studies directly compared esomeprazole or pantoprazole to Mg/Al-based antacids in adult NERD populations meeting Rome IV criteria. Primary outcomes included symptom relief (RR) and GERD-specific quality of life (GERD-HRQL). Secondary outcomes included adverse events (RD) and onset of symptom relief (HR). Risk of bias was assessed using Cochrane ROB 2.0.
Results: 1,624 records screened, 8 RCTs (n=4,850) were included. All had low risk of bias and heterogeneity (I² < 25%). PPIs significantly improved 8-week symptom relief over antacids (RR 1.42, 95% CI 1.31–1.54; I² = 11%). Quality of life also favored PPIs (MD 2.27, 95% CI 2.23–3.31; I² = 0%). PPIs were associated with increased risk of hypomagnesemia (RD 0.09, 95% CI 0.05–0.12), while antacids had a slightly higher incidence of diarrhea (RD –0.08, 95% CI –0.16 to –0.01). Antacids acted significantly faster (HR 0.14, 95% CI 0.07–0.28).
Discussion: PPIs remain superior for long-term symptom control and quality of life in NERD, though antacids provide faster onset and are better tolerated in some populations. A sequential approach—initiating PPIs for sustained control with antacid rescue—may balance efficacy and tolerability. Recent impedance-pH studies further classify NERD into acid-sensitive, weakly acidic, and functional heartburn subtypes, with PPIs effective primarily in acid-sensitive subgroups. This underscores the need for phenotype-specific therapy, which our analysis addresses by isolating Rome IV-defined populations. This meta-analysis provides robust, clinically relevant evidence that proton pump inhibitors (PPIs) offer superior long-term symptom relief and quality-of-life improvement in adults with Rome IV-defined non-erosive reflux disease (NERD). However, magnesium/aluminum-based antacids demonstrate a significantly faster onset of action and may be better tolerated in specific subgroups, such as patients with overlapping functional bowel disorders.
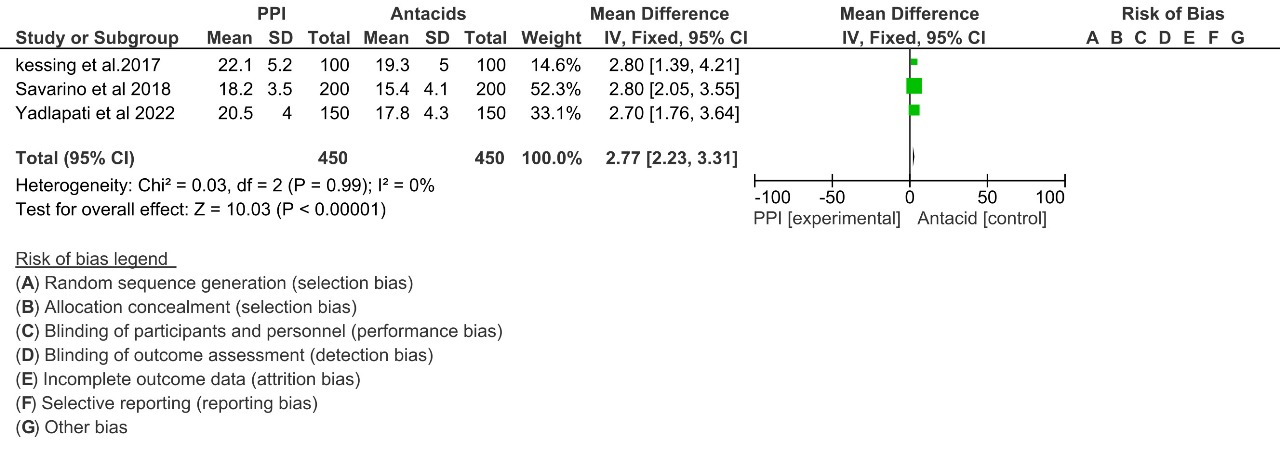
Figure: Forest plot comparing the efficacy of Proton Pump Inhibitors (PPI) versus Antacids across three studies (Kessing et al. 2017, Savarino et al. 2018, Yadlapati et al. 2022). The overall mean difference favors PPI with a fixed-effects model estimate of 2.77 [95% CI: 2.23, 3.31], based on 450 participants in each group. Risk of bias is assessed across seven domains.

