Monday Poster Session
Category: Esophagus
P2749 - Risk of Esophageal Cancer in Patients With Eosinophilic Esophagitis Compared to Those With GERD: A Propensity Score-Matched Retrospective Cohort Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- FE
Fatima Elmustafa, MBBS
Henry Ford Warren
Warren, MI
Presenting Author(s)
Fatima Elmustafa, MBBS1, Abdellatif Ismail, MD2, Abdelaziz Mohamed, MBBS3, Mohammad Adam, MD, MSc4, Abdelhaleem Sideeg, MD5, Fady Banno, MD6, Yasmin O. Ali, MBBS7, Tasneem Elmustafa, MBBS8, Eelaf Osman, MBBS9, Mohamed Abdallah, MD10, Mohammad Bilal, MD, FACG11
1Henry Ford Warren, Warren, MI; 2University of Maryland, Baltimore, MD; 3One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 4University of Missouri-Kansas City, Kansas City, MO; 5Virginia Mason Franciscan Health, Seattle, WA; 6Carewell Health William Beaumont Hospital, Royal Oak, MI; 7Hennepin Healthcare, Minneapolis, MN; 8Omdurman Islamic University, Al Rashidiya, Ajman, United Arab Emirates; 9University of Khartoum, Riyadh, Ar Riyad, Saudi Arabia; 10Corewell Health, Royal Oak, MI; 11University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Eosinophilic esophagitis (EoE) is a chronic immune-mediated condition increasingly recognized in recent decades. While chronic inflammation is linked to cancer risk, data on the association between EoE and esophageal cancer (EC) are limited and inconclusive. This study evaluated the 10-year risk of EC in patients with EoE compared to those with gastroesophageal reflux disease (GERD) using a large population-based dataset.
Methods: We conducted a retrospective cohort study using TriNetX, a global federated health research network aggregating de-identified electronic health records. Adult patients diagnosed with EoE between April 2015 and April 2025 were identified as cases. A control cohort comprised patients with a history of gastroesophageal reflux disease (GERD). One-to-one propensity score matching was used to balance demographics, alcohol use, nicotine dependence, and Barrett’s esophagus. The primary outcome was the risk of EC within 10 years. Secondary outcomes included surgical excision rates, esophageal stenting, frequency of endoscopic resections, use of esophageal dilation procedures, and all-cause mortality. Relative risk (RR) and 95% confidence intervals (CI) were calculated, and a two-sided p-value < 0.05 was considered statistically significant.
Results: Prior to matching, 93,056 patients with EoE and 8,127,510 with GERD were identified. After propensity score matching, 93,056 patients remained in each group with mean age (43.3 ± 16.4 years), female sex (41.6%), and comparable rates of nicotine dependence (6.5%), alcohol use (2.6%), and Barrett’s esophagus (2.8%). Over a 10-year follow-up, esophageal cancer developed in 99 EoE patients (0.1%) and 102 GERD patients (0.1%), with no significant difference between groups (RR 0.97, 95% CI 0.737–1.280; p=0.836). No variation was seen across esophageal cancer subtypes. Surgical excision and stenting rates were similar, while endoscopic resections and dilation procedures were more frequent in the EoE group. All-cause mortality was higher among GERD patients.
Discussion: In this large, matched cohort study, no increased risk of esophageal cancer was observed in patients with EoE compared to those with GERD over a 10-year period. These findings are consistent with prior smaller studies and suggest that despite the chronic inflammation seen in EoE, it may not confer an elevated malignancy risk.
