Monday Poster Session
Category: GI Bleeding
P3154 - When Purpura Isn't Skin Deep: Recurrent GI Bleeding Secondary to IgA Vasculitis in a Young Adult
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Anjali Rajagopal, MBBS
University of Connecticut
Hartford, CT
Presenting Author(s)
Anjali Rajagopal, MBBS1, Karthik Mathialagan, MD2, Haleh Vaziri, MD3
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut, Farmington, CT; 3UConn, Farmington, CT
Introduction: IgA vasculitis (IgAV) or Henoch-Schönlein Purpura (HSP), is a small-vessel, immune-complex vasculitis with skin, renal & gastrointestinal (GI) manifestations. IgAV predominantly affects pediatric populations & is rare in older patients, with an estimated annual incidence between 0.8 to 2 cases per 100,000 adults. GI manifestations occur in a significant number of patients who present with severe abdominal pain, nausea, vomiting & GI bleeding.
Case Description/
Methods: A 22-year-old male with a past medical history of IgA Vasculitis & Juvenile Idiopathic Arthritis (psoriatic subtype) presented to the ED with 2 days of acute abdominal pain, hematemesis & hematochezia. He was hemodynamically stable on presentation with labs notable for elevated WBC count 20 × 10⁹/L, hemoglobin 16.5 g/dL, platelet count 378 × 10⁹/L, & INR 1.1. Immunoglobulin levels were notable for IgA 972 mg/dL, IgG 433 mg/dL, & IgM 86 mg/dL. CTA of the abdomen & pelvis demonstrated a thickened stomach wall & proximal small bowel with mesenteric lymphadenopathy. EGD was notable for severe erythema & edema with superficial ulcerations in the second part of the duodenum (Fig 1 A & B). Pathology showed severe acute duodenitis with ulceration, ischemic changes, & capillaritis. Immunohistochemistry (IHC) revealed an abundance of IgA positive cells. During a prior IgAV flare with rectal bleeding and palpable purpura (Fig.2), CT A&P demonstrated terminal ileum thickening. Patient received IV steroids with good symptom improvement. Subsequent colonoscopy was unrevealing.
Discussion: IgAV is driven by IgA immune-complex deposition, complement activation & neutrophil-mediated vessel injury causing characteristic abdominal pain & bleeding. IgAV is associated with a poorer prognosis in adults with a frequency of GI symptoms ranging between 37- 65%. Despite this, there is limited literature on the treatment, prognostication, & risk of relapse in adults. In rare cases, fatal episodes of acute surgical abdomen may occur due to mesenteric ischemia & perforation. The mainstay of treatment includes short-course steroids during acute flares. There is limited evidence to guide long term treatment, given the unpredictable natural history of the disease, and randomized clinical trials are warranted to design optimal regimens. Vasculitic causes of GI bleeding must be considered in young adults with autoimmune history, as GI manifestations may not temporally correlate with the presence of skin purpura, causing diagnostic delays.
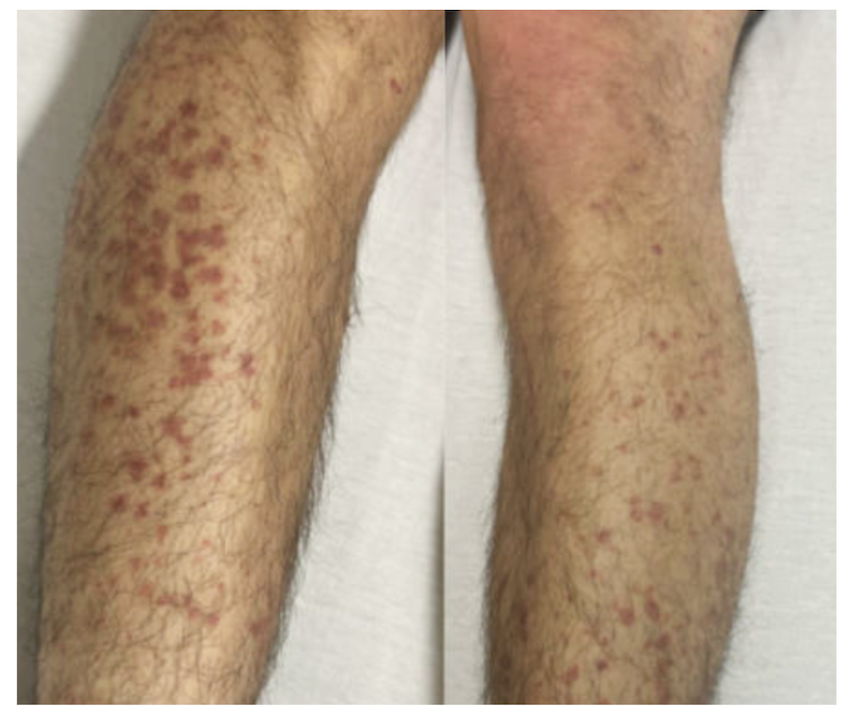
Figure: 1A & B: Second portion of the duodenum depicting erythematous duodenitis on Esophagogastroduodenoscopy (EGD)
