Monday Poster Session
Category: Esophagus
P2744 - Esophageal Myotomy Is Associated With Reduced Esophageal Cancer and Mortality in Achalasia: A Real-World Cohort Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Fouad Jaber, MD
Baylor College of Medicine
Houston, TX
Presenting Author(s)
Fouad Jaber, MD1, Yazan Sallam, MD2, Mohammad Jaber, MD3, Fares Ayoub, MD1, Tara Keihanian, MD, MPH1, Mai Khalaf, MD1, Mohamed O.. Othman, MD1, Salmaan A.. Jawaid, MD1
1Baylor College of Medicine, Houston, TX; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO; 3Rawalpindi University, Rawalpindi, Islamabad, Pakistan
Introduction: Patients with achalasia have an increased risk of esophageal cancers, such as squamous cell carcinoma. Although peroral endoscopic myotomy (POEM) or Heller’s myotomy can reduce dysphagia symptoms, less is known about their impact on esophageal cancer.
Methods: This retrospective cohort study used the TriNetX database to identify adults (≥18 years) with achalasia. Patients were grouped into: (1) those who underwent myotomy (POEM or Heller) and (2) those who did not. Individuals with prior Barrett’s esophagus, esophagectomy, or esophageal cancer were excluded. The primary outcome was incident esophageal cancer, with subgroup analysis by histologic subtype. Secondary outcome was all-cause mortality. Propensity score matching balanced baseline characteristics. Cox proportional hazards modeling and adjusted odds ratios (aORs) assessed associations, adjusting for demographics, comorbidities, and medication exposures.
Results: A total of 8,106 patients underwent myotomy and 53,874 did not. Median follow-up was 609 days (IQR: 1,746) for the myotomy group and 896 days (IQR: 1,961) for the non-myotomy group. After matching, baseline characteristics were balanced (Table 1). Myotomy was associated with a significantly lower risk of esophageal cancer (before matching: 6 vs. 202, aOR: 0.323; 95% CI: 0.171–0.610; after: 6 vs. 24, aOR: 0.417; 95% CI: 0.199–0.871). Subgroup analysis showed no significant differences in squamous cell carcinoma (before: 4 vs. 37, aOR: 1.769; 95% CI: 0.879–3.559; after: 4 vs. 6, aOR: 1.00; 95% CI: 0.416–2.404) or adenocarcinoma (before: 4 vs. 82, aOR: 0.797; 95% CI: 0.413–1.538; after: 4 vs. 11, aOR: 0.909; 95% CI: 0.386–2.142). Myotomy was also linked to reduced all-cause mortality before (330 vs. 6,496, aHR: 0.235; 95% CI: 0.196–0.281) and after matching (330 vs. 705, aHR: 0.445; 95% CI: 0.389–0.509) (Figure 1-A). Cox regression identified male sex (aHR: 2.64; 95% CI: 1.97–3.53), older age (aHR per year: 1.03; 95% CI: 1.02–1.04), and alcohol use (aHR: 3.10; 95% CI: 1.39–6.90) as independent predictors of esophageal cancer (Figure 1-B). GERD, tobacco, obesity, and PPI use were not significant.
Discussion: In short-term follow-up, myotomy in achalasia was associated with lower risks of esophageal cancer and mortality compared to non-myotomy care. Subgroup analysis by histology showed no significant difference, likely due to low event rates. Prospective studies with longer follow-up are needed to confirm these findings and clarify the oncologic impact of achalasia treatment.
