Monday Poster Session
Category: GI Bleeding
P3059 - Bridging the Gap Between Guidelines and Clinical Practice: Continuation of Nonselective Beta-Blocker Therapy to Prevent Variceal Haemorrhage in Patients With High Risk Varices
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Haniya Waseem, MD (she/her/hers)
AdventHealth
Tampa, FL
Presenting Author(s)
Award: ACG Presidential Poster Award
Haniya Waseem, MD, FNU Naina, MD, Muhammad Umair, MD, Muhammad Ahmad, MD, Adnan Muhammad, MD, FACG
AdventHealth, Tampa, FL
Introduction: Decompensated cirrhosis, an advanced stage of liver disease marked by significant hepatic dysfunction, is associated with markedly reduced life expectancy. Patients with cirrhosis are at increased risk of upper gastrointestinal (GI) bleeding due to lesions related to portal hypertension, including gastroesophageal varices and portal hypertensive gastropathy. According to the 2024 American Association for the Study of Liver Diseases (AASLD) practice guidance, patients with high-risk varices should receive either nonselective beta-blockers (NSBBs) or endoscopic band ligation (EBL), with preference given to NSBBs due to additional benefits beyond prevention of variceal haemorrhage.
This study aims to evaluate adherence to AASLD guidelines in the prescription of NSBBs in patients with cirrhosis presenting with upper GI bleeding.
Methods: We conducted a retrospective chart review of patients with cirrhosis admitted to an academic tertiary care centre between January and December 2024. Collected demographic data included age, gender, BMI, and ethnicity, along with cirrhosis-specific variables such as etiology, MELD score, presence of ascites or hepatic encephalopathy, and discharge medications. We also documented whether the indication for NSBB prescription was primary (prophylaxis) or secondary (post-variceal bleeding) prevention. Reasons for non-prescription were also assessed.
Results: A total of 61 patients were reviewed. After removing duplicates and non-cirrhotic upper GI bleeding cases, 57 patients were included in the final analysis. Among them, 31.57% were prescribed nonselective beta-blockers appropriately, 63.11% were not prescribed NSBBs, and 5.2% died during admission.
Discussion: Our findings highlight a persistent gap between AASLD guideline recommendations and real-world clinical practice in the management of patients with cirrhosis and high-risk varices. Despite clear evidence supporting NSBB use, a substantial proportion of eligible patients were not discharged with appropriate therapy. To bridge this gap, targeted strategies such as implementing standardized discharge protocols with built-in electronic reminders, enhancing provider education on guideline updates, and improving care coordination during transitions of care are recommended. This study is limited by its retrospective nature and reliance on documentation accuracy within the EMR. Additionally, it was conducted at a single academic centre, which may limit generalizability.
