Monday Poster Session
Category: Infections and Microbiome
P3454 - Rectal LGV Imitating Cancer: A Diagnostic Pitfall in Anorectal Pathology
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Charitha Karanam Ramapathy, MD (she/her/hers)
UAB Montgomery
Montgomery, AL
Presenting Author(s)
Charitha Karanam Ramapathy, MD1, Mahmoud Aryan, MD2, Kirk Russ, MD2
1UAB Montgomery, Montgomery, AL; 2University of Alabama at Birmingham, Birmingham, AL
Introduction: Proctitis associated with Chlamydia Trachomatis-Lymphogranuloma Venereum (LGV) is a rare but emerging cause among men who have sex with men (MSM). Infection is a rare etiology for proctitis compared to Inflammatory bowel disease(IBD), ischemia or secondary to systemic radiation therapy. Clinical presentation can mimic like any other proctitis including fevers, blood and mucoid discharge, pain and tenesmus. Isolated proctitis which is associated with sexually transmitted infections (STI) presents as a rectal mass and is mistaken for malignancy. Chlamydia is the most common bacterial STI in the United States with 50% of the cases being asymptomatic.
Case Description/
Methods: Patient is a 60-year-old male with HIV presented with intermittent bleeding per rectum for several months associated with purulent drainage. Unable to complete full digital exam due to severe anal pain with digital insertion. The IBD diagnostic panel is negative. CT abdomen and pelvis showed rectal wall thickening with prominent mesorectal lymph nodes. Colonoscopy findings in figure 1 and 2 consistent with infiltrative, polypoid, ulcerated circumferential mass in the distal rectum about 9 cm extending to the dentate line and no bleeding. Biopsies showed fragments of active colitis, ulcer