Monday Poster Session
Category: Esophagus
P2747 - Prevalence of Barrett's Esophagus in Latin American Countries: A Systematic Review and Meta-Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Wilfor Diaz Fernandez, MD (he/him/his)
Mayo Clinic
Rochester, MN
Presenting Author(s)
Wilfor Diaz Fernandez, MD1, Vanessa Pamela Salolin-Vargas, MD2, Huber Padilla Zambrano, MD3, Michele McGinnis, MS4, Cadman Leggett, MD4
1Mayo Clinic, Boston, MA; 2Gastroenterology Consultants, Mexico City, Distrito Federal, Mexico; 3Emura Center Latinoamerica, New York, NY; 4Mayo Clinic, Rochester, MN
Introduction: Barrett’s esophagus (BE), a well-established precursor to esophageal adenocarcinoma (EAC), necessitates a thorough understanding of its epidemiology to guide effective screening and surveillance strategies. However, the prevalence of BE across Latin America remains poorly characterized, with existing studies reporting highly variable estimates. To address this gap, we conducted a systematic review and meta-analysis to evaluate the prevalence of BE in Latin America and identify associated risk factors.
Methods: Two investigators independently conducted a comprehensive literature search across PubMed, Embase, Web of Science, LILACS, SciELO, and MEDLINE databases to identify studies published from database inception through December 2024. Eligible studies included adults aged ≥18 years with histologically confirmed BE, sample sizes exceeding 100 individuals, and geographic focus on Latin America. The region was subcategorized into North/Central America, the Caribbean, and South America. Pooled BE prevalence estimates were calculated using a random-effects model to account for heterogeneity across studies.
Results: A total of 28 eligible studies (N = 148,595) from Latin America were identified. The overall pooled prevalence of histologically confirmed BE was 0.09% (95% confidence interval [CI]: 0.04 -- 0.20) with substantial heterogeneity (I² = 96%), based on a random-effects model. Within BE groups, hiatal hernia (HH) were associated with a significantly increased risk of histologic BE compared with patients without BE. Male sex was not significantly associated with histologic BE. Subgroup analyses, such as prevalence trends over time, could not be estimated based on published data.