Figure: Forest plot from a meta-analysis comparing the efficacy of proton pump inhibitors (PPIs) versus antacids across three studies (Kessing et al. 2017, Savarino et al. 2018, Yadlapati et al. 2022). The overall mean difference favors PPIs with a pooled estimate of 2.77 [2.23, 3.31]. Risk of bias is assessed across seven domains
Disclosures:
Chanpreet Singh indicated no relevant financial relationships.
Sai Nikhitha Malapati indicated no relevant financial relationships.
Ibrahim Reyaz indicated no relevant financial relationships.
Priya Kumari Maheshwari indicated no relevant financial relationships.
Aasim Akthar Ahmed indicated no relevant financial relationships.
Arghadip Das indicated no relevant financial relationships.
Sheenam Garg indicated no relevant financial relationships.
Saif Syed indicated no relevant financial relationships.
Mohammad Ali indicated no relevant financial relationships.
Binay Panjiyar indicated no relevant financial relationships.
Omer Farooq Mohammed indicated no relevant financial relationships.
Mourad M. Alsabbagh indicated no relevant financial relationships.
Chanpreet Singh, MD1, Sai Nikhitha Malapati, MBBS2, Ibrahim Reyaz, MBBS3, Priya Kumari Maheshwari, MD4, Aasim Akthar Ahmed, MD5, Arghadip Das, MBBS6, Sheenam Garg, MBBS7, Saif Syed, MD8, Mohammad Ali, MBBS9, Binay Panjiyar, MD10, Omer Farooq Mohammed, MBBS11, Mourad M. Alsabbagh, MD12. P2750 - Assess Comparative Efficacy, Quality-of-life Impact, Safety Profile, and Onset of Action of Proton Pump Inhibitors (PPIs) vs Antacids in Adults with Rome IV-defined Non-erosive Reflux Disease (NERD): A Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1South Texas Health System GME Consortium, McAllen, TX; 2kamineni academy of medical sciences and research center, lb.nagar, hyderabad, india, Hyderabad, Telangana, India; 3Nassau University Medical Center, East Meadow, NY; 4University of Central Florida, HCA Healthcare GME, Pensacola, FL; 5St. Francis Medical Center, Monroe, LA; 6Nilratan Sircar Medical College and Hospital, Kolkata, West Bengal, India; 7Punjab Institute of Medical Sciences, Centreville, VA; 8Indiana University Health, Indiana, IN; 9Kakatiya Medical College, Hyderabad, Telangana, India; 10NorthShore University Hospital, Manhasset, NY; 11Osmania General Hospital and Medical College, Hyderabad, Telangana, India; 12South Texas Health System, Edinburg, TX
Introduction: To assess the comparative efficacy, quality-of-life impact, safety profile, and onset of action of proton pump inhibitors (PPIs) versus antacids in adults with Rome IV-defined non-erosive reflux disease (NERD), using only low-heterogeneity, low-bias randomized controlled trials (RCTs).
Methods: A systematic review and meta-analysis was conducted using PubMed, EMBASE, and Cochrane databases (2015–2023). Eligible studies directly compared esomeprazole or pantoprazole to Mg/Al-based antacids in adult NERD populations meeting Rome IV criteria. Primary outcomes included symptom relief (RR) and GERD-specific quality of life (GERD-HRQL). Secondary outcomes included adverse events (RD) and onset of symptom relief (HR). Risk of bias was assessed using Cochrane ROB 2.0.
Results: 1,624 records screened, 8 RCTs (n=4,850) were included. All had low risk of bias and heterogeneity (I² < 25%). PPIs significantly improved 8-week symptom relief over antacids (RR 1.42, 95% CI 1.31–1.54; I² = 11%). Quality of life also favored PPIs (MD 2.27, 95% CI 2.23–3.31; I² = 0%). PPIs were associated with increased risk of hypomagnesemia (RD 0.09, 95% CI 0.05–0.12), while antacids had a slightly higher incidence of diarrhea (RD –0.08, 95% CI –0.16 to –0.01). Antacids acted significantly faster (HR 0.14, 95% CI 0.07–0.28).
Discussion: PPIs remain superior for long-term symptom control and quality of life in NERD, though antacids provide faster onset and are better tolerated in some populations. A sequential approach—initiating PPIs for sustained control with antacid rescue—may balance efficacy and tolerability. Recent impedance-pH studies further classify NERD into acid-sensitive, weakly acidic, and functional heartburn subtypes, with PPIs effective primarily in acid-sensitive subgroups. This underscores the need for phenotype-specific therapy, which our analysis addresses by isolating Rome IV-defined populations. This meta-analysis provides robust, clinically relevant evidence that proton pump inhibitors (PPIs) offer superior long-term symptom relief and quality-of-life improvement in adults with Rome IV-defined non-erosive reflux disease (NERD). However, magnesium/aluminum-based antacids demonstrate a significantly faster onset of action and may be better tolerated in specific subgroups, such as patients with overlapping functional bowel disorders.