and granulation tissue with no evidence of malignancy. Infectious workup showed positive chlamydia and was treated with doxycycline for 3 weeks with improvement of his symptoms. MRI of pelvis showed right sided intersphincteric perianal fistula and seton was placed. Flexible sigmoidoscopy was done a few weeks later with significant improvement of proctitis.
Discussion: The diagnosis of rectal LGV is usually delayed because of lack of classical symptoms of other etiologies of proctitis. It is extremely important to identify LGV as early as possible because of its challenges in differentiating from IBD as well as rectal malignancy. Even endoscopy or histologic evaluation might not be enough to distinguish LGV infection with mucosal ulceration, cryptitis, crypt abscesses and granuloma formation commonly seen in both. Molecular testing of LGV-specific C. trachomatis DNA from rectal swab specimens can lead to early diagnosis but seldom done. There is always risk of complications like fissures, fistulas and unnecessary invasive testing done with delayed diagnosis. Hopefully this case will help to raise awareness among healthcare providers about the different etiologies of proctitis and presentations.
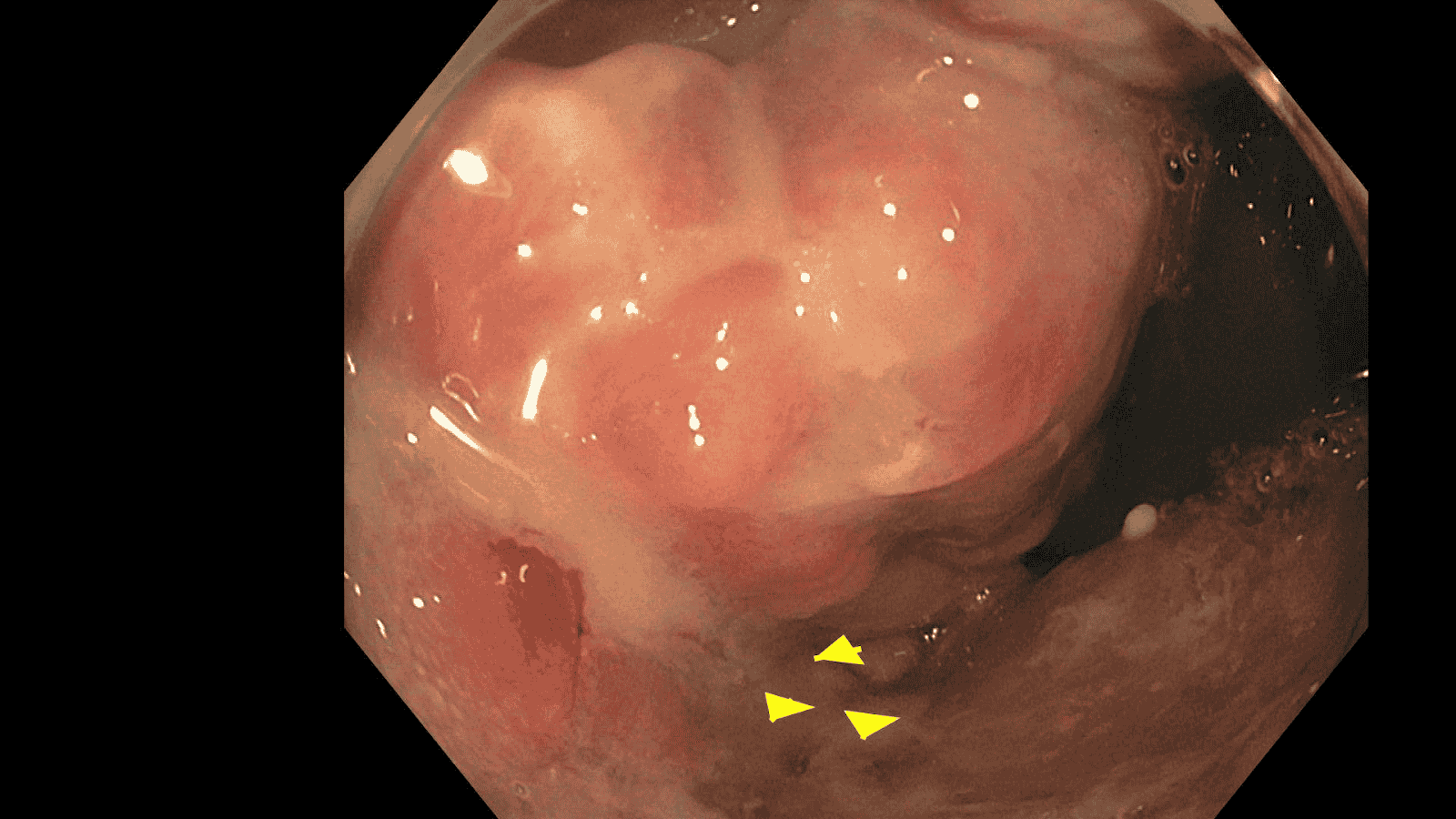
Figure: Figure 1
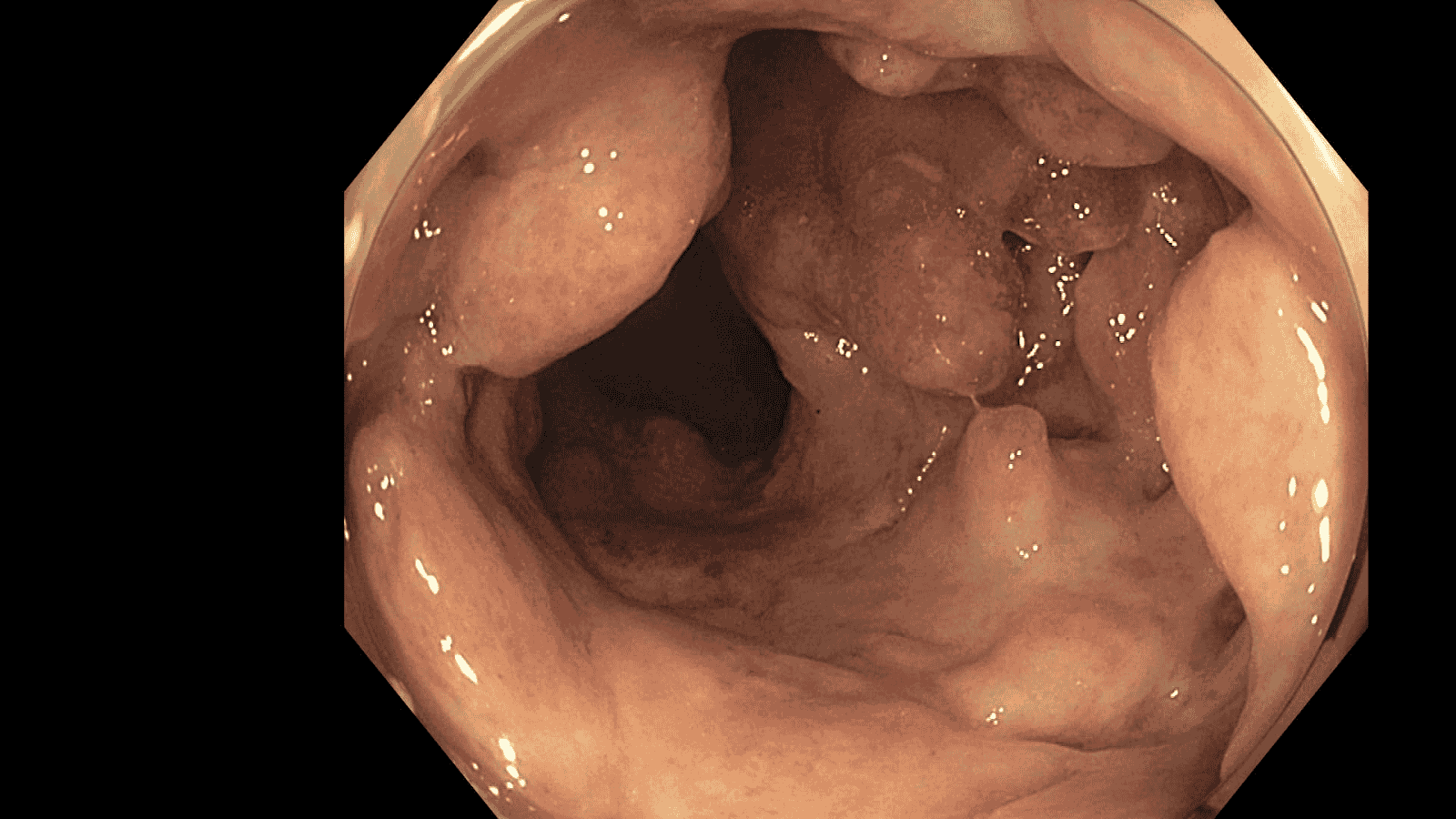
Figure: Figure 2
Disclosures:
Charitha Karanam Ramapathy indicated no relevant financial relationships.
Mahmoud Aryan indicated no relevant financial relationships.
Kirk Russ indicated no relevant financial relationships.
Charitha Karanam Ramapathy, MD1, Mahmoud Aryan, MD2, Kirk Russ, MD2. P3454 - Rectal LGV Imitating Cancer: A Diagnostic Pitfall in Anorectal Pathology, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1UAB Montgomery, Montgomery, AL; 2University of Alabama at Birmingham, Birmingham, AL
