Monday Poster Session
Category: General Endoscopy
P2986 - Impact of Endoscopist Characteristics on Recurrence After Endoscopic Large Colonic Polyp Resection
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Kaitlin R. McGowan, DO (she/her/hers)
Dartmouth Hitchcock Medical Center
Lebanon, NH
Presenting Author(s)
Kaitlin R. McGowan, DO1, Daniel von Renteln, MD2, Douglas Rex, MD3, Jeremy Barber, MD4, Matt Moyer, MD5, B. Joseph Elmunzer, MD6, John Levenick, MD7, Stuart R. Gordon, MD1, Harry Aslanian, MD8, Mazen Elatrache, MD9, Michael B. Wallace, MD10, Rajesh Keswani, MD11, Nikhil Kumta, MD12, Douglas Pleskow, MD13, Cyrus Piraka, MD9, Robert Pompa, MD9, Eugene Zolotarevsky, MD4, Amit Rastogi, MD14, Heiko Pohl, MD1
1Dartmouth Hitchcock Medical Center, Lebanon, NH; 2Centre Hospitalier de L’Universite de Montreal, Montreal, PQ, Canada; 3Indiana University School of Medicine, Indianapolis, IN; 4Spectrum Health Butterworth Hospital, Grand Rapids, MI; 5Penn State Health Milton S Hershey Medical Center, Hershey, PA; 6Medical University of South Carolina, Charleston, SC; 7Penn State College of Medicine, Hershey, PA; 8Yale New Haven Health System, New Haven, CT; 9Henry Ford Health, Detroit, MI; 10Mayo Clinic, Jacksonville, FL; 11Northwestern University, Chicago, IL; 12New York University, New York, NY; 13Beth Israel Deaconess Medical Center, Boston, MA; 14The University of Kansas Health System, Shawnee, KS
Introduction: Although endoscopist experience and skill are believed to be critical to ensuring complete endoscopic mucosal resection (EMR) of large colorectal polyps, very little is known about variation between endoscopists and its effect on completeness of resection. We aimed to examine the association between individual endoscopist characteristics and recurrence after cold and hot EMR.
Methods: We used data of a recent randomized trial comparing cold with hot EMR of ≥20 mm non-pedunculated colorectal polyps. Participating endoscopists completed a survey prior to study commencement. Our primary outcome measure was the endoscopists’ variation in the rate of residual or recurrent neoplastic polyps (termed “recurrence”) at first surveillance colonoscopy. Secondary outcomes included association of endoscopist characteristics with recurrence. Multivariable analysis was applied to adjust for polyp complexity (size, location, advanced histology).
Results: Among 660 patients 714 large polyps were removed by 29 endoscopists. Corresponding survey data were available for 680 EMRs (95.2%). Recurrence varied broadly from 12.7 to 45.8% for any EMR (p= 0.002), 0 and 50.0% for hot EMR (p< 0.001), and 11.9 and 46.7% for cold EMR (p=0.129) (Figure 1). There was no correlation between hot and cold EMR. In univariable analysis (Table 1), endoscopists with longer resection times, fewer study EMRs, and prior advanced endoscopy training had a greater risk of recurrence. After adjusting for polyp complexity, the risk of recurrence increased for endoscopists with longer resection times following any EMR (OR 1.02 per minute increment, 95%CI [CI] 1.01-1.03), hot EMR (OR 1.02, CI 1.01-1.04) and cold EMR (OR 1.02, CI 1.00-1.03). The risk for recurrence following cold EMR was lower for endoscopists with a greater number of lifetime cold EMR procedures (OR 0.999 per one EMR increment, OR 0.999-1.000, p=0.016). Years since training, lifetime number of colonoscopies, or annual EMR volume were not associated with recurrence.
Discussion: This first formal analysis of endoscopist characteristics and recurrence after large polyp EMR showed a broad variation between endoscopists, while poor outcomes after hot and cold EMR were not correlated. Although most endoscopist characteristics were not associated with recurrence, a greater recurrence with longer resection times suggests that sufficient experience is required to ensure low recurrence rates, particularly for cold EMR.