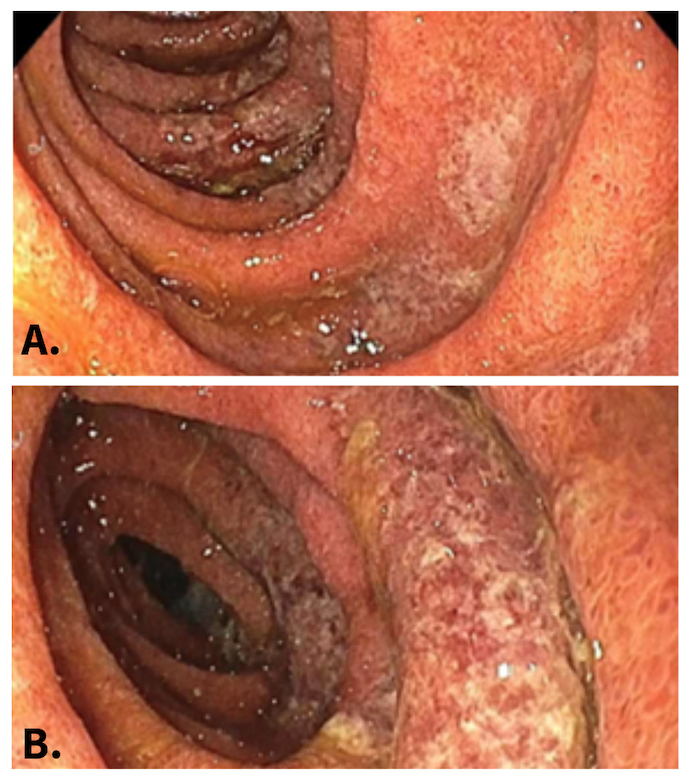
Figure: Fig. 2: Palpable purpura over bilateral lower extremities noted during prior admission for gastrointestinal bleeding
Disclosures:
Anjali Rajagopal indicated no relevant financial relationships.
Karthik Mathialagan indicated no relevant financial relationships.
Haleh Vaziri indicated no relevant financial relationships.
Anjali Rajagopal, MBBS1, Karthik Mathialagan, MD2, Haleh Vaziri, MD3. P3154 - When Purpura Isn't Skin Deep: Recurrent GI Bleeding Secondary to IgA Vasculitis in a Young Adult, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut, Farmington, CT; 3UConn, Farmington, CT
Introduction: IgA vasculitis (IgAV) or Henoch-Schönlein Purpura (HSP), is a small-vessel, immune-complex vasculitis with skin, renal & gastrointestinal (GI) manifestations. IgAV predominantly affects pediatric populations & is rare in older patients, with an estimated annual incidence between 0.8 to 2 cases per 100,000 adults. GI manifestations occur in a significant number of patients who present with severe abdominal pain, nausea, vomiting & GI bleeding.
Case Description/
Methods: A 22-year-old male with a past medical history of IgA Vasculitis & Juvenile Idiopathic Arthritis (psoriatic subtype) presented to the ED with 2 days of acute abdominal pain, hematemesis & hematochezia. He was hemodynamically stable on presentation with labs notable for elevated WBC count 20 × 10⁹/L, hemoglobin 16.5 g/dL, platelet count 378 × 10⁹/L, & INR 1.1. Immunoglobulin levels were notable for IgA 972 mg/dL, IgG 433 mg/dL, & IgM 86 mg/dL. CTA of the abdomen & pelvis demonstrated a thickened stomach wall & proximal small bowel with mesenteric lymphadenopathy. EGD was notable for severe erythema & edema with superficial ulcerations in the second part of the duodenum (Fig 1 A & B). Pathology showed severe acute duodenitis with ulceration, ischemic changes, & capillaritis. Immunohistochemistry (IHC) revealed an abundance of IgA positive cells. During a prior IgAV flare with rectal bleeding and palpable purpura (Fig.2), CT A&P demonstrated terminal ileum thickening. Patient received IV steroids with good symptom improvement. Subsequent colonoscopy was unrevealing.
Discussion: IgAV is driven by IgA immune-complex deposition, complement activation & neutrophil-mediated vessel injury causing characteristic abdominal pain & bleeding. IgAV is associated with a poorer prognosis in adults with a frequency of GI symptoms ranging between 37- 65%. Despite this, there is limited literature on the treatment, prognostication, & risk of relapse in adults. In rare cases, fatal episodes of acute surgical abdomen may occur due to mesenteric ischemia & perforation. The mainstay of treatment includes short-course steroids during acute flares. There is limited evidence to guide long term treatment, given the unpredictable natural history of the disease, and randomized clinical trials are warranted to design optimal regimens. Vasculitic causes of GI bleeding must be considered in young adults with autoimmune history, as GI manifestations may not temporally correlate with the presence of skin purpura, causing diagnostic delays.