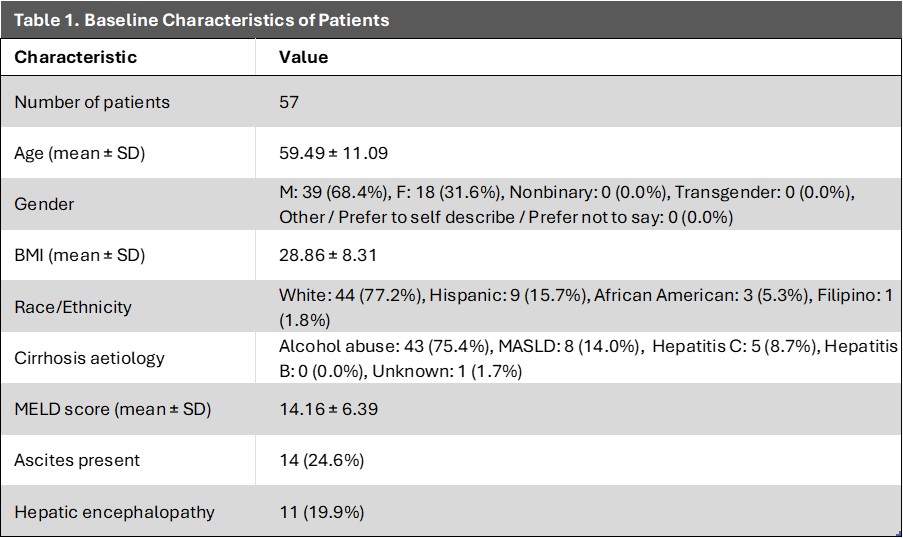
Figure: Table1: Baseline characteristics of patients
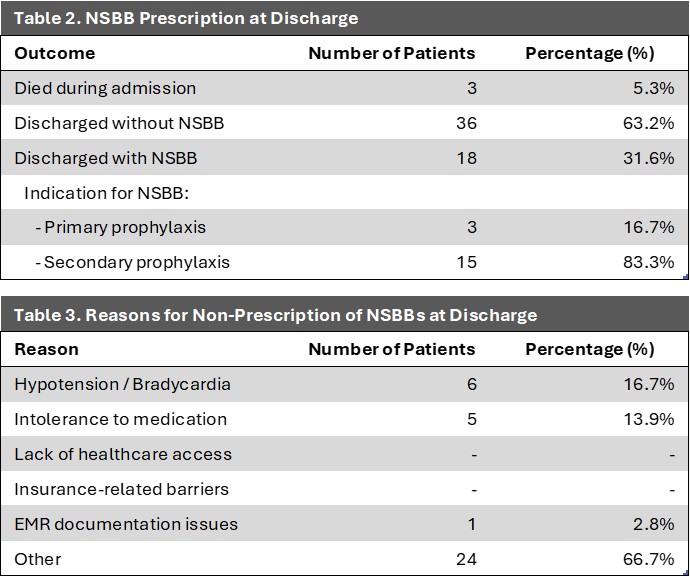
Figure: Table 2: Prescription of NSBB at discharge
Table 3: Reasons for non-prescription of NSBB at discharge
Disclosures:
Haniya Waseem indicated no relevant financial relationships.
FNU Naina indicated no relevant financial relationships.
Muhammad Umair indicated no relevant financial relationships.
Muhammad Ahmad indicated no relevant financial relationships.
Adnan Muhammad indicated no relevant financial relationships.
Haniya Waseem, MD, FNU Naina, MD, Muhammad Umair, MD, Muhammad Ahmad, MD, Adnan Muhammad, MD, FACG. P3059 - Bridging the Gap Between Guidelines and Clinical Practice: Continuation of Nonselective Beta-Blocker Therapy to Prevent Variceal Haemorrhage in Patients With High Risk Varices, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Haniya Waseem, MD, FNU Naina, MD, Muhammad Umair, MD, Muhammad Ahmad, MD, Adnan Muhammad, MD, FACG
AdventHealth, Tampa, FL
Introduction: Decompensated cirrhosis, an advanced stage of liver disease marked by significant hepatic dysfunction, is associated with markedly reduced life expectancy. Patients with cirrhosis are at increased risk of upper gastrointestinal (GI) bleeding due to lesions related to portal hypertension, including gastroesophageal varices and portal hypertensive gastropathy. According to the 2024 American Association for the Study of Liver Diseases (AASLD) practice guidance, patients with high-risk varices should receive either nonselective beta-blockers (NSBBs) or endoscopic band ligation (EBL), with preference given to NSBBs due to additional benefits beyond prevention of variceal haemorrhage.
This study aims to evaluate adherence to AASLD guidelines in the prescription of NSBBs in patients with cirrhosis presenting with upper GI bleeding.
Methods: We conducted a retrospective chart review of patients with cirrhosis admitted to an academic tertiary care centre between January and December 2024. Collected demographic data included age, gender, BMI, and ethnicity, along with cirrhosis-specific variables such as etiology, MELD score, presence of ascites or hepatic encephalopathy, and discharge medications. We also documented whether the indication for NSBB prescription was primary (prophylaxis) or secondary (post-variceal bleeding) prevention. Reasons for non-prescription were also assessed.
Results: A total of 61 patients were reviewed. After removing duplicates and non-cirrhotic upper GI bleeding cases, 57 patients were included in the final analysis. Among them, 31.57% were prescribed nonselective beta-blockers appropriately, 63.11% were not prescribed NSBBs, and 5.2% died during admission.