Discussion: BE is not uncommon in Latin American countries, with a prevalence similar to western countries. However, we identified significant differences about the definition of BE and endoscopic practices which could have affected our results. The prevalence of HH was comparable to that of BE, with a relative risk (RR) of 0.68 (95% CI: 0.59–0.78). This finding aligns with prior studies, reinforcing the notion that HH is a significant risk factor for BE. The RR of BE according to gender was 1.07 (95% CI: 0.96–1.20), suggesting no significant difference between men and women which differs from prior reports. The observed variability and potential bias underscore the need for standardized studies across understudied subregions to refine prevalence estimates and optimize early detection strategies for EAC.
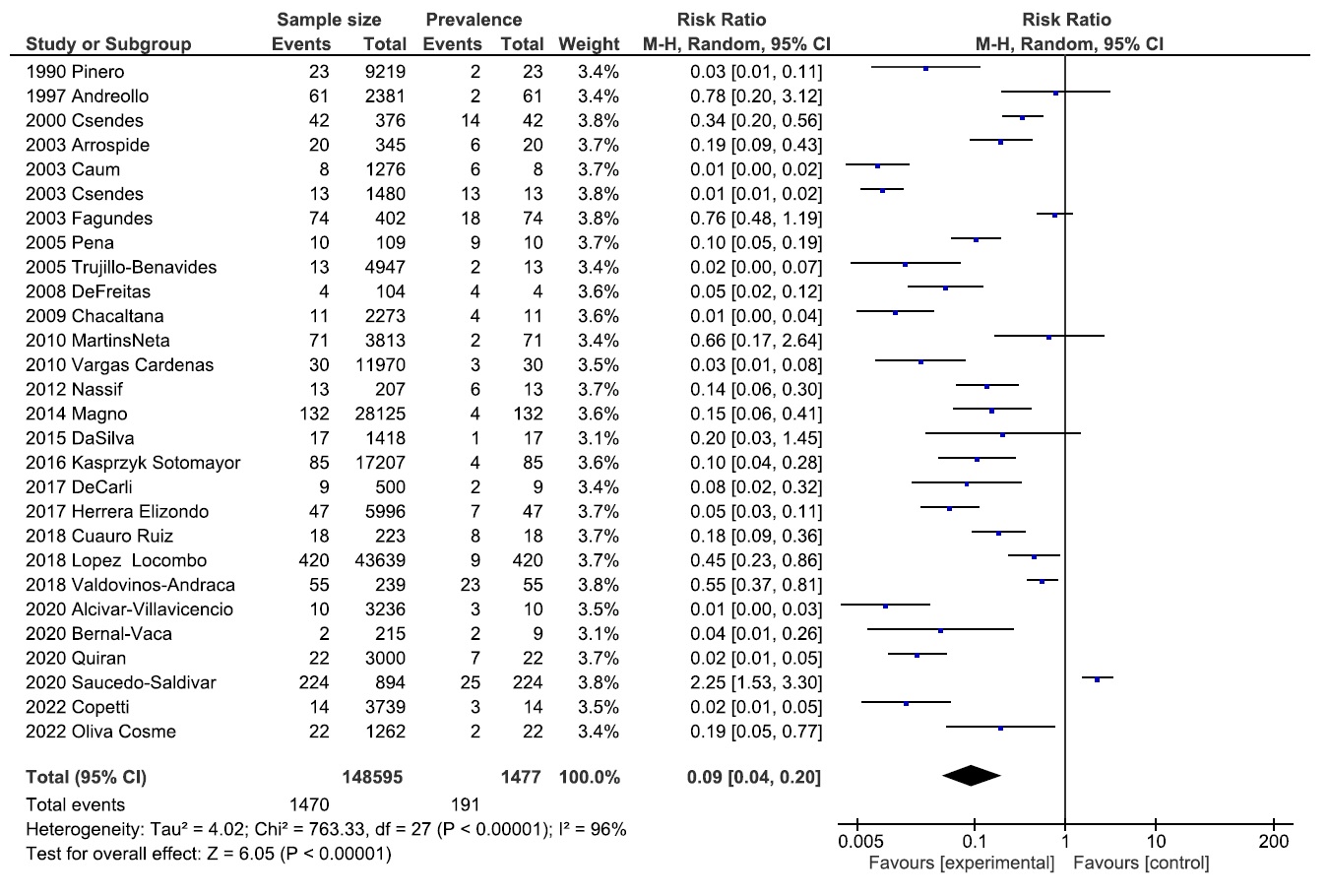
Figure: Figure 1. Pooled prevalence of Barrett's esophagus in Latin America.
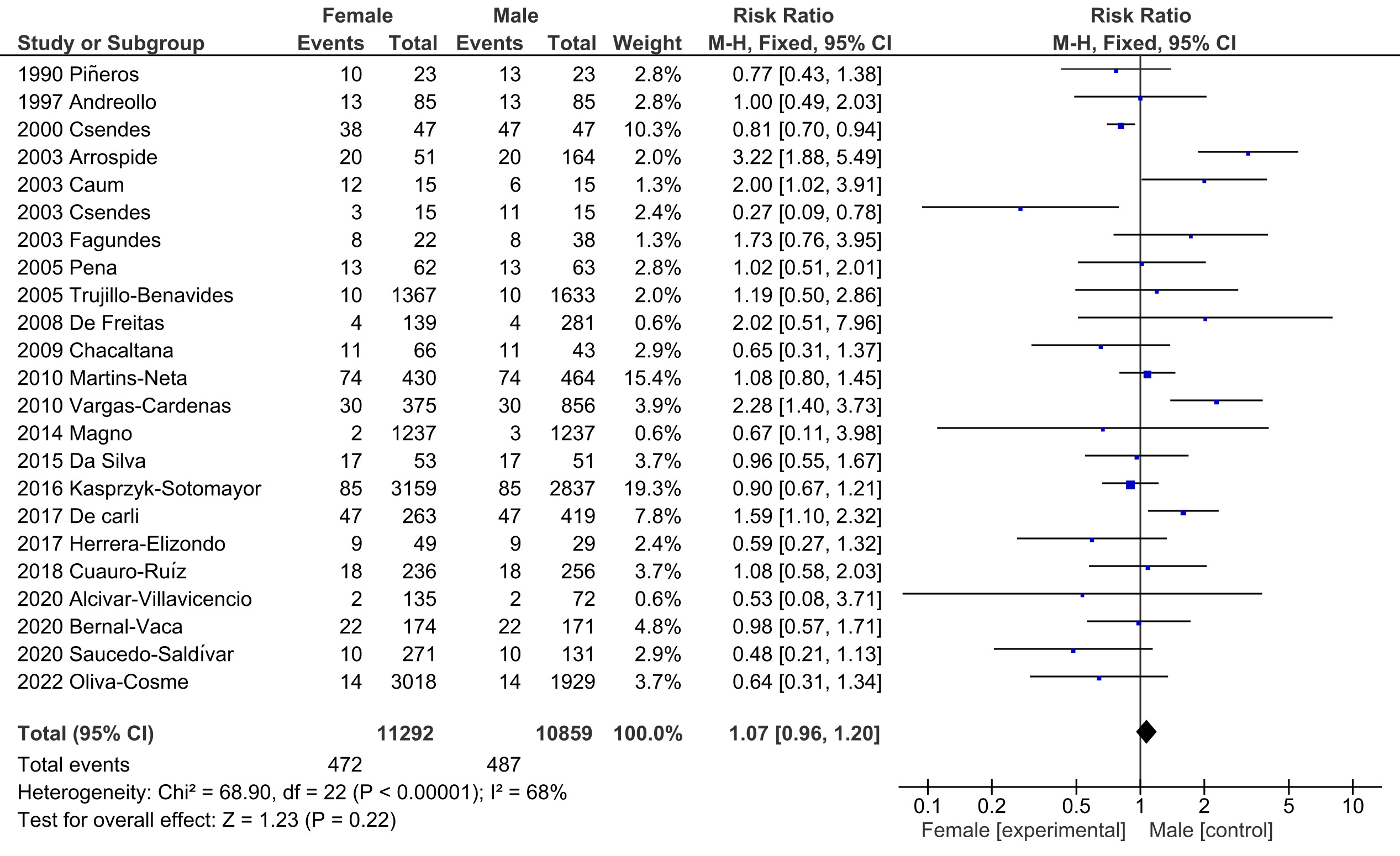
Figure: Figure 2: Risk of Histologic Barrett's Esophagus based on Gender.
Disclosures:
Wilfor Diaz Fernandez indicated no relevant financial relationships.
Vanessa Pamela Salolin-Vargas indicated no relevant financial relationships.
Huber Padilla Zambrano indicated no relevant financial relationships.
Michele McGinnis indicated no relevant financial relationships.
Cadman Leggett indicated no relevant financial relationships.
Wilfor Diaz Fernandez, MD1, Vanessa Pamela Salolin-Vargas, MD2, Huber Padilla Zambrano, MD3, Michele McGinnis, MS4, Cadman Leggett, MD4. P2747 - Prevalence of Barrett's Esophagus in Latin American Countries: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Boston, MA; 2Gastroenterology Consultants, Mexico City, Distrito Federal, Mexico; 3Emura Center Latinoamerica, New York, NY; 4Mayo Clinic, Rochester, MN
Introduction: Barrett’s esophagus (BE), a well-established precursor to esophageal adenocarcinoma (EAC), necessitates a thorough understanding of its epidemiology to guide effective screening and surveillance strategies. However, the prevalence of BE across Latin America remains poorly characterized, with existing studies reporting highly variable estimates. To address this gap, we conducted a systematic review and meta-analysis to evaluate the prevalence of BE in Latin America and identify associated risk factors.
