Monday Poster Session
Category: IBD
P3371 - Drug-Induced Crohn’s Disease Following Ixekizumab Use in a Patient With Psoriasis: A Case Report
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Olanrewaju Adeniran, MD (he/him/his)
West Virginia University Morgantown
Morgantown, WV
Presenting Author(s)
Olanrewaju Adeniran, MD1, George Obeng, MD2, Justin Kupec, MD, FACG2, William Hsueh, MD3
1West Virginia University Morgantown, Morgantown, WV; 2West Virginia University School of Medicine, Morgantown, WV; 3Visalia Medical Clinic, Adventist Health Physicians Network, Visalia, CA
Introduction: Psoriasis and inflammatory bowel disease (IBD), comprising ulcerative colitis (UC) and Crohn’s disease (CD), often co-occur due to shared pathophysiology involving tumor necrosis factor alpha (TNFα) and interleukins (IL) like IL-17 and IL-23. Biologics targeting TNFα and IL-23 are therefore used to manage both conditions. However, recommendations exist against using IL-17-based therapy. We describe a rare case of new-onset CD following initiation of ixekizumab, an IL-17 inhibitor, for psoriasis.
Case Description/
Methods: A 59-year-old female presented with a month of diarrhea and abdominal pain, 4 weeks after starting ixekizumab. Symptoms escalated from 3-4 to 6-7 loose stools/day. She had no IBD history or risk factors. Laboratory values showed hemoglobin 10.7 g/dL, C-reactive protein (26.37 mg/dL), and fecal calprotectin (4110 μg/g). Colonoscopy revealed multiple, pan-colonic, deep and inflamed ulcers, with skip lesions, more pronounced in the left colon and rectum (Figure 1a-d). Histopathology demonstrated moderate to severe chronic active pancolitis. Symptoms improved after ixekizumab discontinuation. Prednisone induction along with infliximab 10 mg/kg infusions resulted in improved stool frequency (2 episodes/day), consistency, and inflammatory markers. Repeat colonoscopy 15 months later, showed significantly improved colitis (Figure 1e-h). Simple Endoscopic Score for Crohn’s disease improved from 33 to 9.
Discussion: IL-17 plays contrasting roles in psoriasis and IBD. In psoriasis, it promotes keratinocyte proliferation, leading to the characteristic scaly plaques. However, in IBD, it maintains intestinal epithelial integrity and antimicrobial defense. This distinction explains the differing roles of IL-17 inhibition in both conditions. While a few studies have reported IBD exacerbations following IL-17-based therapy, new-onset IBD is very rare. Endoscopically, IL-17 inhibitor-induced colitis may mimic UC or CD, often necessitating a multidisciplinary approach for accurate diagnosis. Our patient's transmural ulcers, skip lesions, and rectal involvement favored CD despite normal terminal ileum and absence of granulomas. Treatment involves discontinuing the offending IL-17 inhibitor, induction with corticosteroids, and initiating biologics, often a TNF-α inhibitor, an IL-12/23 inhibitor, or an IL-23 inhibitor, as demonstrated in recent trials. This case underscores the importance of considering potential IBD risk when initiating IL-17 inhibitors.
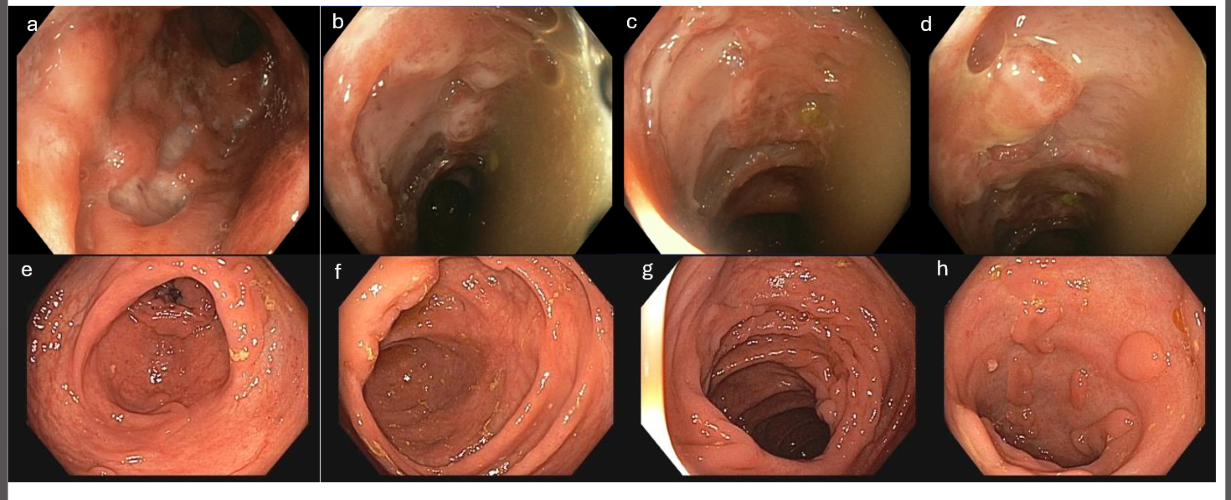
Figure: Figure 1: a-d demonstrates the left colon with multiple areas of deep, extensive, and inflamed ulcers with some sparing between the lesions. e-h shows the colon following discontinuation of ixekinumab and commencement of steroids and infliximab. Although there are still some areas of deep craters and healed ulcers, the inflammation has improved, with tiny areas of focal colitis remaining.
Disclosures:
Olanrewaju Adeniran indicated no relevant financial relationships.
George Obeng indicated no relevant financial relationships.
Justin Kupec indicated no relevant financial relationships.
William Hsueh indicated no relevant financial relationships.
