Monday Poster Session
Category: Esophagus
P2824 - Primary HSV Esophagitis in an Immunocompetent Young Adult: A Diagnostic Challenge
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ahmad Abdulraheem, MD (he/him/his)
MedStar Washington Hospital Center-Georgetown University
Washington, DC
Presenting Author(s)
Mohammad Alzoubi, MD1, Nada Odeh, MD1, Khaled Rafeh, MD2, Mohammad A. Rayyan, 1, Ahmad Abdulraheem, MD3, Khaled Alomari, MD1, Mustafa Ramadan, MD4
1School of Medicine, The University of Jordan, Amman, 'Amman, Jordan; 2School of Medicine, The University of Jordan, Shmeisani, 'Amman, Jordan; 3MedStar Washington Hospital Center-Georgetown University, Washington, DC; 4Istishari Hosptial, Amman, 'Amman, Jordan
Introduction: Esophagitis commonly presents with odynophagia and dysphagia and is often attributed to reflux, infections, or medications. While uncommon, Herpes simplex virus (HSV) esophagitis is among the differential and typically affects immunocompromised patients but can also rarely affect immunocompetent individuals, especially during primary infection. Due to its nonspecific presentation, it may be mistaken for other etiologies. This case highlights HSV esophagitis in a previously healthy, young adult.
Case Description/
Methods: A 24-year-old immunocompetent male presented with a three-day history of high-grade fever and sore throat. On examination, he had purulent tonsillar exudates, and a provisional diagnosis of bacterial tonsillitis was made. He was started on amoxicillin-clavulanate. However, due to lack of improvement, noticeable tonsillar enlargement, and worsening odynophagia, treatment was escalated with clindamycin and dexamethasone.
Over the following days, his symptoms progressed with increased odynophagia and reduced oral intake, prompting a gastroenterology referral. Further history revealed recent labial vesicles and oral ulcers. Notably, his wife had experienced a self-limited episode of herpes labialis shortly before his illness, raising suspicion for a primary HSV infection. HIV testing was negative, with no known immunodeficiency.
Esophagogastroduodenoscopy revealed extensive esophageal ulcerations with white exudates, initially suspicious for Candida esophagitis. Empiric treatment with fluconazole, acyclovir, esomeprazole, and continued clindamycin was initiated. Histopathological examination of esophageal biopsies showed viral cytopathic changes including nuclear molding, multinucleation, and intranuclear inclusions consistent with HSV esophagitis. PAS staining was negative for fungal elements.
After confirmation, only acyclovir (400 mg orally) and esomeprazole (40 mg orally) were continued. The patient’s symptoms resolved completely within two weeks.
Discussion: HSV esophagitis, though rare in immunocompetent individuals, should be considered in cases of persistent odynophagia, especially in the context of recent HSV exposure and mucocutaneous lesions. In our case, recent corticosteroid use may have contributed by transiently impairing local immune defenses, allowing for more severe mucosal involvement during primary infection. Endoscopy and biopsy remain essential for diagnosis, and early antiviral treatment can lead to rapid resolution.
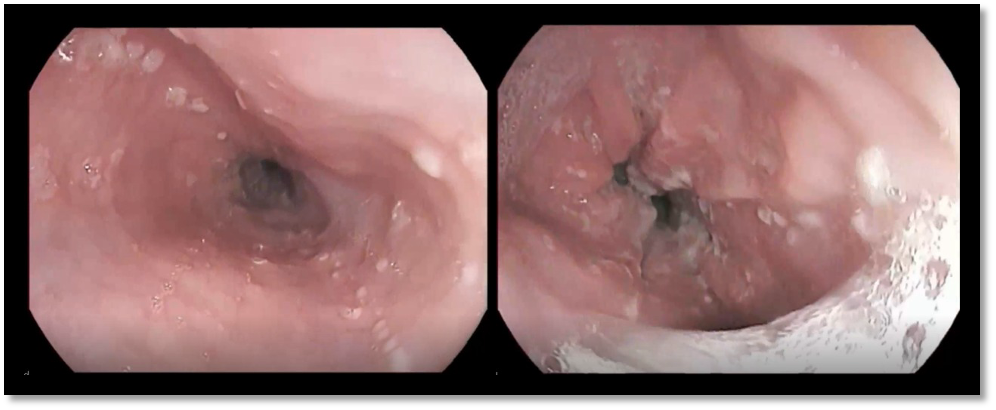
Figure: Figure 1. Endoscopic images showing esophageal ulcerations and exudates indicative of Herpes Simplex Virus (HSV) infection. The left image shows early-stage ulceration with white exudate, while the right image demonstrates more extensive ulcerations and mucosal damage
Disclosures:
Mohammad Alzoubi indicated no relevant financial relationships.
Nada Odeh indicated no relevant financial relationships.
Khaled Rafeh indicated no relevant financial relationships.
Mohammad Rayyan indicated no relevant financial relationships.
Ahmad Abdulraheem indicated no relevant financial relationships.
Khaled Alomari indicated no relevant financial relationships.
Mustafa Ramadan indicated no relevant financial relationships.
