Monday Poster Session
Category: GI Bleeding
P3155 - Gastrointestinal Hemorrhage Secondary to Pancreaticoduodenal Aneurysm Into Duodenum
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
John M. Sullivan, III, MD
Henry Ford Health Genesys Hospital
Grand Blanc, MI
Presenting Author(s)
Brandon Wiggins, DO, MPH, Mark Rigby, DO, John M. Sullivan, MD, Sonika Gill-Ahluwalia, DO, Derek Thigpin, DO, Justin Miller, DO
Henry Ford Health Genesys Hospital, Grand Blanc, MI
Introduction: Pancreaticoduodenal artery (PDA) aneurysms, a rare type of visceral artery aneurysm (VAA), infrequently cause intraluminal gastrointestinal (GI) bleeding. We discuss the case of an 85-year-old male who developed an aneurysm of the inferior pancreaticoduodenal artery with erosion into the duodenum, causing symptomatic bleeding.
Case Description/
Methods: An 85-year-old male with a history of CAD on baby Aspirin presented for melena, fatigue and weakness. Hemoglobin was 4.5 g/dL with baseline two weeks before of 11.5 and a BUN:Creatinine ratio of 45, consistent with upper GI bleed. CTA demonstrated a pulmonary embolism and he was started on heparin, IV pantoprazole 40mg twice daily, and blood transfusions. Esophagogastroduodenoscopy (EGD) was performed revealing LA grade D esophagitis, but no duodenal bleeding. Ten days later, the patient had large volume melena associated with hypotension, and repeat EGD demonstrated blood clot throughout the esophagus and stomach without a source of bleeding. A repeat CT showed a PDA embedded in the wall of the second portion of duodenum with active bleeding. He underwent IR angiography that redemonstrated a PDA, but failed to show active bleeding, and no intervention performed. After bleeding subsided, blood thinners were discontinued and he was discharged.
Discussion: PDAs make up about 2% of all visceral artery aneurysms. Their pathophysiology can be explained by either stenosis, occlusion or compression of the celiac artery causing increased pressure and altered blood flow within the collateral pancreaticoduodenal arcades. Celiac stenosis has been observed in about 50-80% of patients and these aneurysms are typically discovered on CT imaging of the abdomen after clinical evaluation fails to produce a diagnosis. Patients can present with a variety of symptoms including nausea, vomiting, abdominal pain, fatigue, or melena. Unfortunately, in many cases VAAs are not discovered until after catastrophic bleeding in the retroperitoneal space of the abdomen has occurred with up to a 50% fatality rate. Our case is unique as he was past the mean age of 60 with a 8x9 mm aneurysm that became embedded in the wall of the second portion of the duodenum with a suspected slow leak. This case helps add to the literature by highlighting a rare anatomical and clinical occurrence. Gastroenterologists should be aware of PDA aneurysms when evaluating upper abdominal pain and GI bleeding as failure to do so may lead to high mortality.
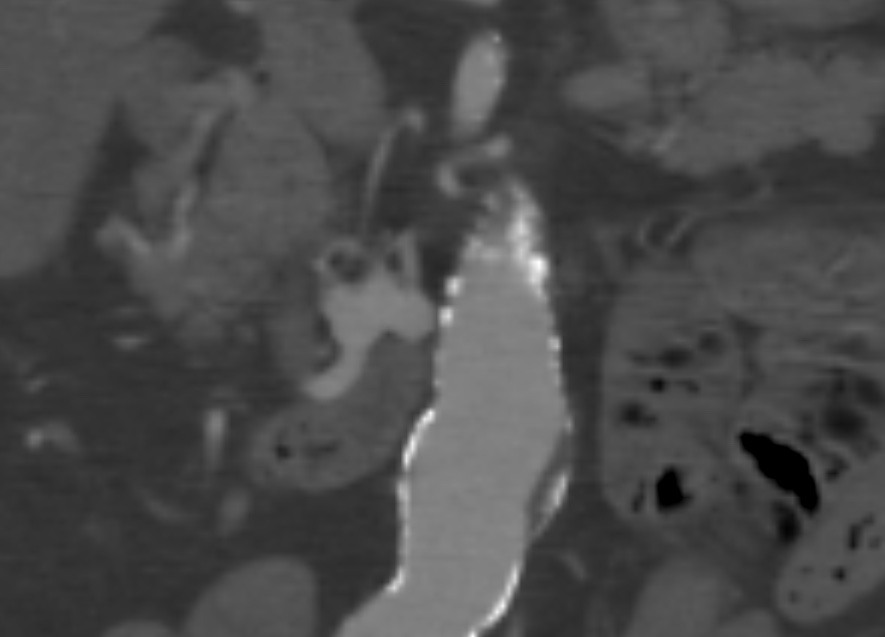
Figure: CTA of the abdomen/pelvis revealing a fusiform inferior pancreaticoduodenal artery aneurysm.
