Monday Poster Session
Category: Esophagus
P2819 - Eosinophilic Gastrointestinal Disorders and Marked Leukocytosis in Alpha-Gal Syndrome: Infection, Allergy, or Hematologic Malignancy?
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Frhaan Zahrawi, MBBCh (he/him/his)
Franciscan Health Olympia Fields
Olympia Fields, IL
Presenting Author(s)
Frhaan Zahrawi, MBBCh1, Mohamed Alharami, MD2, Omar Alwan, MD3, Ziad Suleiman, MD4, Hadi Hemaidan, MS5
1Franciscan Health Olympia Fields, Olympia Fields, IL; 2Henry Ford Warren, Warren, MI; 3Hamilton Medical Center, Dalton, GA; 4Southwest healthcare medical education consortium, Murrieta, CA; 5Florida International University, Daytona Beach, FL
Introduction: Alpha-gal syndrome (AGS) is a tick-borne, delayed hypersensitivity reaction to galactose-α-1,3-galactose, manifesting as urticaria, anaphylaxis, or gastrointestinal symptoms following the consumption of mammalian meat products. While eosinophilia can occur in allergic conditions, the literature contains no reports of patients with AGS concurrently developing eosinophilic gastrointestinal disorders (EGIDs). We present a rare case of AGS manifesting with eosinophilic gastrointestinal symptoms and bone marrow findings consistent with eosinophilic proliferation and myeloid atypia.
Case Description/
Methods: A 63-year-old male with a history of AGS presented with dysphagia, dyspnea, and a generalized pustular rash a few days after consuming a hamburger (Figure 1). After a recent visit to the urgent care unit, cefepime was started for fever and mild leukocytosis. Upon hospital admission, imaging revealed bilateral pulmonary infiltrates, and laboratory tests showed marked leukocytosis exceeding 100,000/µL and an eosinophil count above 42,000/µL. Upper endoscopy revealed severe mucosal inflammation of the esophagus and stomach with dense eosinophilic infiltrates, consistent with eosinophilic esophagitis (EoE) and eosinophilic gastritis (EG). A skin biopsy also showed eosinophilic infiltration.The initial differential diagnosis included eosinophilic pneumonia, drug-induced eosinophilia (cefepime), leukemoid reaction, and primary eosinophilic disorders such as hypereosinophilic syndrome (HES) or chronic eosinophilic leukemia. The patient was started on empiric antibiotics and high-dose corticosteroids. Due to worsening leukocytosis, a bone marrow biopsy was performed, revealing hypercellularity with myeloid predominance and increased eosinophils and eosinophilic precursors. Molecular and cytogenetic studies were negative for PDGFRA, PDGFRB, FGFR1, JAK2, BCR-ABL1, and CBFB rearrangements, leading to a diagnosis of idiopathic HES.
Discussion: A potential link between AGS and EGIDs is highlighted through this case. While AGS is typically considered a food allergy, it may act as a trigger for eosinophilic infiltration of the gastrointestinal tract, as seen in this patient with findings consistent with EoE and EG. More studies are needed to clarify the relationship between AGS and primary eosinophilic disorders and to explore whether AGS may unmask or exacerbate underlying eosinophilic gastrointestinal pathology.