Olanrewaju Adeniran, MD1, George Obeng, MD2, Justin Kupec, MD, FACG2, William Hsueh, MD3. P3371 - Drug-Induced Crohn’s Disease Following Ixekizumab Use in a Patient With Psoriasis: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1West Virginia University Morgantown, Morgantown, WV; 2West Virginia University School of Medicine, Morgantown, WV; 3Visalia Medical Clinic, Adventist Health Physicians Network, Visalia, CA
Introduction: Psoriasis and inflammatory bowel disease (IBD), comprising ulcerative colitis (UC) and Crohn’s disease (CD), often co-occur due to shared pathophysiology involving tumor necrosis factor alpha (TNFα) and interleukins (IL) like IL-17 and IL-23. Biologics targeting TNFα and IL-23 are therefore used to manage both conditions. However, recommendations exist against using IL-17-based therapy. We describe a rare case of new-onset CD following initiation of ixekizumab, an IL-17 inhibitor, for psoriasis.
Case Description/
Methods: A 59-year-old female presented with a month of diarrhea and abdominal pain, 4 weeks after starting ixekizumab. Symptoms escalated from 3-4 to 6-7 loose stools/day. She had no IBD history or risk factors. Laboratory values showed hemoglobin 10.7 g/dL, C-reactive protein (26.37 mg/dL), and fecal calprotectin (4110 μg/g). Colonoscopy revealed multiple, pan-colonic, deep and inflamed ulcers, with skip lesions, more pronounced in the left colon and rectum (Figure 1a-d). Histopathology demonstrated moderate to severe chronic active pancolitis. Symptoms improved after ixekizumab discontinuation. Prednisone induction along with infliximab 10 mg/kg infusions resulted in improved stool frequency (2 episodes/day), consistency, and inflammatory markers. Repeat colonoscopy 15 months later, showed significantly improved colitis (Figure 1e-h). Simple Endoscopic Score for Crohn’s disease improved from 33 to 9.
Discussion: IL-17 plays contrasting roles in psoriasis and IBD. In psoriasis, it promotes keratinocyte proliferation, leading to the characteristic scaly plaques. However, in IBD, it maintains intestinal epithelial integrity and antimicrobial defense. This distinction explains the differing roles of IL-17 inhibition in both conditions. While a few studies have reported IBD exacerbations following IL-17-based therapy, new-onset IBD is very rare. Endoscopically, IL-17 inhibitor-induced colitis may mimic UC or CD, often necessitating a multidisciplinary approach for accurate diagnosis. Our patient's transmural ulcers, skip lesions, and rectal involvement favored CD despite normal terminal ileum and absence of granulomas. Treatment involves discontinuing the offending IL-17 inhibitor, induction with corticosteroids, and initiating biologics, often a TNF-α inhibitor, an IL-12/23 inhibitor, or an IL-23 inhibitor, as demonstrated in recent trials. This case underscores the importance of considering potential IBD risk when initiating IL-17 inhibitors.
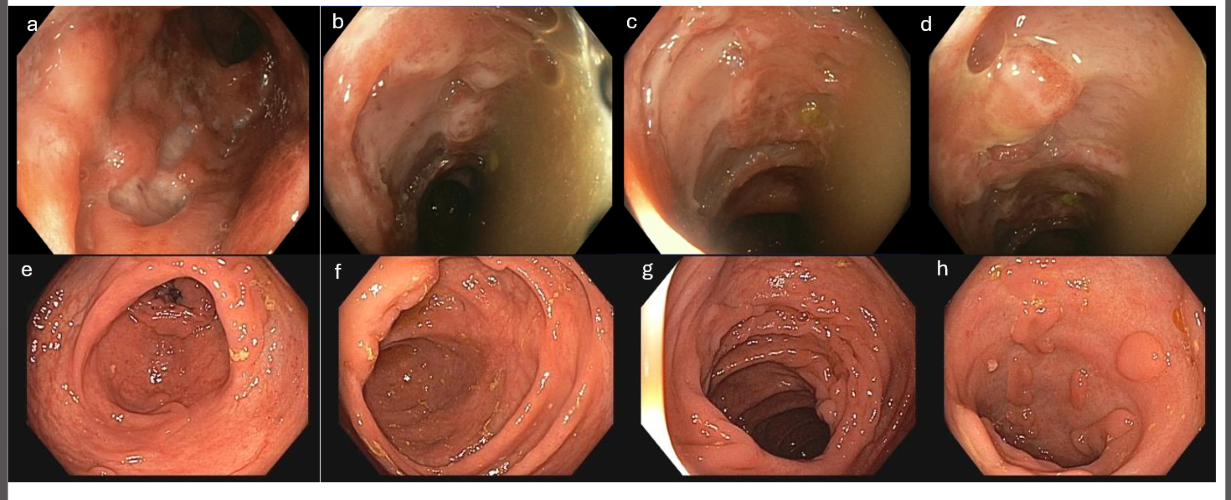
Figure: Figure 1: a-d demonstrates the left colon with multiple areas of deep, extensive, and inflamed ulcers with some sparing between the lesions. e-h shows the colon following discontinuation of ixekinumab and commencement of steroids and infliximab. Although there are still some areas of deep craters and healed ulcers, the inflammation has improved, with tiny areas of focal colitis remaining.
Disclosures:
Olanrewaju Adeniran indicated no relevant financial relationships.
George Obeng indicated no relevant financial relationships.
Justin Kupec indicated no relevant financial relationships.
William Hsueh indicated no relevant financial relationships.
Olanrewaju Adeniran, MD1, George Obeng, MD2, Justin Kupec, MD, FACG2, William Hsueh, MD3. P3371 - Drug-Induced Crohn’s Disease Following Ixekizumab Use in a Patient With Psoriasis: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