Mohammad Alzoubi, MD1, Nada Odeh, MD1, Khaled Rafeh, MD2, Mohammad A. Rayyan, 1, Ahmad Abdulraheem, MD3, Khaled Alomari, MD1, Mustafa Ramadan, MD4. P2824 - Primary HSV Esophagitis in an Immunocompetent Young Adult: A Diagnostic Challenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1School of Medicine, The University of Jordan, Amman, 'Amman, Jordan; 2School of Medicine, The University of Jordan, Shmeisani, 'Amman, Jordan; 3MedStar Washington Hospital Center-Georgetown University, Washington, DC; 4Istishari Hosptial, Amman, 'Amman, Jordan
Introduction: Esophagitis commonly presents with odynophagia and dysphagia and is often attributed to reflux, infections, or medications. While uncommon, Herpes simplex virus (HSV) esophagitis is among the differential and typically affects immunocompromised patients but can also rarely affect immunocompetent individuals, especially during primary infection. Due to its nonspecific presentation, it may be mistaken for other etiologies. This case highlights HSV esophagitis in a previously healthy, young adult.
Case Description/
Methods: A 24-year-old immunocompetent male presented with a three-day history of high-grade fever and sore throat. On examination, he had purulent tonsillar exudates, and a provisional diagnosis of bacterial tonsillitis was made. He was started on amoxicillin-clavulanate. However, due to lack of improvement, noticeable tonsillar enlargement, and worsening odynophagia, treatment was escalated with clindamycin and dexamethasone.
Over the following days, his symptoms progressed with increased odynophagia and reduced oral intake, prompting a gastroenterology referral. Further history revealed recent labial vesicles and oral ulcers. Notably, his wife had experienced a self-limited episode of herpes labialis shortly before his illness, raising suspicion for a primary HSV infection. HIV testing was negative, with no known immunodeficiency.
Esophagogastroduodenoscopy revealed extensive esophageal ulcerations with white exudates, initially suspicious for Candida esophagitis. Empiric treatment with fluconazole, acyclovir, esomeprazole, and continued clindamycin was initiated. Histopathological examination of esophageal biopsies showed viral cytopathic changes including nuclear molding, multinucleation, and intranuclear inclusions consistent with HSV esophagitis. PAS staining was negative for fungal elements.
After confirmation, only acyclovir (400 mg orally) and esomeprazole (40 mg orally) were continued. The patient’s symptoms resolved completely within two weeks.
Discussion: HSV esophagitis, though rare in immunocompetent individuals, should be considered in cases of persistent odynophagia, especially in the context of recent HSV exposure and mucocutaneous lesions. In our case, recent corticosteroid use may have contributed by transiently impairing local immune defenses, allowing for more severe mucosal involvement during primary infection. Endoscopy and biopsy remain essential for diagnosis, and early antiviral treatment can lead to rapid resolution.
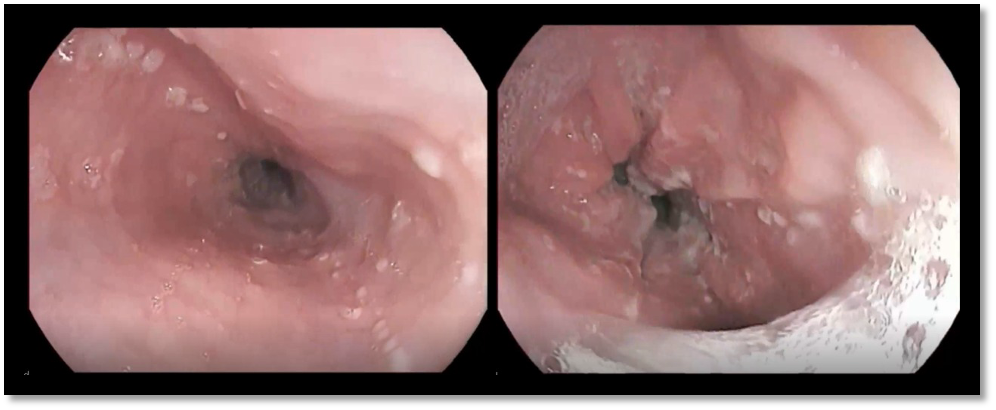
Figure: Figure 1. Endoscopic images showing esophageal ulcerations and exudates indicative of Herpes Simplex Virus (HSV) infection. The left image shows early-stage ulceration with white exudate, while the right image demonstrates more extensive ulcerations and mucosal damage
Disclosures:
Mohammad Alzoubi indicated no relevant financial relationships.
Nada Odeh indicated no relevant financial relationships.
Khaled Rafeh indicated no relevant financial relationships.
Mohammad Rayyan indicated no relevant financial relationships.
Ahmad Abdulraheem indicated no relevant financial relationships.
Khaled Alomari indicated no relevant financial relationships.
Mustafa Ramadan indicated no relevant financial relationships.
Mohammad Alzoubi, MD1, Nada Odeh, MD1, Khaled Rafeh, MD2, Mohammad A. Rayyan, 1, Ahmad Abdulraheem, MD3, Khaled Alomari, MD1, Mustafa Ramadan, MD4. P2824 - Primary HSV Esophagitis in an Immunocompetent Young Adult: A Diagnostic Challenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