Methods: Two investigators independently conducted a comprehensive literature search across PubMed, Embase, Web of Science, LILACS, SciELO, and MEDLINE databases to identify studies published from database inception through December 2024. Eligible studies included adults aged ≥18 years with histologically confirmed BE, sample sizes exceeding 100 individuals, and geographic focus on Latin America. The region was subcategorized into North/Central America, the Caribbean, and South America. Pooled BE prevalence estimates were calculated using a random-effects model to account for heterogeneity across studies.
Results: A total of 28 eligible studies (N = 148,595) from Latin America were identified. The overall pooled prevalence of histologically confirmed BE was 0.09% (95% confidence interval [CI]: 0.04 -- 0.20) with substantial heterogeneity (I² = 96%), based on a random-effects model. Within BE groups, hiatal hernia (HH) were associated with a significantly increased risk of histologic BE compared with patients without BE. Male sex was not significantly associated with histologic BE. Subgroup analyses, such as prevalence trends over time, could not be estimated based on published data.
Discussion: BE is not uncommon in Latin American countries, with a prevalence similar to western countries. However, we identified significant differences about the definition of BE and endoscopic practices which could have affected our results. The prevalence of HH was comparable to that of BE, with a relative risk (RR) of 0.68 (95% CI: 0.59–0.78). This finding aligns with prior studies, reinforcing the notion that HH is a significant risk factor for BE. The RR of BE according to gender was 1.07 (95% CI: 0.96–1.20), suggesting no significant difference between men and women which differs from prior reports. The observed variability and potential bias underscore the need for standardized studies across understudied subregions to refine prevalence estimates and optimize early detection strategies for EAC.