Introduction: Proctitis associated with Chlamydia Trachomatis-Lymphogranuloma Venereum (LGV) is a rare but emerging cause among men who have sex with men (MSM). Infection is a rare etiology for proctitis compared to Inflammatory bowel disease(IBD), ischemia or secondary to systemic radiation therapy. Clinical presentation can mimic like any other proctitis including fevers, blood and mucoid discharge, pain and tenesmus. Isolated proctitis which is associated with sexually transmitted infections (STI) presents as a rectal mass and is mistaken for malignancy. Chlamydia is the most common bacterial STI in the United States with 50% of the cases being asymptomatic.
Case Description/
Methods: Patient is a 60-year-old male with HIV presented with intermittent bleeding per rectum for several months associated with purulent drainage. Unable to complete full digital exam due to severe anal pain with digital insertion. The IBD diagnostic panel is negative. CT abdomen and pelvis showed rectal wall thickening with prominent mesorectal lymph nodes. Colonoscopy findings in figure 1 and 2 consistent with infiltrative, polypoid, ulcerated circumferential mass in the distal rectum about 9 cm extending to the dentate line and no bleeding. Biopsies showed fragments of active colitis, ulcer and granulation tissue with no evidence of malignancy. Infectious workup showed positive chlamydia and was treated with doxycycline for 3 weeks with improvement of his symptoms. MRI of pelvis showed right sided intersphincteric perianal fistula and seton was placed. Flexible sigmoidoscopy was done a few weeks later with significant improvement of proctitis.
