Monday Poster Session
Category: GI Bleeding
P3065 - A Nationwide Cross-Sectional Study of Gastrointestinal Outcomes in Systemic Sclerosis: A National Inpatient Sample (2016–2022)
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sreekant Avula, MBBS
Hennepin Healthcare
Eden Prairie, MN
Presenting Author(s)
Sreekant Avula, MBBS1, Vinay Thallapally, MBBS2, Khalid Ahmed, MD3, Mahesh Cheryala, MD4
1Hennepin Healthcare, Eden Prairie, MN; 2HealthPartners, Regions Hospital, Minneapolis, MN; 3University of Minnesota, Minneapolis, MN; 4Riverside Regional Medical center, Newport News, VA
Introduction: Systemic sclerosis(SSC) is a chronic autoimmune disease that can affect any part of gastrointestinal (GI system. After the skin, gastrointestinal (GI) involvement is the most often occurring internal organ manifestation in over 80% of patients. From the esophagus to the rectum, it can affect any section of the GI tract and cause dysphagia, reflux, gastroparesis, pseudo-obstruction, diarrhea, and fecal incontinence. These symptoms are a main cause of death in SSc patients and greatly add to morbidity. GI involvement in SSc is sometimes underdiagnosed and undertreated despite its great frequency, which emphasizes the need of more population-level research to grasp its burden and consequences.
Methods: Our study examined records from the Nationwide Inpatient Sample Database (NIS) covering the seven-year period from January 1, 2016, to December 31, 2022. We included patients aged 18 and above who were hospitalized primarily for Systemic Sclerosis (SSC). Patients with SSC were identified and compared to non-SSC admissions. Demographic variables included age, sex, length of stay, and total hospital charges. Comorbidities were identified using ICD-10-CM codes for diabetes mellitus, hypertension, hyperlipidemia, obesity and tobacco use. Primary outcomes were the prevalence of pancreatitis, mesenteric vasculitis, gastrointestinal perforation, gastrointestinal bleeding, and in-hospital mortality. Multivariate logistic regression models adjusted for age, sex, diabetes, hypertension, hyperlipidemia, obesity, and smoking status. Results are presented as adjusted ORs with 95% CIs and p-values.
Results: Of the 241 million weighted hospitalizations, 214,770 (0.09%) had SSC. SSC patients were older (mean age 63.1 vs 49.8 years) and more likely female (84.2% vs 55.8%). Compared to non-SSC patients, SSC patients had longer hospital stays (6.3 vs. 4.8 days) and higher total charges ($80,904 vs. $57,589). After adjustment, SSC was associated with increased odds of mesenteric vasculitis (aOR 2.89, 95% CI 2.69–3.11), GI bleeding (aOR 2.09, 95% CI 2.03–2.16), and in-hospital mortality (aOR 1.85, 95% CI 1.77–1.94). Conversely, SSC was associated with lower odds of pancreatitis (aOR 0.85, 95% CI 0.77–0.94) and GI perforation (aOR 0.69, 95% CI 0.48–1.00).