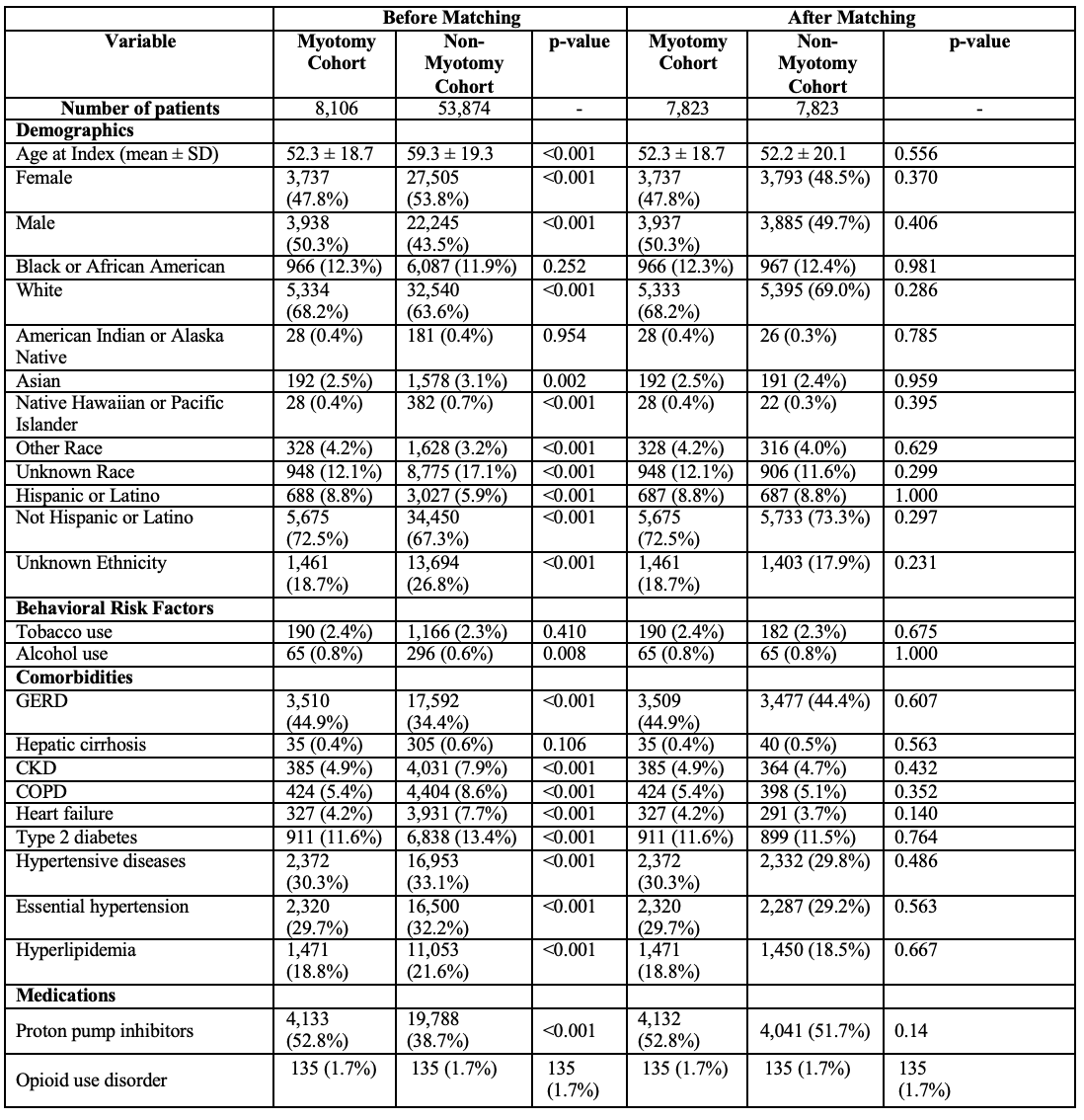
Figure: Table 1: Baseline characteristics of the included cohorts before and after matching
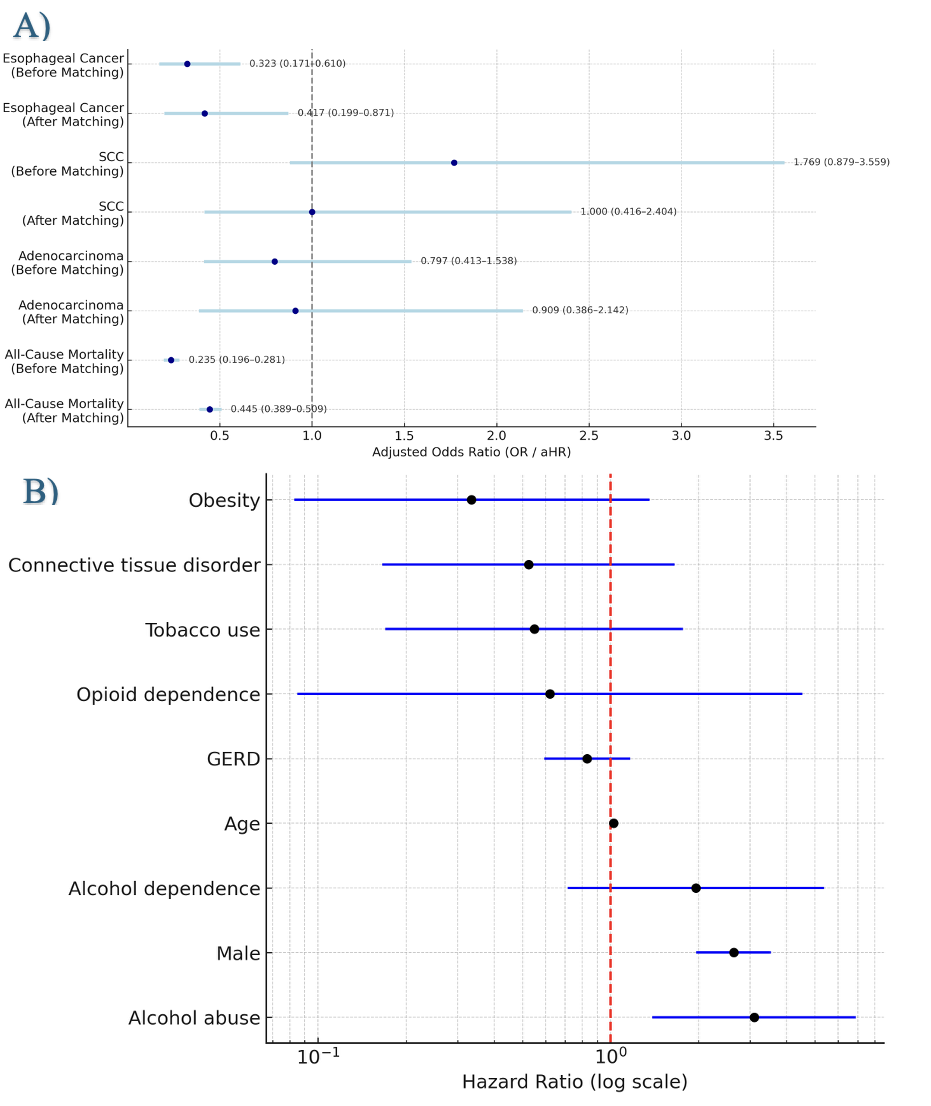
Figure: Figure 1: Forest plot for A) Adjusted Odds ration (aOR) for outcomes of interests between myotomy and non-myotomy cohort. B) cox regression model depicting hazard ratios (HR) and 95% confidence intervals (CI) for predictors of esophageal cancer in achalasia patients after myotomy.
Disclosures:
Fouad Jaber indicated no relevant financial relationships.
Yazan Sallam indicated no relevant financial relationships.
Mohammad Jaber indicated no relevant financial relationships.
Fares Ayoub indicated no relevant financial relationships.
Tara Keihanian: Boston Scientific – Consultant. ConMed – Consultant. Microtech – Consultant.
Mai Khalaf indicated no relevant financial relationships.
Mohamed Othman: Abbvie – Consultant. Boston Scientific – Consultant. ConMed – Consultant. Microtech – Consultant.
Salmaan Jawaid: 3D Matrix – Consultant. Boston Scientific – Consultant. ConMed – Consultant. Creo Medical – Consultant. Microtech – Consultant.