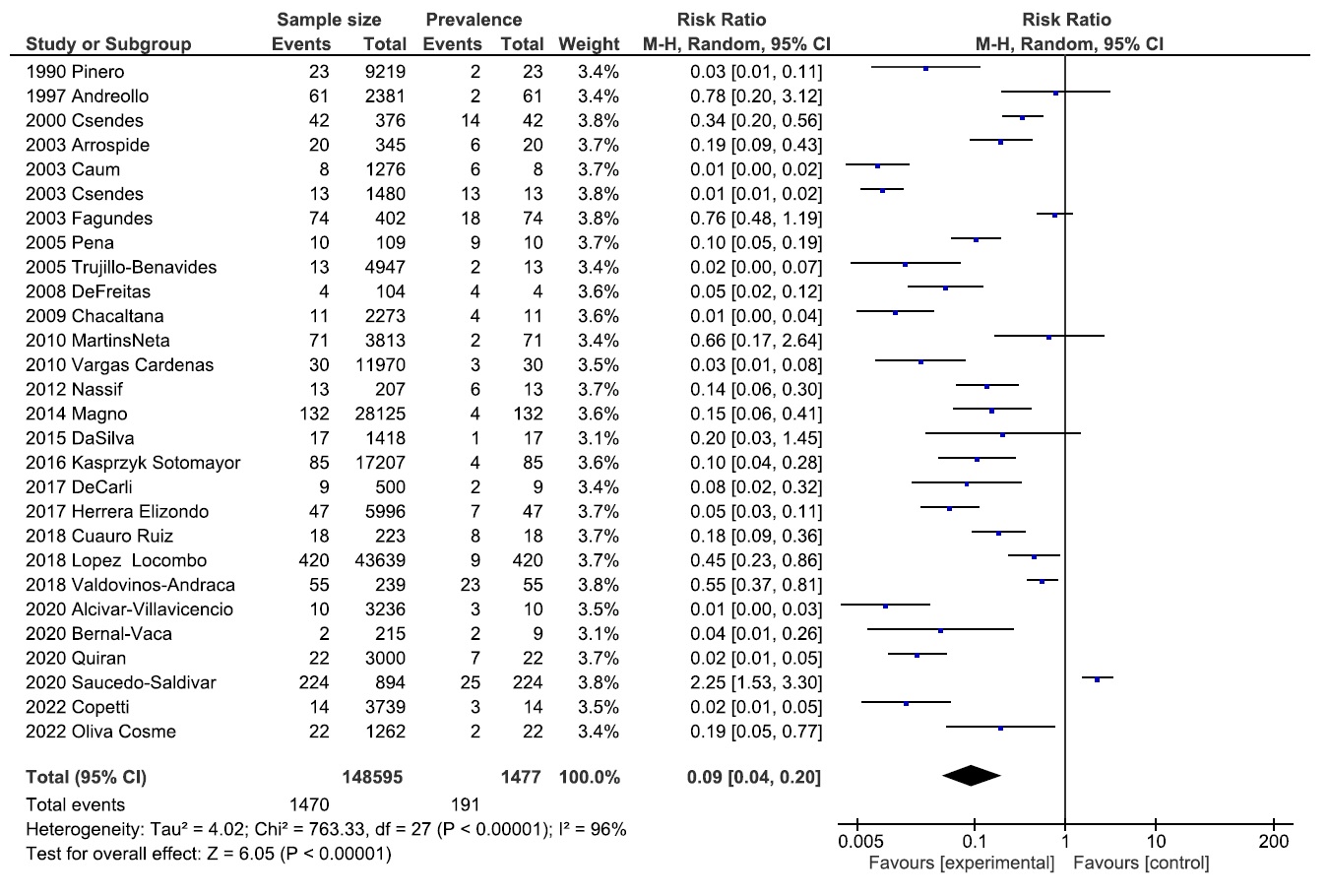
Figure: Figure 1. Pooled prevalence of Barrett's esophagus in Latin America.