Discussion: Hospitalized patients with systemic sclerosis experience significantly higher risks of mesenteric vasculitis, GI bleeding, and mortality. These findings highlight the need for vigilant GI monitoring and risk mitigation in SSC hospital care.
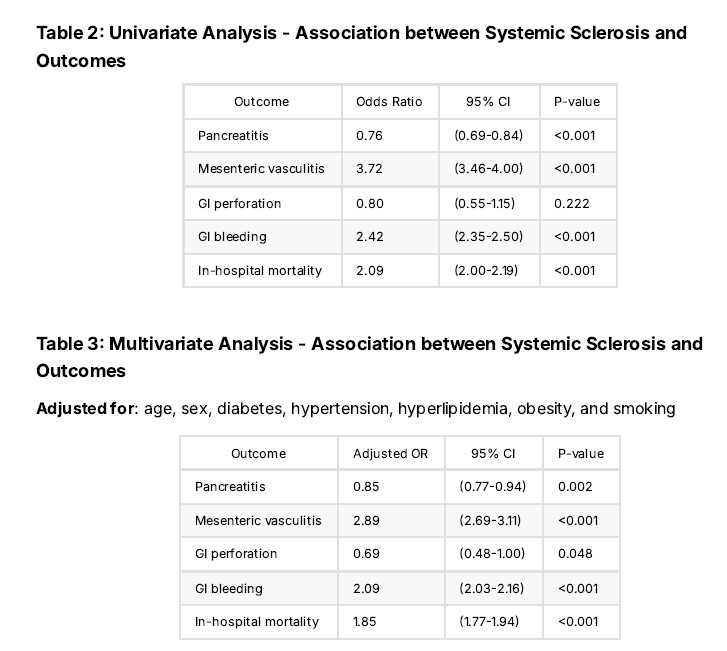
Figure: Demographics and Clinical Characteristics
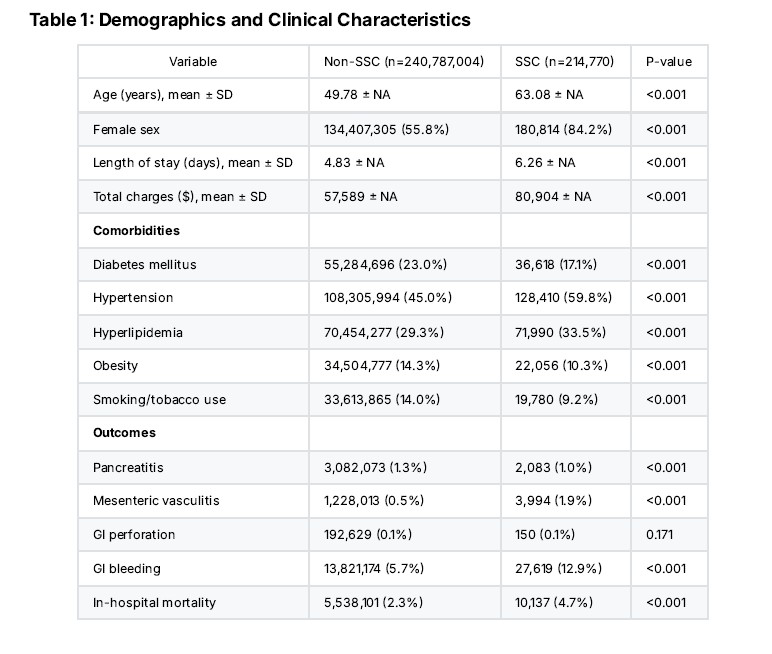
Figure: Univariate & Multivariate Analysis - Association between Systemic Sclerosis and Outcomes
Disclosures:
Sreekant Avula indicated no relevant financial relationships.
Vinay Thallapally indicated no relevant financial relationships.
Khalid Ahmed indicated no relevant financial relationships.
Mahesh Cheryala indicated no relevant financial relationships.
Sreekant Avula, MBBS1, Vinay Thallapally, MBBS2, Khalid Ahmed, MD3, Mahesh Cheryala, MD4. P3065 - A Nationwide Cross-Sectional Study of Gastrointestinal Outcomes in Systemic Sclerosis: A National Inpatient Sample (2016–2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Hennepin Healthcare, Eden Prairie, MN; 2HealthPartners, Regions Hospital, Minneapolis, MN; 3University of Minnesota, Minneapolis, MN; 4Riverside Regional Medical center, Newport News, VA
Introduction: Systemic sclerosis(SSC) is a chronic autoimmune disease that can affect any part of gastrointestinal (GI system. After the skin, gastrointestinal (GI) involvement is the most often occurring internal organ manifestation in over 80% of patients. From the esophagus to the rectum, it can affect any section of the GI tract and cause dysphagia, reflux, gastroparesis, pseudo-obstruction, diarrhea, and fecal incontinence. These symptoms are a main cause of death in SSc patients and greatly add to morbidity. GI involvement in SSc is sometimes underdiagnosed and undertreated despite its great frequency, which emphasizes the need of more population-level research to grasp its burden and consequences.
Methods: Our study examined records from the Nationwide Inpatient Sample Database (NIS) covering the seven-year period from January 1, 2016, to December 31, 2022. We included patients aged 18 and above who were hospitalized primarily for Systemic Sclerosis (SSC). Patients with SSC were identified and compared to non-SSC admissions. Demographic variables included age, sex, length of stay, and total hospital charges. Comorbidities were identified using ICD-10-CM codes for diabetes mellitus, hypertension, hyperlipidemia, obesity and tobacco use. Primary outcomes were the prevalence of pancreatitis, mesenteric vasculitis, gastrointestinal perforation, gastrointestinal bleeding, and in-hospital mortality. Multivariate logistic regression models adjusted for age, sex, diabetes, hypertension, hyperlipidemia, obesity, and smoking status. Results are presented as adjusted ORs with 95% CIs and p-values.