Disclosures:
Brandon Wiggins indicated no relevant financial relationships.
Mark Rigby indicated no relevant financial relationships.
John Sullivan indicated no relevant financial relationships.
Sonika Gill-Ahluwalia indicated no relevant financial relationships.
Derek Thigpin indicated no relevant financial relationships.
Justin Miller indicated no relevant financial relationships.
Brandon Wiggins, DO, MPH, Mark Rigby, DO, John M. Sullivan, MD, Sonika Gill-Ahluwalia, DO, Derek Thigpin, DO, Justin Miller, DO. P3155 - Gastrointestinal Hemorrhage Secondary to Pancreaticoduodenal Aneurysm Into Duodenum, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Henry Ford Health Genesys Hospital, Grand Blanc, MI
Introduction: Pancreaticoduodenal artery (PDA) aneurysms, a rare type of visceral artery aneurysm (VAA), infrequently cause intraluminal gastrointestinal (GI) bleeding. We discuss the case of an 85-year-old male who developed an aneurysm of the inferior pancreaticoduodenal artery with erosion into the duodenum, causing symptomatic bleeding.
Case Description/
Methods: An 85-year-old male with a history of CAD on baby Aspirin presented for melena, fatigue and weakness. Hemoglobin was 4.5 g/dL with baseline two weeks before of 11.5 and a BUN:Creatinine ratio of 45, consistent with upper GI bleed. CTA demonstrated a pulmonary embolism and he was started on heparin, IV pantoprazole 40mg twice daily, and blood transfusions. Esophagogastroduodenoscopy (EGD) was performed revealing LA grade D esophagitis, but no duodenal bleeding. Ten days later, the patient had large volume melena associated with hypotension, and repeat EGD demonstrated blood clot throughout the esophagus and stomach without a source of bleeding. A repeat CT showed a PDA embedded in the wall of the second portion of duodenum with active bleeding. He underwent IR angiography that redemonstrated a PDA, but failed to show active bleeding, and no intervention performed. After bleeding subsided, blood thinners were discontinued and he was discharged.
Discussion: PDAs make up about 2% of all visceral artery aneurysms. Their pathophysiology can be explained by either stenosis, occlusion or compression of the celiac artery causing increased pressure and altered blood flow within the collateral pancreaticoduodenal arcades. Celiac stenosis has been observed in about 50-80% of patients and these aneurysms are typically discovered on CT imaging of the abdomen after clinical evaluation fails to produce a diagnosis. Patients can present with a variety of symptoms including nausea, vomiting, abdominal pain, fatigue, or melena. Unfortunately, in many cases VAAs are not discovered until after catastrophic bleeding in the retroperitoneal space of the abdomen has occurred with up to a 50% fatality rate. Our case is unique as he was past the mean age of 60 with a 8x9 mm aneurysm that became embedded in the wall of the second portion of the duodenum with a suspected slow leak. This case helps add to the literature by highlighting a rare anatomical and clinical occurrence. Gastroenterologists should be aware of PDA aneurysms when evaluating upper abdominal pain and GI bleeding as failure to do so may lead to high mortality.
Figure: CTA of the abdomen/pelvis revealing a fusiform inferior pancreaticoduodenal artery aneurysm.
Disclosures:
Brandon Wiggins indicated no relevant financial relationships.
Mark Rigby indicated no relevant financial relationships.
John Sullivan indicated no relevant financial relationships.
Sonika Gill-Ahluwalia indicated no relevant financial relationships.
Derek Thigpin indicated no relevant financial relationships.
Justin Miller indicated no relevant financial relationships.
Brandon Wiggins, DO, MPH, Mark Rigby, DO, John M. Sullivan, MD, Sonika Gill-Ahluwalia, DO, Derek Thigpin, DO, Justin Miller, DO. P3155 - Gastrointestinal Hemorrhage Secondary to Pancreaticoduodenal Aneurysm Into Duodenum, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