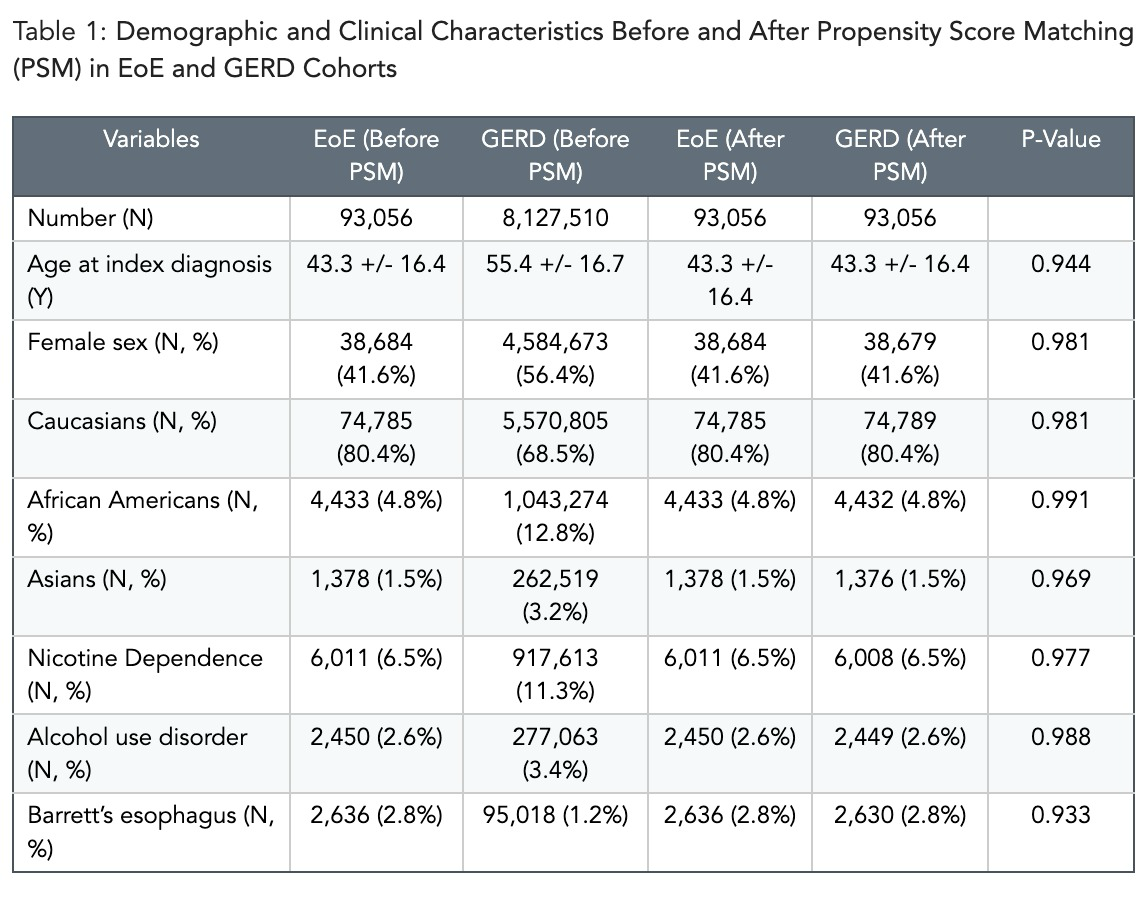
Figure: Table 1: Demographic and Clinical Characteristics Before and After Propensity Score Matching (PSM) in EoE and GERD Cohorts
Disclosures:
Fatima Elmustafa indicated no relevant financial relationships.
Abdellatif Ismail indicated no relevant financial relationships.
Abdelaziz Mohamed indicated no relevant financial relationships.
Mohammad Adam indicated no relevant financial relationships.
Abdelhaleem Sideeg indicated no relevant financial relationships.
Fady Banno indicated no relevant financial relationships.
Yasmin Ali indicated no relevant financial relationships.
Tasneem Elmustafa indicated no relevant financial relationships.
Eelaf Osman indicated no relevant financial relationships.
