Monday Poster Session
Category: GI Bleeding
P3048 - Impact of EGD on Embolization Strategies During Catheter Angiography in Non-Variceal Upper Gastrointestinal Bleeding
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nurlan Aliyev, MD
University of Nebraska Medical Center
Elkhorn, NE
Presenting Author(s)
Nurlan Aliyev, MD1, Anasua Deb, MD2, Abu Fahad Abbasi, MD3, Elizabeth R. Lyden, MS2, Kathryn Hutchins, MD, FACG2, Fedja A. Rochling, MBBCh, MBA4, Ishfaq Bhat, MD2
1University of Nebraska Medical Center, Elkhorn, NE; 2University of Nebraska Medical Center, Omaha, NE; 3Mercyhealth Gastroenterology Fellowship, Rockford, IL; 4UNMC, Omaha, NE
Introduction: Endoscopic hemostasis is the first-line approach for acute non-variceal upper gastrointestinal bleeding (NVUGIB) after initial stabilization, with success rates exceeding 90%. However, up to 20% of patients experience further bleeding despite initial treatment. Current practice guidelines recommend considering a second endoscopy before transcatheter arterial embolization (TAE) in cases of recurrent bleeding, however, this is a conditional recommendation with very low-quality evidence. The impact of prior endoscopic procedures on intra-angiogram embolization strategies (e.g., no embolization, empiric, and therapeutic embolization) remains poorly understood. This study aimed to assess how the pre-angiographic esophagogastroduodenoscopy (EGD) influences embolization strategies.
Methods: This single-center retrospective study included 92 consecutive patients diagnosed with acute NVUGIB who underwent catheter angiogram (CA) with the intention of embolization from January 2010 to August 2023 at the University of Nebraska Medical Center. Data was extracted from patients’ electronic medical records and stratified into three groups based on type of embolization: no embolization, empiric, and therapeutic embolization. The groups were further categorized according to the number of EGDs performed before CA (no EGD, 1 EGD, and ≥2 EGDs). Pairwise comparison was performed using Fisher’s Exact Test, with P-values adjusted using the Bonferroni method.
Results: 92 patients (52% male, mean age of 64) were included in the study. Baseline characteristics were similar across the study groups (Table 1). A total of 11 (12%) patients received no embolization, 54 (58.7%) empiric, and 27 (29.3%) therapeutic embolization (Table 2). The majority of patients who did not receive embolization (81.8%) had ≥2 EGD before CA, while most patients who received empiric (63%) and therapeutic (54.3%) embolization had 1 EGD before CA (P< 0.0001). Pairwise comparisons showed significant differences in embolization strategy between patients who had 0 EGD versus ≥ 2 EGDs (P=0.0073) and between patients with 1 EGD versus ≥2 EGDs (P=0.0023).
Discussion: Current literature suggests that both empiric and therapeutic embolization is superior to no embolization in NVUGIB. Also, pre-CA EGD known to improve targeted embolization. This study suggest that patients who had 1 EGD before CA were more likely to receive embolization than those who had 0 EGD and ≥2 EGDs. Large scale studies are warranted to confirm the finding.
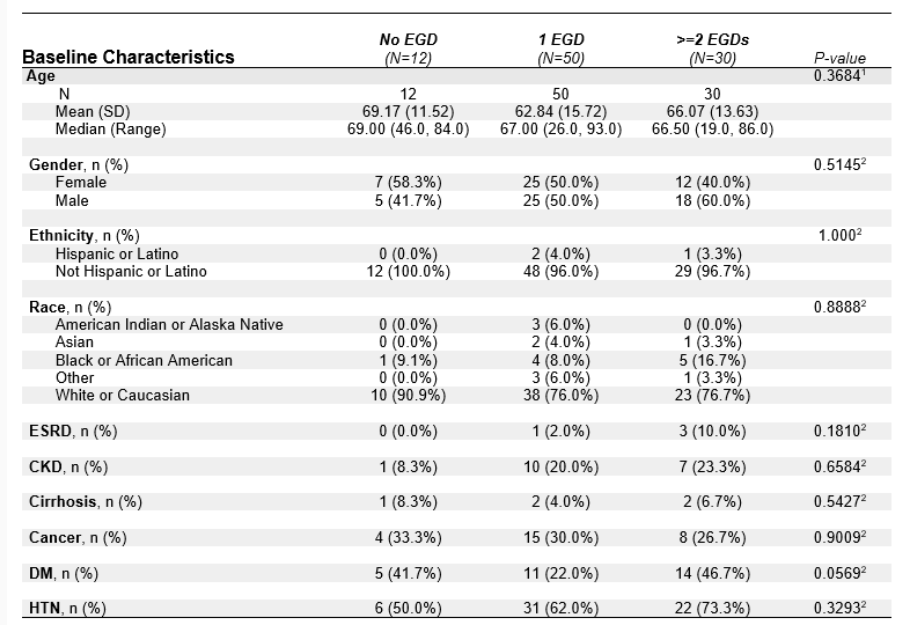
Figure: Baseline characteristics

Figure: Results
Disclosures:
Nurlan Aliyev indicated no relevant financial relationships.
Anasua Deb indicated no relevant financial relationships.
Abu Fahad Abbasi indicated no relevant financial relationships.
Elizabeth R. Lyden indicated no relevant financial relationships.
Kathryn Hutchins indicated no relevant financial relationships.
Fedja Rochling indicated no relevant financial relationships.
Ishfaq Bhat indicated no relevant financial relationships.