Discussion: The diagnosis of rectal LGV is usually delayed because of lack of classical symptoms of other etiologies of proctitis. It is extremely important to identify LGV as early as possible because of its challenges in differentiating from IBD as well as rectal malignancy. Even endoscopy or histologic evaluation might not be enough to distinguish LGV infection with mucosal ulceration, cryptitis, crypt abscesses and granuloma formation commonly seen in both. Molecular testing of LGV-specific C. trachomatis DNA from rectal swab specimens can lead to early diagnosis but seldom done. There is always risk of complications like fissures, fistulas and unnecessary invasive testing done with delayed diagnosis. Hopefully this case will help to raise awareness among healthcare providers about the different etiologies of proctitis and presentations.
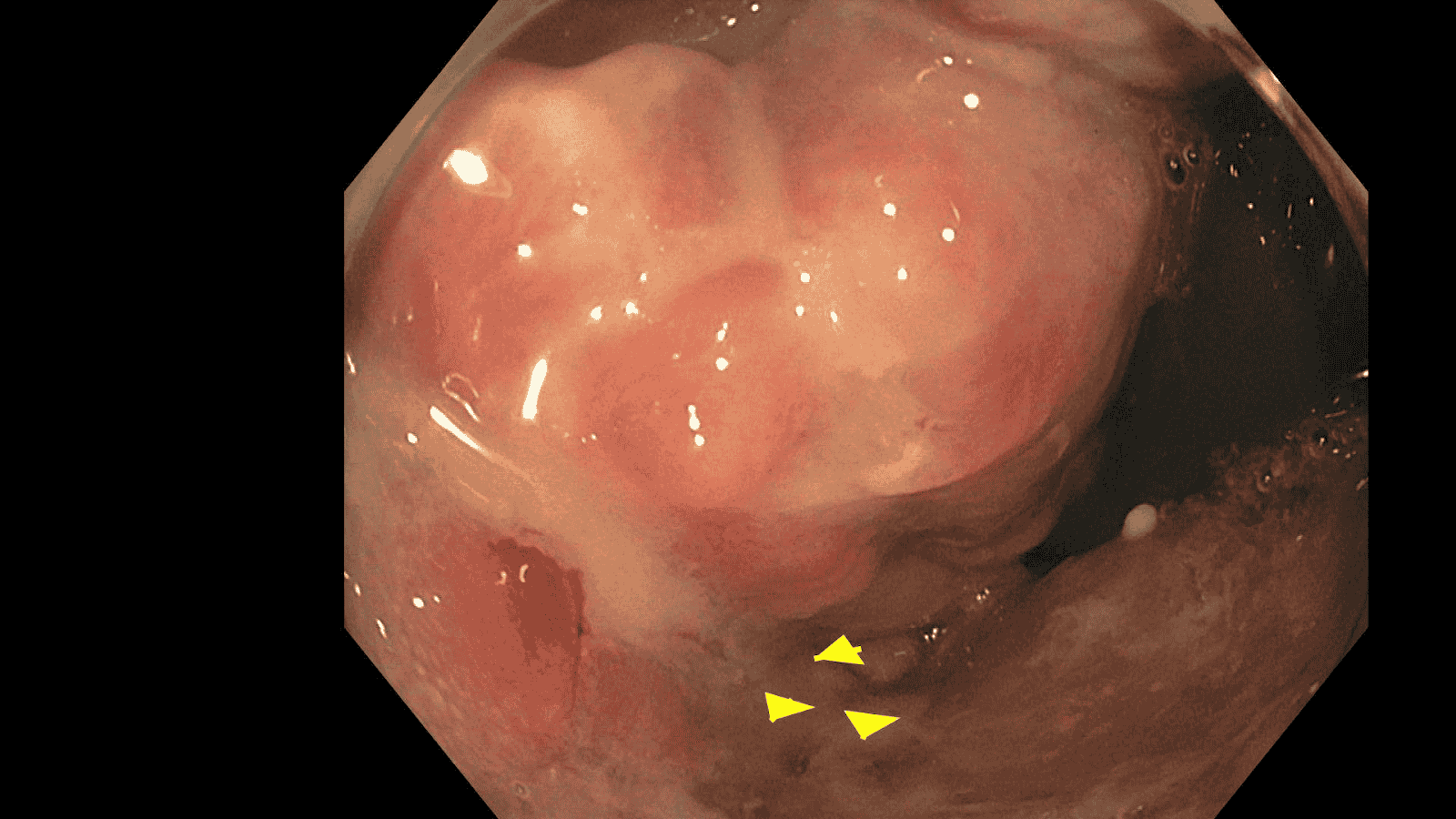
Figure: Figure 1
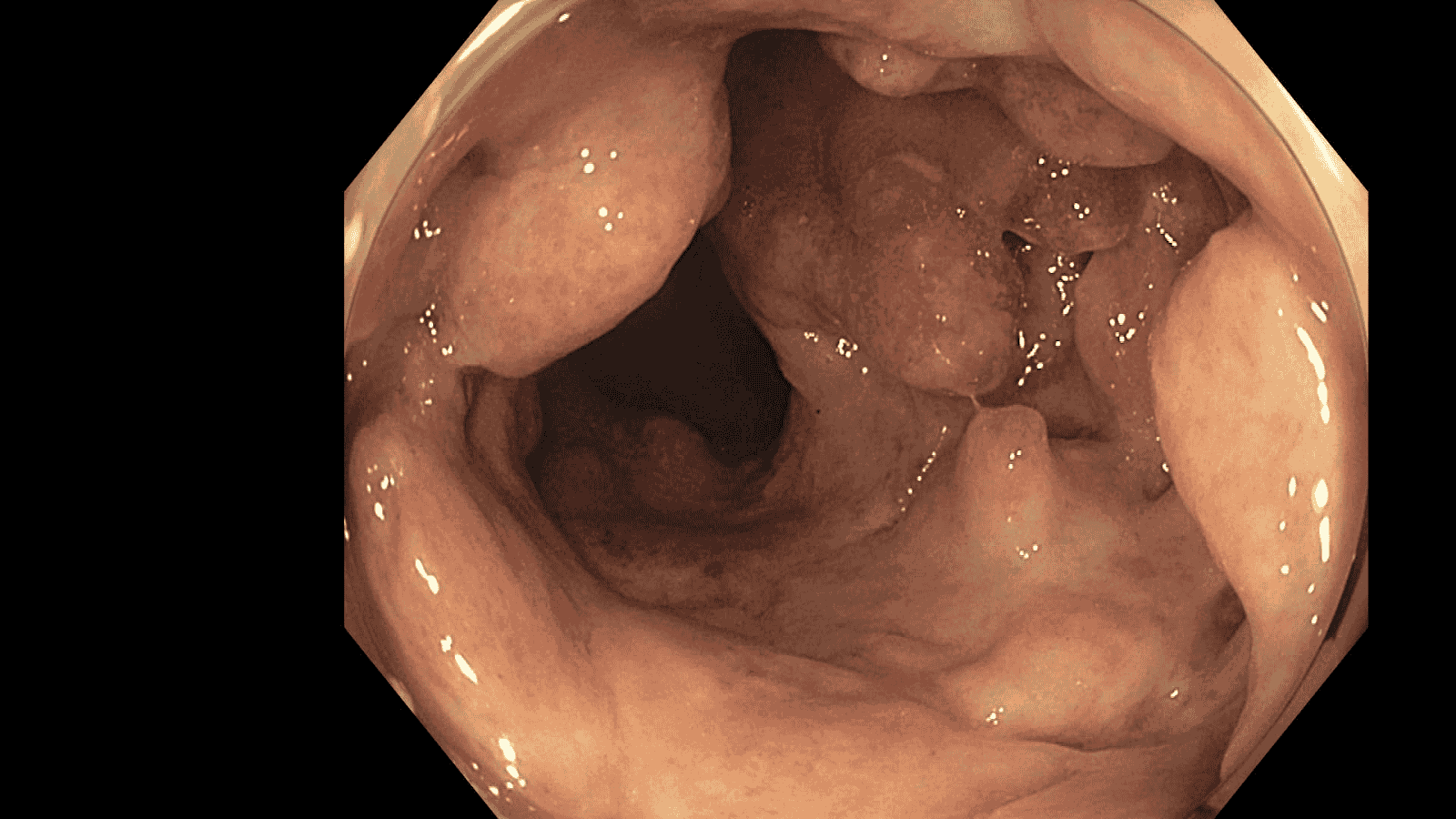
Figure: Figure 2
Disclosures:
Charitha Karanam Ramapathy indicated no relevant financial relationships.
Mahmoud Aryan indicated no relevant financial relationships.
Kirk Russ indicated no relevant financial relationships.
Charitha Karanam Ramapathy, MD1, Mahmoud Aryan, MD2, Kirk Russ, MD2. P3454 - Rectal LGV Imitating Cancer: A Diagnostic Pitfall in Anorectal Pathology, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