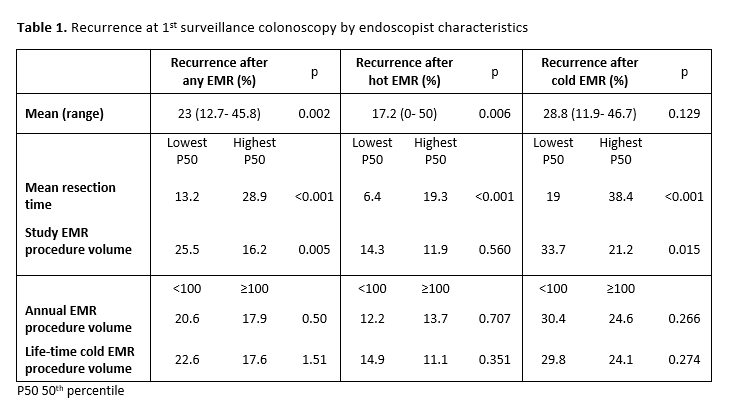
Figure: Table 1. Recurrence at 1st surveillance colonoscopy by endoscopist characteristics.
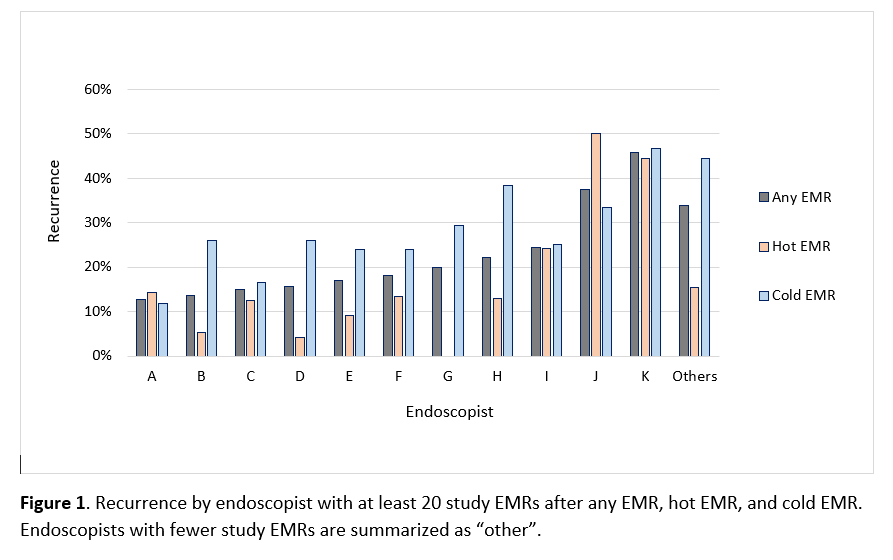
Figure: Figure 1. Recurrence by endoscopist.
Disclosures:
Kaitlin McGowan indicated no relevant financial relationships.
Daniel von Renteln indicated no relevant financial relationships.
Douglas Rex indicated no relevant financial relationships.
Jeremy Barber indicated no relevant financial relationships.
Matt Moyer indicated no relevant financial relationships.
B. Joseph Elmunzer indicated no relevant financial relationships.
John Levenick indicated no relevant financial relationships.
Stuart Gordon: Boston Scientific – Consultant.
Harry Aslanian indicated no relevant financial relationships.
Mazen Elatrache indicated no relevant financial relationships.
Michael Wallace indicated no relevant financial relationships.
Rajesh Keswani indicated no relevant financial relationships.
Nikhil Kumta indicated no relevant financial relationships.
Douglas Pleskow indicated no relevant financial relationships.
Cyrus Piraka indicated no relevant financial relationships.
Robert Pompa indicated no relevant financial relationships.
Eugene Zolotarevsky indicated no relevant financial relationships.
Amit Rastogi indicated no relevant financial relationships.
Heiko Pohl indicated no relevant financial relationships.