Mohamed Abdallah indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Fatima Elmustafa, MBBS1, Abdellatif Ismail, MD2, Abdelaziz Mohamed, MBBS3, Mohammad Adam, MD, MSc4, Abdelhaleem Sideeg, MD5, Fady Banno, MD6, Yasmin O. Ali, MBBS7, Tasneem Elmustafa, MBBS8, Eelaf Osman, MBBS9, Mohamed Abdallah, MD10, Mohammad Bilal, MD, FACG11. P2749 - Risk of Esophageal Cancer in Patients With Eosinophilic Esophagitis Compared to Those With GERD: A Propensity Score-Matched Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Henry Ford Warren, Warren, MI; 2University of Maryland, Baltimore, MD; 3One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 4University of Missouri-Kansas City, Kansas City, MO; 5Virginia Mason Franciscan Health, Seattle, WA; 6Carewell Health William Beaumont Hospital, Royal Oak, MI; 7Hennepin Healthcare, Minneapolis, MN; 8Omdurman Islamic University, Al Rashidiya, Ajman, United Arab Emirates; 9University of Khartoum, Riyadh, Ar Riyad, Saudi Arabia; 10Corewell Health, Royal Oak, MI; 11University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Eosinophilic esophagitis (EoE) is a chronic immune-mediated condition increasingly recognized in recent decades. While chronic inflammation is linked to cancer risk, data on the association between EoE and esophageal cancer (EC) are limited and inconclusive. This study evaluated the 10-year risk of EC in patients with EoE compared to those with gastroesophageal reflux disease (GERD) using a large population-based dataset.
Methods: We conducted a retrospective cohort study using TriNetX, a global federated health research network aggregating de-identified electronic health records. Adult patients diagnosed with EoE between April 2015 and April 2025 were identified as cases. A control cohort comprised patients with a history of gastroesophageal reflux disease (GERD). One-to-one propensity score matching was used to balance demographics, alcohol use, nicotine dependence, and Barrett’s esophagus. The primary outcome was the risk of EC within 10 years. Secondary outcomes included surgical excision rates, esophageal stenting, frequency of endoscopic resections, use of esophageal dilation procedures, and all-cause mortality. Relative risk (RR) and 95% confidence intervals (CI) were calculated, and a two-sided p-value < 0.05 was considered statistically significant.
Results: Prior to matching, 93,056 patients with EoE and 8,127,510 with GERD were identified. After propensity score matching, 93,056 patients remained in each group with mean age (43.3 ± 16.4 years), female sex (41.6%), and comparable rates of nicotine dependence (6.5%), alcohol use (2.6%), and Barrett’s esophagus (2.8%). Over a 10-year follow-up, esophageal cancer developed in 99 EoE patients (0.1%) and 102 GERD patients (0.1%), with no significant difference between groups (RR 0.97, 95% CI 0.737–1.280; p=0.836). No variation was seen across esophageal cancer subtypes. Surgical excision and stenting rates were similar, while endoscopic resections and dilation procedures were more frequent in the EoE group. All-cause mortality was higher among GERD patients.
Discussion: In this large, matched cohort study, no increased risk of esophageal cancer was observed in patients with EoE compared to those with GERD over a 10-year period. These findings are consistent with prior smaller studies and suggest that despite the chronic inflammation seen in EoE, it may not confer an elevated malignancy risk.