Fouad Jaber, MD1, Yazan Sallam, MD2, Mohammad Jaber, MD3, Fares Ayoub, MD1, Tara Keihanian, MD, MPH1, Mai Khalaf, MD1, Mohamed O.. Othman, MD1, Salmaan A.. Jawaid, MD1. P2744 - Esophageal Myotomy Is Associated With Reduced Esophageal Cancer and Mortality in Achalasia: A Real-World Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Baylor College of Medicine, Houston, TX; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO; 3Rawalpindi University, Rawalpindi, Islamabad, Pakistan
Introduction: Patients with achalasia have an increased risk of esophageal cancers, such as squamous cell carcinoma. Although peroral endoscopic myotomy (POEM) or Heller’s myotomy can reduce dysphagia symptoms, less is known about their impact on esophageal cancer.
Methods: This retrospective cohort study used the TriNetX database to identify adults (≥18 years) with achalasia. Patients were grouped into: (1) those who underwent myotomy (POEM or Heller) and (2) those who did not. Individuals with prior Barrett’s esophagus, esophagectomy, or esophageal cancer were excluded. The primary outcome was incident esophageal cancer, with subgroup analysis by histologic subtype. Secondary outcome was all-cause mortality. Propensity score matching balanced baseline characteristics. Cox proportional hazards modeling and adjusted odds ratios (aORs) assessed associations, adjusting for demographics, comorbidities, and medication exposures.
Results: A total of 8,106 patients underwent myotomy and 53,874 did not. Median follow-up was 609 days (IQR: 1,746) for the myotomy group and 896 days (IQR: 1,961) for the non-myotomy group. After matching, baseline characteristics were balanced (Table 1). Myotomy was associated with a significantly lower risk of esophageal cancer (before matching: 6 vs. 202, aOR: 0.323; 95% CI: 0.171–0.610; after: 6 vs. 24, aOR: 0.417; 95% CI: 0.199–0.871). Subgroup analysis showed no significant differences in squamous cell carcinoma (before: 4 vs. 37, aOR: 1.769; 95% CI: 0.879–3.559; after: 4 vs. 6, aOR: 1.00; 95% CI: 0.416–2.404) or adenocarcinoma (before: 4 vs. 82, aOR: 0.797; 95% CI: 0.413–1.538; after: 4 vs. 11, aOR: 0.909; 95% CI: 0.386–2.142). Myotomy was also linked to reduced all-cause mortality before (330 vs. 6,496, aHR: 0.235; 95% CI: 0.196–0.281) and after matching (330 vs. 705, aHR: 0.445; 95% CI: 0.389–0.509) (Figure 1-A). Cox regression identified male sex (aHR: 2.64; 95% CI: 1.97–3.53), older age (aHR per year: 1.03; 95% CI: 1.02–1.04), and alcohol use (aHR: 3.10; 95% CI: 1.39–6.90) as independent predictors of esophageal cancer (Figure 1-B). GERD, tobacco, obesity, and PPI use were not significant.
Discussion: In short-term follow-up, myotomy in achalasia was associated with lower risks of esophageal cancer and mortality compared to non-myotomy care. Subgroup analysis by histology showed no significant difference, likely due to low event rates. Prospective studies with longer follow-up are needed to confirm these findings and clarify the oncologic impact of achalasia treatment.