Kaitlin R. McGowan, DO1, Daniel von Renteln, MD2, Douglas Rex, MD3, Jeremy Barber, MD4, Matt Moyer, MD5, B. Joseph Elmunzer, MD6, John Levenick, MD7, Stuart R. Gordon, MD1, Harry Aslanian, MD8, Mazen Elatrache, MD9, Michael B. Wallace, MD10, Rajesh Keswani, MD11, Nikhil Kumta, MD12, Douglas Pleskow, MD13, Cyrus Piraka, MD9, Robert Pompa, MD9, Eugene Zolotarevsky, MD4, Amit Rastogi, MD14, Heiko Pohl, MD1. P2986 - Impact of Endoscopist Characteristics on Recurrence After Endoscopic Large Colonic Polyp Resection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Dartmouth Hitchcock Medical Center, Lebanon, NH; 2Centre Hospitalier de L’Universite de Montreal, Montreal, PQ, Canada; 3Indiana University School of Medicine, Indianapolis, IN; 4Spectrum Health Butterworth Hospital, Grand Rapids, MI; 5Penn State Health Milton S Hershey Medical Center, Hershey, PA; 6Medical University of South Carolina, Charleston, SC; 7Penn State College of Medicine, Hershey, PA; 8Yale New Haven Health System, New Haven, CT; 9Henry Ford Health, Detroit, MI; 10Mayo Clinic, Jacksonville, FL; 11Northwestern University, Chicago, IL; 12New York University, New York, NY; 13Beth Israel Deaconess Medical Center, Boston, MA; 14The University of Kansas Health System, Shawnee, KS
Introduction: Although endoscopist experience and skill are believed to be critical to ensuring complete endoscopic mucosal resection (EMR) of large colorectal polyps, very little is known about variation between endoscopists and its effect on completeness of resection. We aimed to examine the association between individual endoscopist characteristics and recurrence after cold and hot EMR.
Methods: We used data of a recent randomized trial comparing cold with hot EMR of ≥20 mm non-pedunculated colorectal polyps. Participating endoscopists completed a survey prior to study commencement. Our primary outcome measure was the endoscopists’ variation in the rate of residual or recurrent neoplastic polyps (termed “recurrence”) at first surveillance colonoscopy. Secondary outcomes included association of endoscopist characteristics with recurrence. Multivariable analysis was applied to adjust for polyp complexity (size, location, advanced histology).
Results: Among 660 patients 714 large polyps were removed by 29 endoscopists. Corresponding survey data were available for 680 EMRs (95.2%). Recurrence varied broadly from 12.7 to 45.8% for any EMR (p= 0.002), 0 and 50.0% for hot EMR (p< 0.001), and 11.9 and 46.7% for cold EMR (p=0.129) (Figure 1). There was no correlation between hot and cold EMR. In univariable analysis (Table 1), endoscopists with longer resection times, fewer study EMRs, and prior advanced endoscopy training had a greater risk of recurrence. After adjusting for polyp complexity, the risk of recurrence increased for endoscopists with longer resection times following any EMR (OR 1.02 per minute increment, 95%CI [CI] 1.01-1.03), hot EMR (OR 1.02, CI 1.01-1.04) and cold EMR (OR 1.02, CI 1.00-1.03). The risk for recurrence following cold EMR was lower for endoscopists with a greater number of lifetime cold EMR procedures (OR 0.999 per one EMR increment, OR 0.999-1.000, p=0.016). Years since training, lifetime number of colonoscopies, or annual EMR volume were not associated with recurrence.
Discussion: This first formal analysis of endoscopist characteristics and recurrence after large polyp EMR showed a broad variation between endoscopists, while poor outcomes after hot and cold EMR were not correlated. Although most endoscopist characteristics were not associated with recurrence, a greater recurrence with longer resection times suggests that sufficient experience is required to ensure low recurrence rates, particularly for cold EMR.