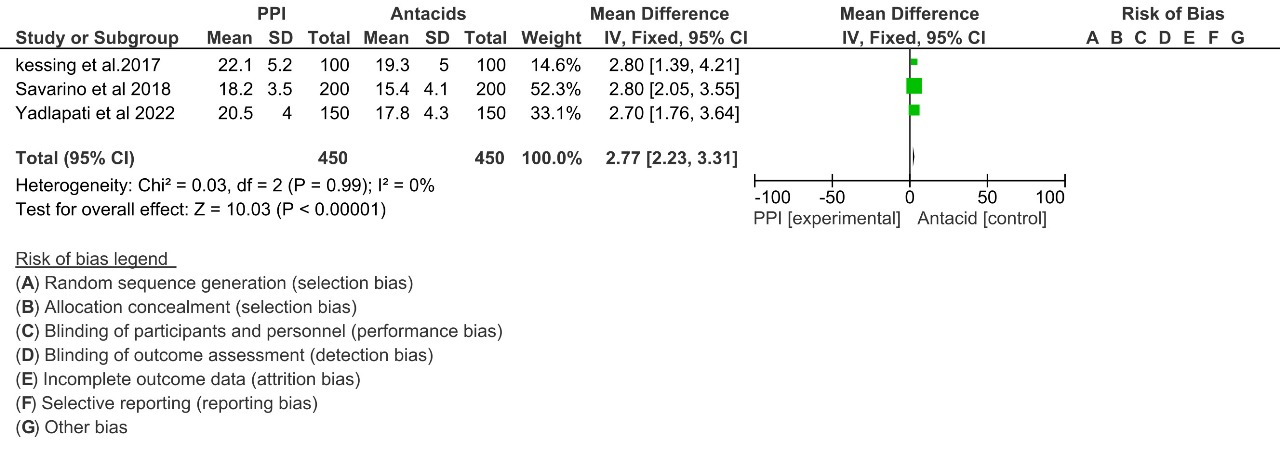
Figure: Forest plot comparing the efficacy of Proton Pump Inhibitors (PPI) versus Antacids across three studies (Kessing et al. 2017, Savarino et al. 2018, Yadlapati et al. 2022). The overall mean difference favors PPI with a fixed-effects model estimate of 2.77 [95% CI: 2.23, 3.31], based on 450 participants in each group. Risk of bias is assessed across seven domains.

Figure: Forest plot from a meta-analysis comparing the efficacy of proton pump inhibitors (PPIs) versus antacids across three studies (Kessing et al. 2017, Savarino et al. 2018, Yadlapati et al. 2022). The overall mean difference favors PPIs with a pooled estimate of 2.77 [2.23, 3.31]. Risk of bias is assessed across seven domains
Disclosures:
Chanpreet Singh indicated no relevant financial relationships.
Sai Nikhitha Malapati indicated no relevant financial relationships.
Ibrahim Reyaz indicated no relevant financial relationships.
Priya Kumari Maheshwari indicated no relevant financial relationships.
Aasim Akthar Ahmed indicated no relevant financial relationships.
Arghadip Das indicated no relevant financial relationships.
Sheenam Garg indicated no relevant financial relationships.
Saif Syed indicated no relevant financial relationships.
Mohammad Ali indicated no relevant financial relationships.
Binay Panjiyar indicated no relevant financial relationships.
Omer Farooq Mohammed indicated no relevant financial relationships.
Mourad M. Alsabbagh indicated no relevant financial relationships.
Chanpreet Singh, MD1, Sai Nikhitha Malapati, MBBS2, Ibrahim Reyaz, MBBS3, Priya Kumari Maheshwari, MD4, Aasim Akthar Ahmed, MD5, Arghadip Das, MBBS6, Sheenam Garg, MBBS7, Saif Syed, MD8, Mohammad Ali, MBBS9, Binay Panjiyar, MD10, Omer Farooq Mohammed, MBBS11, Mourad M. Alsabbagh, MD12. P2750 - Assess Comparative Efficacy, Quality-of-life Impact, Safety Profile, and Onset of Action of Proton Pump Inhibitors (PPIs) vs Antacids in Adults with Rome IV-defined Non-erosive Reflux Disease (NERD): A Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