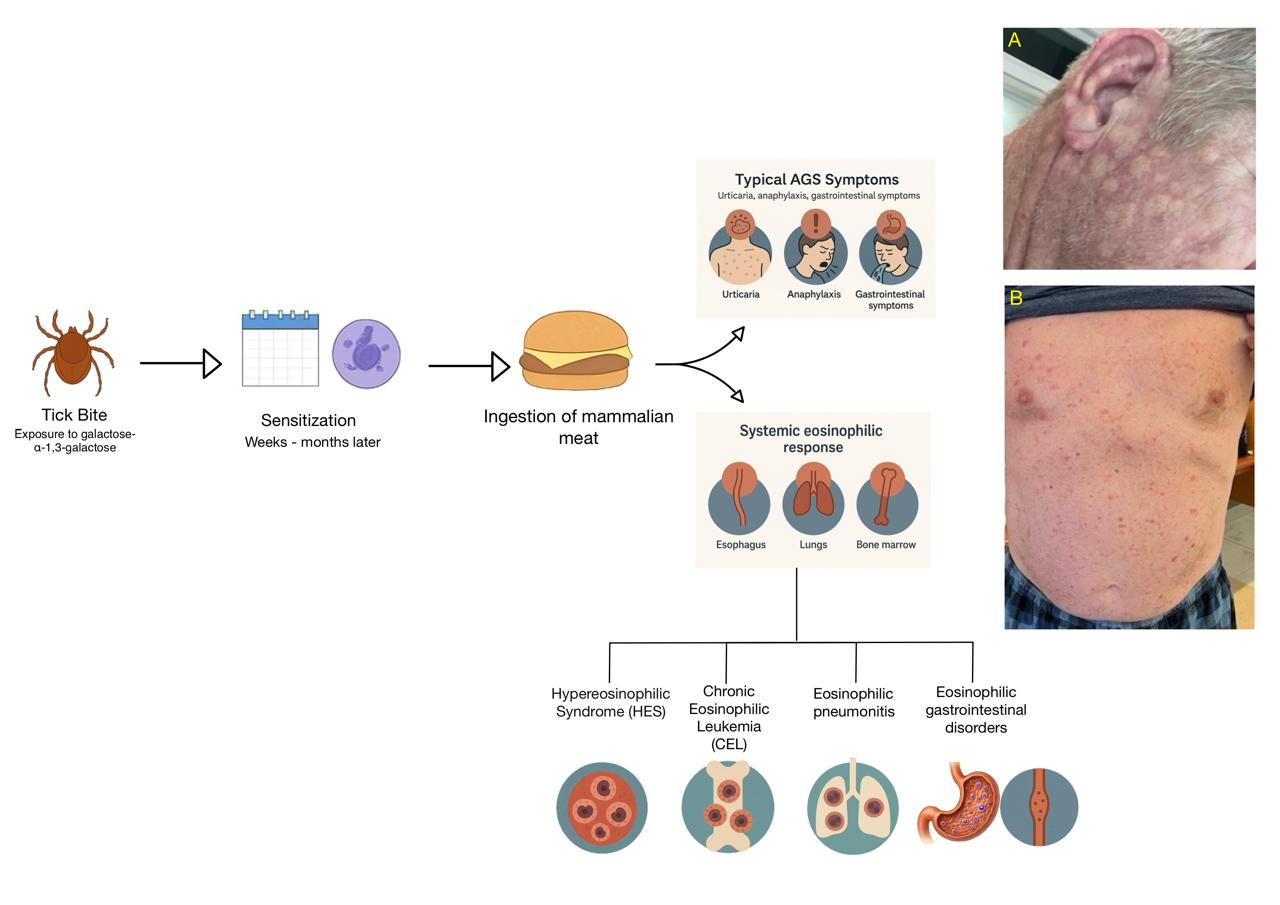
Figure: Overview of the case, illustrating alpha-gal syndrome (AGS) pathogenesis and its potential to trigger systemic eosinophilic responses, including gastrointestinal involvement. Images A and B show the patient’s eosinophilic rash at presentation.
Disclosures:
Frhaan Zahrawi indicated no relevant financial relationships.
Mohamed Alharami indicated no relevant financial relationships.
Omar Alwan indicated no relevant financial relationships.
Ziad Suleiman indicated no relevant financial relationships.
Hadi Hemaidan indicated no relevant financial relationships.
Frhaan Zahrawi, MBBCh1, Mohamed Alharami, MD2, Omar Alwan, MD3, Ziad Suleiman, MD4, Hadi Hemaidan, MS5. P2819 - Eosinophilic Gastrointestinal Disorders and Marked Leukocytosis in Alpha-Gal Syndrome: Infection, Allergy, or Hematologic Malignancy?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Franciscan Health Olympia Fields, Olympia Fields, IL; 2Henry Ford Warren, Warren, MI; 3Hamilton Medical Center, Dalton, GA; 4Southwest healthcare medical education consortium, Murrieta, CA; 5Florida International University, Daytona Beach, FL
Introduction: Alpha-gal syndrome (AGS) is a tick-borne, delayed hypersensitivity reaction to galactose-α-1,3-galactose, manifesting as urticaria, anaphylaxis, or gastrointestinal symptoms following the consumption of mammalian meat products. While eosinophilia can occur in allergic conditions, the literature contains no reports of patients with AGS concurrently developing eosinophilic gastrointestinal disorders (EGIDs). We present a rare case of AGS manifesting with eosinophilic gastrointestinal symptoms and bone marrow findings consistent with eosinophilic proliferation and myeloid atypia.
Case Description/
Methods: A 63-year-old male with a history of AGS presented with dysphagia, dyspnea, and a generalized pustular rash a few days after consuming a hamburger (Figure 1). After a recent visit to the urgent care unit, cefepime was started for fever and mild leukocytosis. Upon hospital admission, imaging revealed bilateral pulmonary infiltrates, and laboratory tests showed marked leukocytosis exceeding 100,000/µL and an eosinophil count above 42,000/µL. Upper endoscopy revealed severe mucosal inflammation of the esophagus and stomach with dense eosinophilic infiltrates, consistent with eosinophilic esophagitis (EoE) and eosinophilic gastritis (EG). A skin biopsy also showed eosinophilic infiltration.The initial differential diagnosis included eosinophilic pneumonia, drug-induced eosinophilia (cefepime), leukemoid reaction, and primary eosinophilic disorders such as hypereosinophilic syndrome (HES) or chronic eosinophilic leukemia. The patient was started on empiric antibiotics and high-dose corticosteroids. Due to worsening leukocytosis, a bone marrow biopsy was performed, revealing hypercellularity with myeloid predominance and increased eosinophils and eosinophilic precursors. Molecular and cytogenetic studies were negative for PDGFRA, PDGFRB, FGFR1, JAK2, BCR-ABL1, and CBFB rearrangements, leading to a diagnosis of idiopathic HES.