Results: Of the 241 million weighted hospitalizations, 214,770 (0.09%) had SSC. SSC patients were older (mean age 63.1 vs 49.8 years) and more likely female (84.2% vs 55.8%). Compared to non-SSC patients, SSC patients had longer hospital stays (6.3 vs. 4.8 days) and higher total charges ($80,904 vs. $57,589). After adjustment, SSC was associated with increased odds of mesenteric vasculitis (aOR 2.89, 95% CI 2.69–3.11), GI bleeding (aOR 2.09, 95% CI 2.03–2.16), and in-hospital mortality (aOR 1.85, 95% CI 1.77–1.94). Conversely, SSC was associated with lower odds of pancreatitis (aOR 0.85, 95% CI 0.77–0.94) and GI perforation (aOR 0.69, 95% CI 0.48–1.00).
Discussion: Hospitalized patients with systemic sclerosis experience significantly higher risks of mesenteric vasculitis, GI bleeding, and mortality. These findings highlight the need for vigilant GI monitoring and risk mitigation in SSC hospital care.
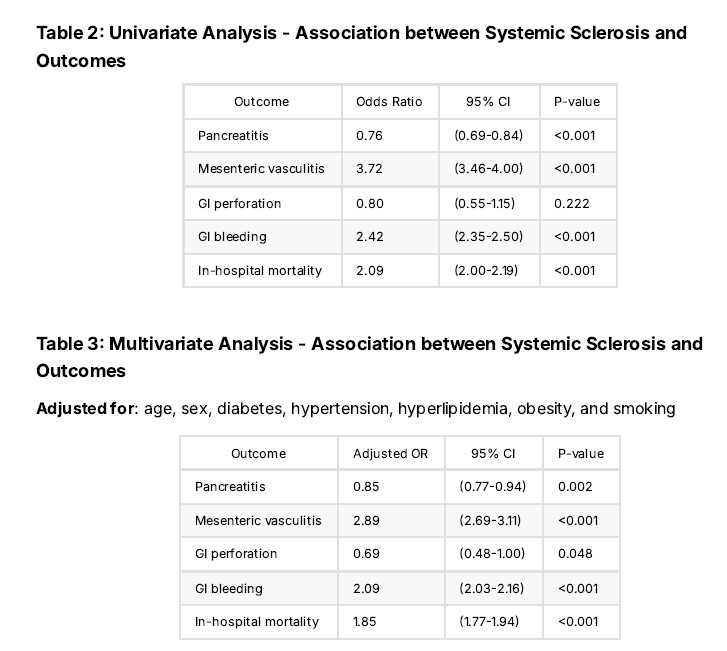
Figure: Demographics and Clinical Characteristics
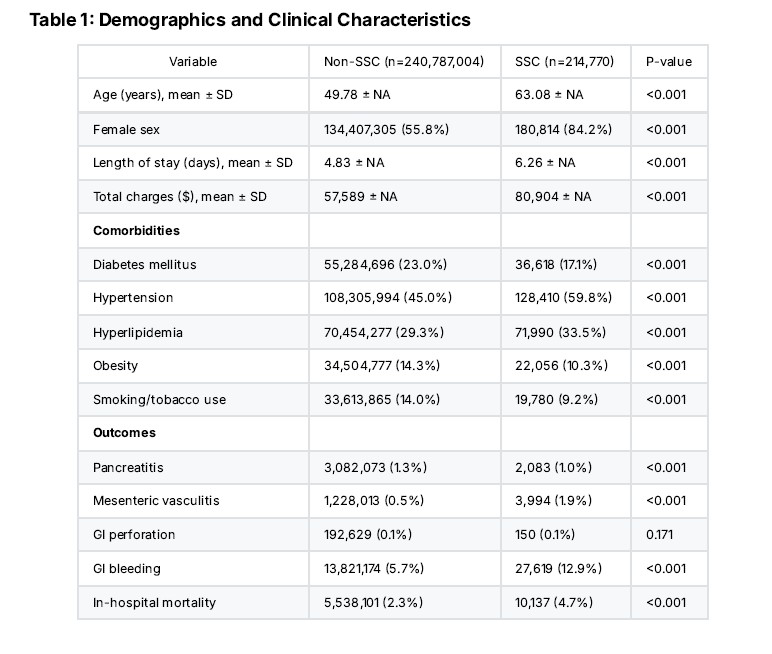
Figure: Univariate & Multivariate Analysis - Association between Systemic Sclerosis and Outcomes
Disclosures:
Sreekant Avula indicated no relevant financial relationships.
Vinay Thallapally indicated no relevant financial relationships.
Khalid Ahmed indicated no relevant financial relationships.
Mahesh Cheryala indicated no relevant financial relationships.
Sreekant Avula, MBBS1, Vinay Thallapally, MBBS2, Khalid Ahmed, MD3, Mahesh Cheryala, MD4. P3065 - A Nationwide Cross-Sectional Study of Gastrointestinal Outcomes in Systemic Sclerosis: A National Inpatient Sample (2016–2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