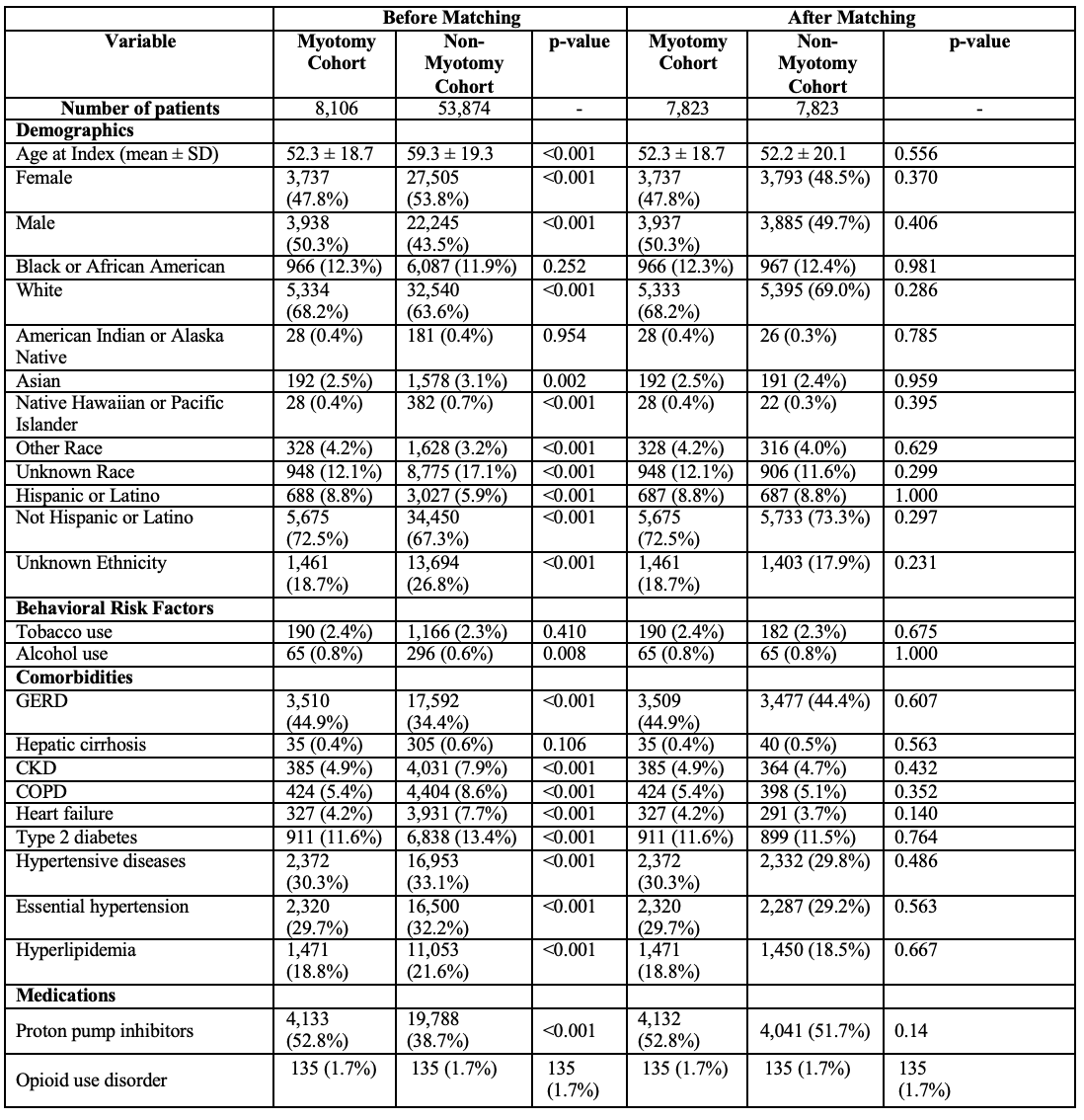
Figure: Table 1: Baseline characteristics of the included cohorts before and after matching
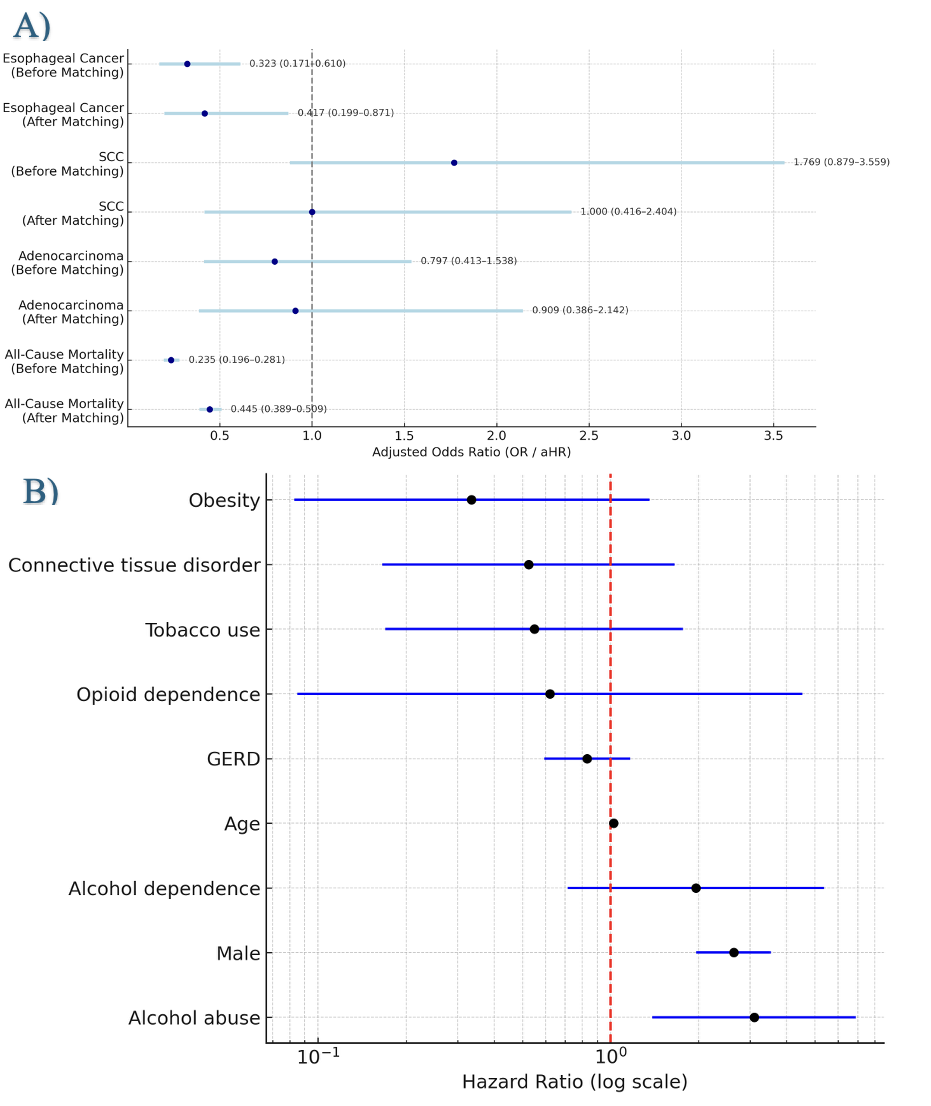
Figure: Figure 1: Forest plot for A) Adjusted Odds ration (aOR) for outcomes of interests between myotomy and non-myotomy cohort. B) cox regression model depicting hazard ratios (HR) and 95% confidence intervals (CI) for predictors of esophageal cancer in achalasia patients after myotomy.
Disclosures:
Fouad Jaber indicated no relevant financial relationships.
Yazan Sallam indicated no relevant financial relationships.
Mohammad Jaber indicated no relevant financial relationships.
Fares Ayoub indicated no relevant financial relationships.
Tara Keihanian: Boston Scientific – Consultant. ConMed – Consultant. Microtech – Consultant.
Mai Khalaf indicated no relevant financial relationships.
Mohamed Othman: Abbvie – Consultant. Boston Scientific – Consultant. ConMed – Consultant. Microtech – Consultant.
Salmaan Jawaid: 3D Matrix – Consultant. Boston Scientific – Consultant. ConMed – Consultant. Creo Medical – Consultant. Microtech – Consultant.
Fouad Jaber, MD1, Yazan Sallam, MD2, Mohammad Jaber, MD3, Fares Ayoub, MD1, Tara Keihanian, MD, MPH1, Mai Khalaf, MD1, Mohamed O.. Othman, MD1, Salmaan A.. Jawaid, MD1. P2744 - Esophageal Myotomy Is Associated With Reduced Esophageal Cancer and Mortality in Achalasia: A Real-World Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