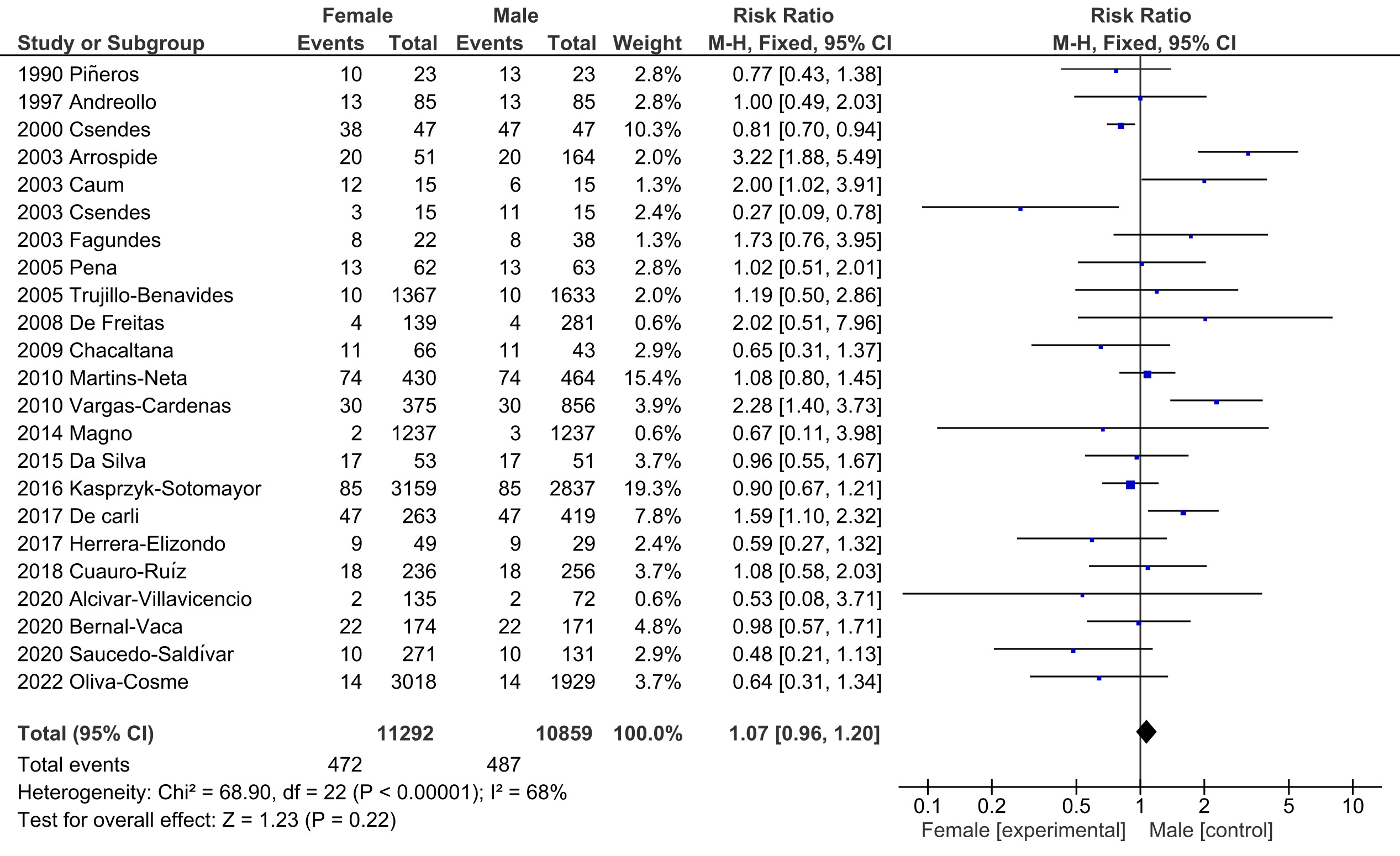
Figure: Figure 2: Risk of Histologic Barrett's Esophagus based on Gender.
Disclosures:
Wilfor Diaz Fernandez indicated no relevant financial relationships.
Vanessa Pamela Salolin-Vargas indicated no relevant financial relationships.
Huber Padilla Zambrano indicated no relevant financial relationships.
Michele McGinnis indicated no relevant financial relationships.
Cadman Leggett indicated no relevant financial relationships.
Wilfor Diaz Fernandez, MD1, Vanessa Pamela Salolin-Vargas, MD2, Huber Padilla Zambrano, MD3, Michele McGinnis, MS4, Cadman Leggett, MD4. P2747 - Prevalence of Barrett's Esophagus in Latin American Countries: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