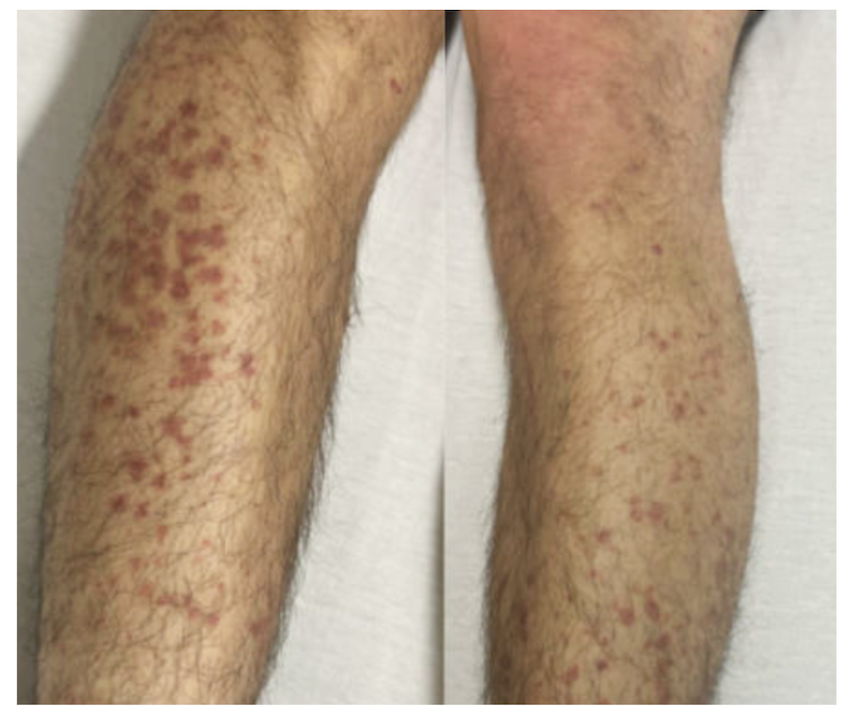
Figure: 1A & B: Second portion of the duodenum depicting erythematous duodenitis on Esophagogastroduodenoscopy (EGD)
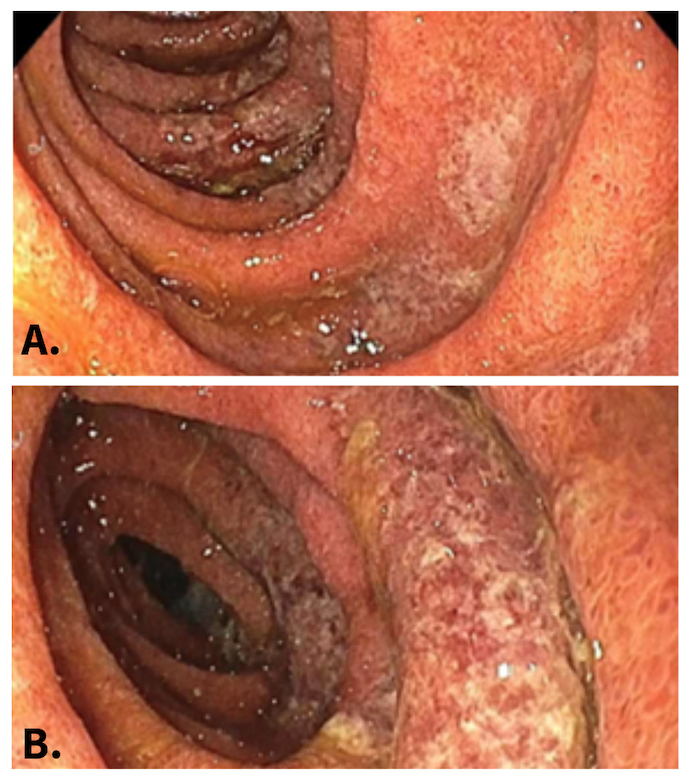
Figure: Fig. 2: Palpable purpura over bilateral lower extremities noted during prior admission for gastrointestinal bleeding
Disclosures:
Anjali Rajagopal indicated no relevant financial relationships.
Karthik Mathialagan indicated no relevant financial relationships.
Haleh Vaziri indicated no relevant financial relationships.
Anjali Rajagopal, MBBS1, Karthik Mathialagan, MD2, Haleh Vaziri, MD3. P3154 - When Purpura Isn't Skin Deep: Recurrent GI Bleeding Secondary to IgA Vasculitis in a Young Adult, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