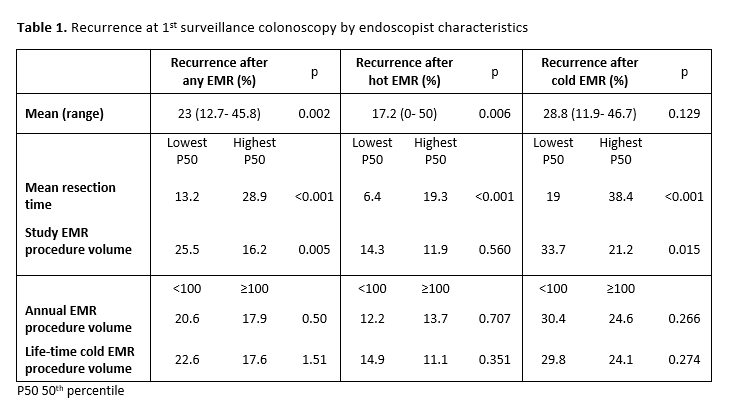
Figure: Table 1. Recurrence at 1st surveillance colonoscopy by endoscopist characteristics.
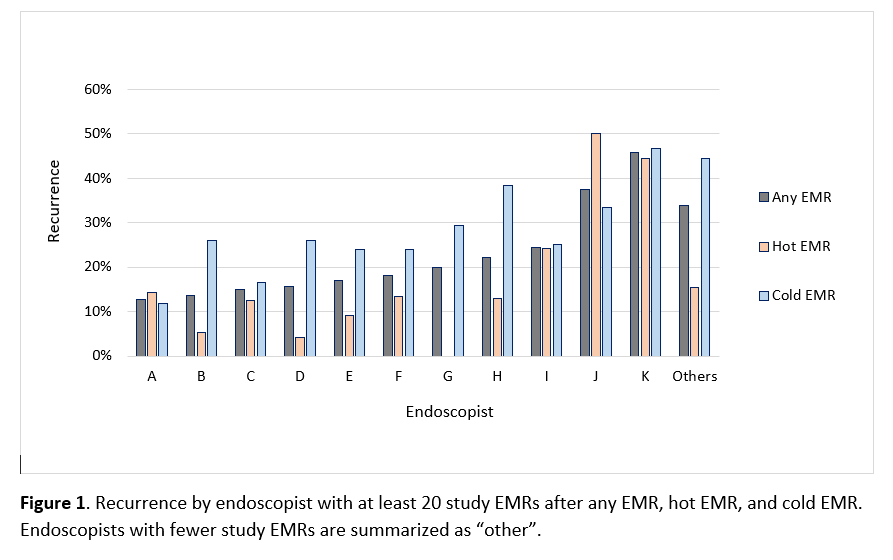
Figure: Figure 1. Recurrence by endoscopist.
Disclosures:
Kaitlin McGowan indicated no relevant financial relationships.
Daniel von Renteln indicated no relevant financial relationships.
Douglas Rex indicated no relevant financial relationships.
Jeremy Barber indicated no relevant financial relationships.
Matt Moyer indicated no relevant financial relationships.
B. Joseph Elmunzer indicated no relevant financial relationships.
John Levenick indicated no relevant financial relationships.
Stuart Gordon: Boston Scientific – Consultant.
Harry Aslanian indicated no relevant financial relationships.
Mazen Elatrache indicated no relevant financial relationships.
Michael Wallace indicated no relevant financial relationships.
Rajesh Keswani indicated no relevant financial relationships.
Nikhil Kumta indicated no relevant financial relationships.
Douglas Pleskow indicated no relevant financial relationships.
Cyrus Piraka indicated no relevant financial relationships.
Robert Pompa indicated no relevant financial relationships.
Eugene Zolotarevsky indicated no relevant financial relationships.
Amit Rastogi indicated no relevant financial relationships.
Heiko Pohl indicated no relevant financial relationships.
Kaitlin R. McGowan, DO1, Daniel von Renteln, MD2, Douglas Rex, MD3, Jeremy Barber, MD4, Matt Moyer, MD5, B. Joseph Elmunzer, MD6, John Levenick, MD7, Stuart R. Gordon, MD1, Harry Aslanian, MD8, Mazen Elatrache, MD9, Michael B. Wallace, MD10, Rajesh Keswani, MD11, Nikhil Kumta, MD12, Douglas Pleskow, MD13, Cyrus Piraka, MD9, Robert Pompa, MD9, Eugene Zolotarevsky, MD4, Amit Rastogi, MD14, Heiko Pohl, MD1. P2986 - Impact of Endoscopist Characteristics on Recurrence After Endoscopic Large Colonic Polyp Resection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