Nurlan Aliyev, MD1, Anasua Deb, MD2, Abu Fahad Abbasi, MD3, Elizabeth R. Lyden, MS2, Kathryn Hutchins, MD, FACG2, Fedja A. Rochling, MBBCh, MBA4, Ishfaq Bhat, MD2. P3048 - Impact of EGD on Embolization Strategies During Catheter Angiography in Non-Variceal Upper Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Nebraska Medical Center, Elkhorn, NE; 2University of Nebraska Medical Center, Omaha, NE; 3Mercyhealth Gastroenterology Fellowship, Rockford, IL; 4UNMC, Omaha, NE
Introduction: Endoscopic hemostasis is the first-line approach for acute non-variceal upper gastrointestinal bleeding (NVUGIB) after initial stabilization, with success rates exceeding 90%. However, up to 20% of patients experience further bleeding despite initial treatment. Current practice guidelines recommend considering a second endoscopy before transcatheter arterial embolization (TAE) in cases of recurrent bleeding, however, this is a conditional recommendation with very low-quality evidence. The impact of prior endoscopic procedures on intra-angiogram embolization strategies (e.g., no embolization, empiric, and therapeutic embolization) remains poorly understood. This study aimed to assess how the pre-angiographic esophagogastroduodenoscopy (EGD) influences embolization strategies.
Methods: This single-center retrospective study included 92 consecutive patients diagnosed with acute NVUGIB who underwent catheter angiogram (CA) with the intention of embolization from January 2010 to August 2023 at the University of Nebraska Medical Center. Data was extracted from patients’ electronic medical records and stratified into three groups based on type of embolization: no embolization, empiric, and therapeutic embolization. The groups were further categorized according to the number of EGDs performed before CA (no EGD, 1 EGD, and ≥2 EGDs). Pairwise comparison was performed using Fisher’s Exact Test, with P-values adjusted using the Bonferroni method.
Results: 92 patients (52% male, mean age of 64) were included in the study. Baseline characteristics were similar across the study groups (Table 1). A total of 11 (12%) patients received no embolization, 54 (58.7%) empiric, and 27 (29.3%) therapeutic embolization (Table 2). The majority of patients who did not receive embolization (81.8%) had ≥2 EGD before CA, while most patients who received empiric (63%) and therapeutic (54.3%) embolization had 1 EGD before CA (P< 0.0001). Pairwise comparisons showed significant differences in embolization strategy between patients who had 0 EGD versus ≥ 2 EGDs (P=0.0073) and between patients with 1 EGD versus ≥2 EGDs (P=0.0023).
Discussion: Current literature suggests that both empiric and therapeutic embolization is superior to no embolization in NVUGIB. Also, pre-CA EGD known to improve targeted embolization. This study suggest that patients who had 1 EGD before CA were more likely to receive embolization than those who had 0 EGD and ≥2 EGDs. Large scale studies are warranted to confirm the finding.
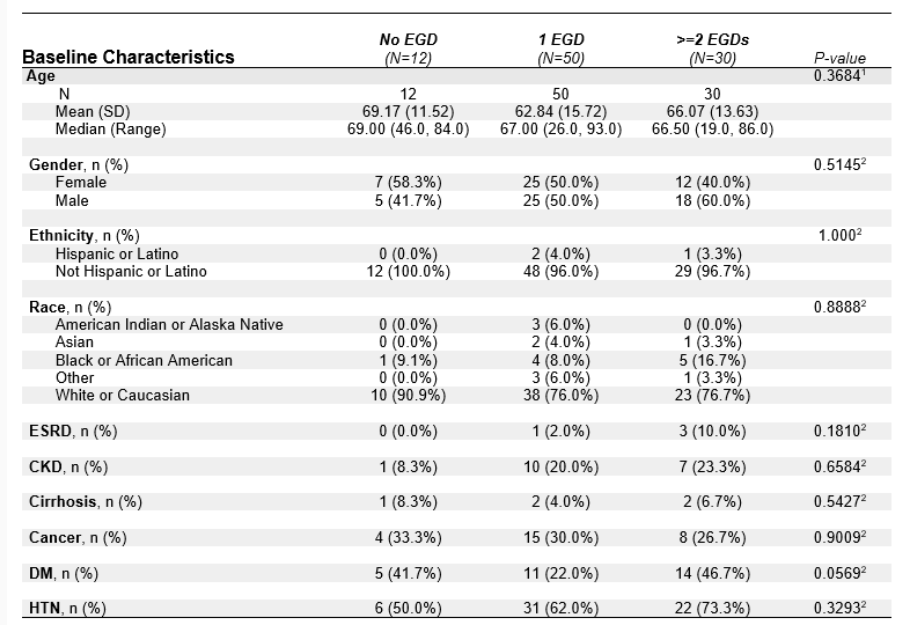
Figure: Baseline characteristics

Figure: Results
Disclosures:
Nurlan Aliyev indicated no relevant financial relationships.
Anasua Deb indicated no relevant financial relationships.
Abu Fahad Abbasi indicated no relevant financial relationships.
Elizabeth R. Lyden indicated no relevant financial relationships.
Kathryn Hutchins indicated no relevant financial relationships.
Fedja Rochling indicated no relevant financial relationships.
Ishfaq Bhat indicated no relevant financial relationships.
Nurlan Aliyev, MD1, Anasua Deb, MD2, Abu Fahad Abbasi, MD3, Elizabeth R. Lyden, MS2, Kathryn Hutchins, MD, FACG2, Fedja A. Rochling, MBBCh, MBA4, Ishfaq Bhat, MD2. P3048 - Impact of EGD on Embolization Strategies During Catheter Angiography in Non-Variceal Upper Gastrointestinal Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