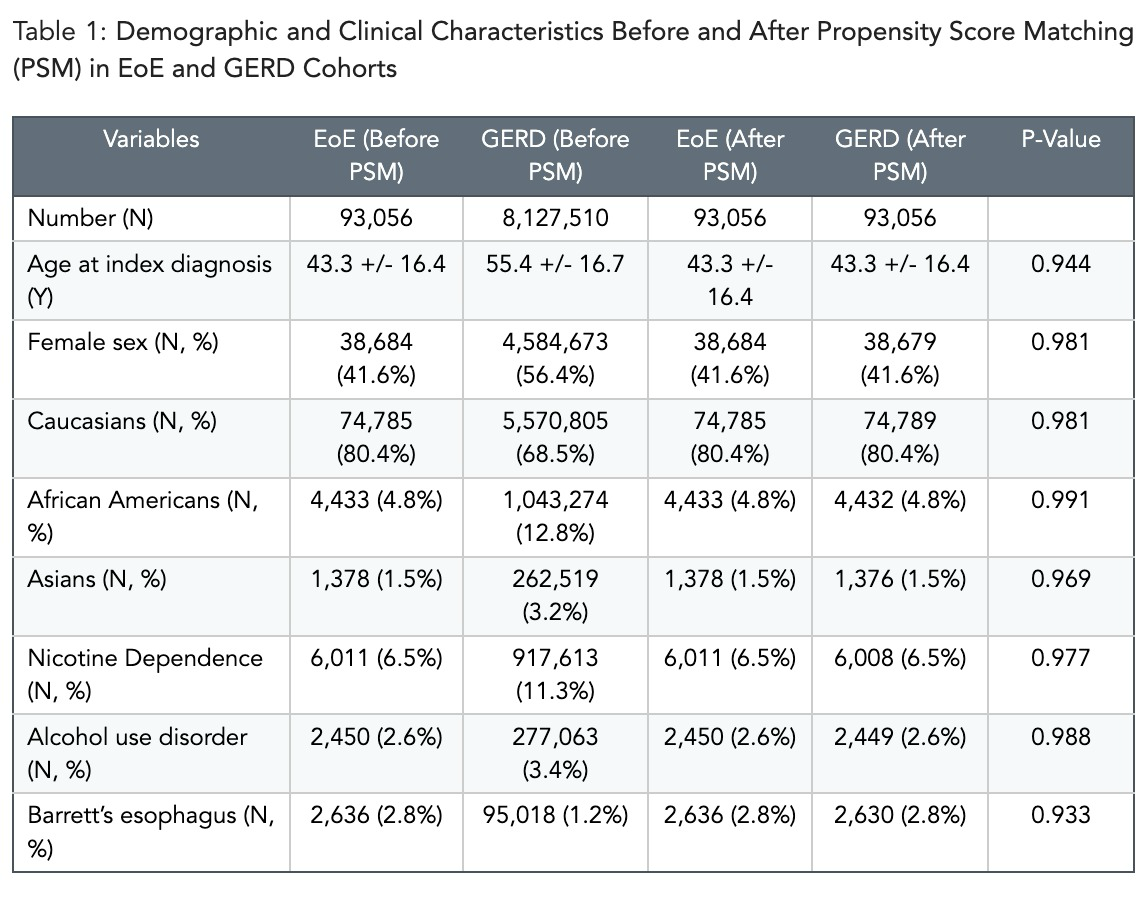
Figure: Table 1: Demographic and Clinical Characteristics Before and After Propensity Score Matching (PSM) in EoE and GERD Cohorts
Disclosures:
Fatima Elmustafa indicated no relevant financial relationships.
Abdellatif Ismail indicated no relevant financial relationships.
Abdelaziz Mohamed indicated no relevant financial relationships.
Mohammad Adam indicated no relevant financial relationships.
Abdelhaleem Sideeg indicated no relevant financial relationships.
Fady Banno indicated no relevant financial relationships.
Yasmin Ali indicated no relevant financial relationships.
Tasneem Elmustafa indicated no relevant financial relationships.
Eelaf Osman indicated no relevant financial relationships.
Mohamed Abdallah indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Fatima Elmustafa, MBBS1, Abdellatif Ismail, MD2, Abdelaziz Mohamed, MBBS3, Mohammad Adam, MD, MSc4, Abdelhaleem Sideeg, MD5, Fady Banno, MD6, Yasmin O. Ali, MBBS7, Tasneem Elmustafa, MBBS8, Eelaf Osman, MBBS9, Mohamed Abdallah, MD10, Mohammad Bilal, MD, FACG11. P2749 - Risk of Esophageal Cancer in Patients With Eosinophilic Esophagitis Compared to Those With GERD: A Propensity Score-Matched Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