Discussion: A potential link between AGS and EGIDs is highlighted through this case. While AGS is typically considered a food allergy, it may act as a trigger for eosinophilic infiltration of the gastrointestinal tract, as seen in this patient with findings consistent with EoE and EG. More studies are needed to clarify the relationship between AGS and primary eosinophilic disorders and to explore whether AGS may unmask or exacerbate underlying eosinophilic gastrointestinal pathology.
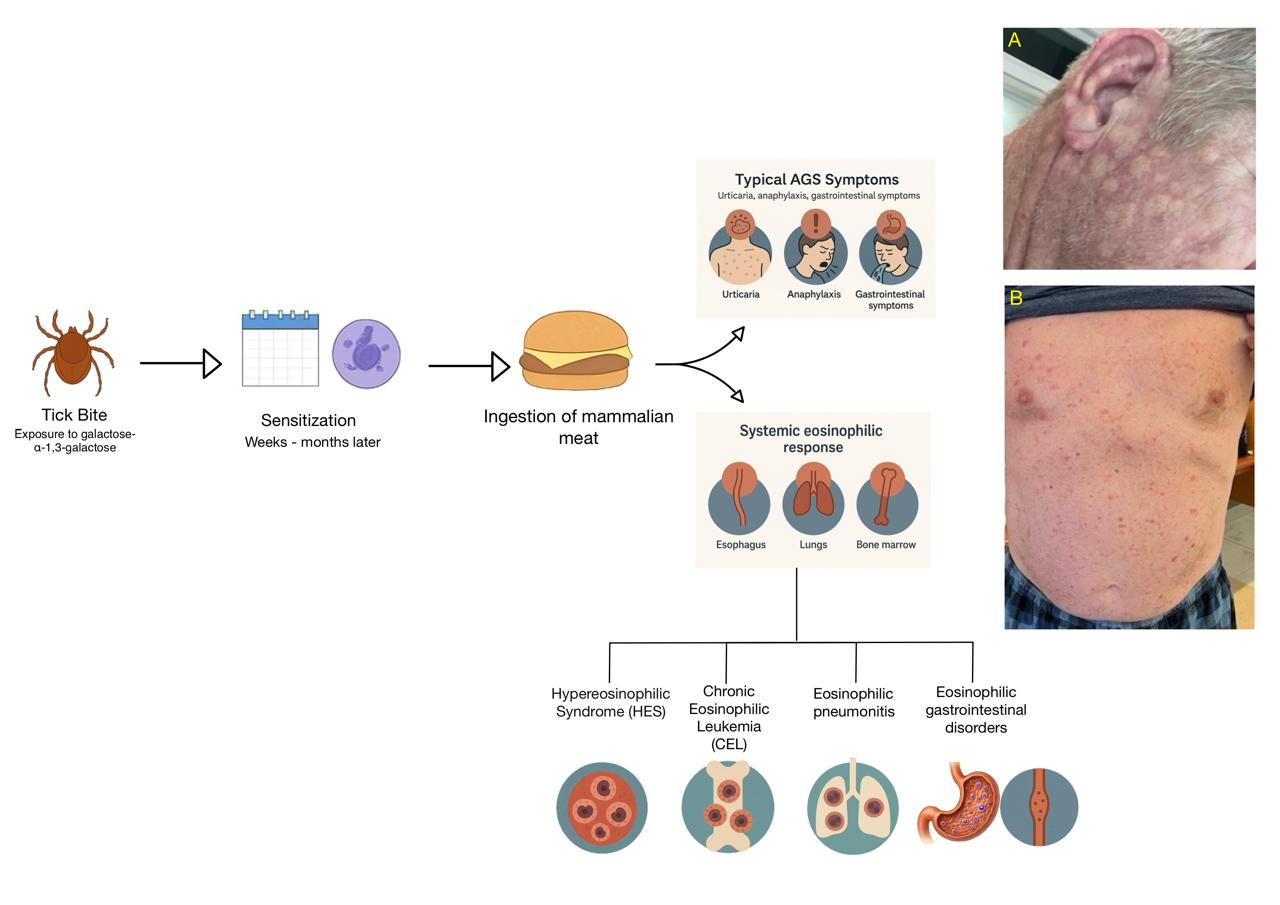
Figure: Overview of the case, illustrating alpha-gal syndrome (AGS) pathogenesis and its potential to trigger systemic eosinophilic responses, including gastrointestinal involvement. Images A and B show the patient’s eosinophilic rash at presentation.
Disclosures:
Frhaan Zahrawi indicated no relevant financial relationships.
Mohamed Alharami indicated no relevant financial relationships.
Omar Alwan indicated no relevant financial relationships.
Ziad Suleiman indicated no relevant financial relationships.
Hadi Hemaidan indicated no relevant financial relationships.
Frhaan Zahrawi, MBBCh1, Mohamed Alharami, MD2, Omar Alwan, MD3, Ziad Suleiman, MD4, Hadi Hemaidan, MS5. P2819 - Eosinophilic Gastrointestinal Disorders and Marked Leukocytosis in Alpha-Gal Syndrome: Infection, Allergy, or Hematologic Malignancy?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