Discussion: Our findings highlight a persistent gap between AASLD guideline recommendations and real-world clinical practice in the management of patients with cirrhosis and high-risk varices. Despite clear evidence supporting NSBB use, a substantial proportion of eligible patients were not discharged with appropriate therapy. To bridge this gap, targeted strategies such as implementing standardized discharge protocols with built-in electronic reminders, enhancing provider education on guideline updates, and improving care coordination during transitions of care are recommended. This study is limited by its retrospective nature and reliance on documentation accuracy within the EMR. Additionally, it was conducted at a single academic centre, which may limit generalizability.
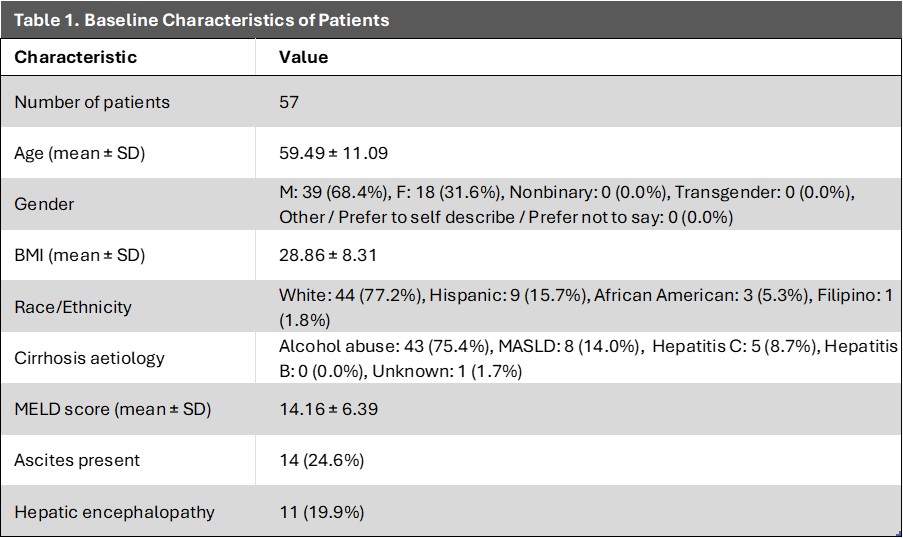
Figure: Table1: Baseline characteristics of patients
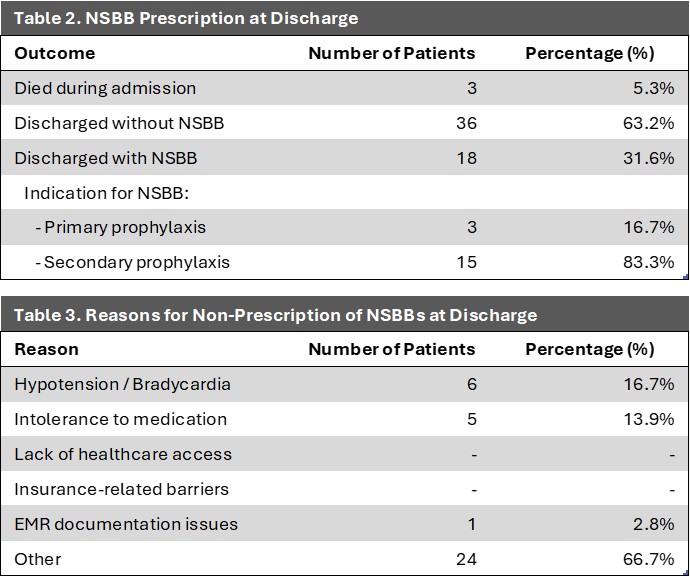
Figure: Table 2: Prescription of NSBB at discharge
Table 3: Reasons for non-prescription of NSBB at discharge
Disclosures:
Haniya Waseem indicated no relevant financial relationships.
FNU Naina indicated no relevant financial relationships.
Muhammad Umair indicated no relevant financial relationships.
Muhammad Ahmad indicated no relevant financial relationships.
Adnan Muhammad indicated no relevant financial relationships.
Haniya Waseem, MD, FNU Naina, MD, Muhammad Umair, MD, Muhammad Ahmad, MD, Adnan Muhammad, MD, FACG. P3059 - Bridging the Gap Between Guidelines and Clinical Practice: Continuation of Nonselective Beta-Blocker Therapy to Prevent Variceal Haemorrhage in Patients With High Risk Varices, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

