Monday Poster Session
Category: Infections and Microbiome
P3441 - Adoption of New ICD-10 Codes for Microbial Overgrowth Syndromes: A Nationwide Analysis of Demographics and Treatment Trends
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SM
Sepideh Mehravar, MD (she/her/hers)
Cedars-Sinai Medical Center
Los Angeles, CA
Presenting Author(s)
Sepideh Mehravar, MD1, Gabriela Leite, PhD2, Parnian Naji, MD3, Ava Hosseini, MPH2, Ruchi Mathur, MD2, Mark Pimentel, MD, FACG1, Ali Rezaie, MD, MSc1
1Cedars-Sinai Medical Center, Los Angeles, CA; 2Cedars-Sinai Medical Center, West Hollywood, CA; 3University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: In October 2023, the World Health Organization introduced International Classification of Disease (ICD) codes for intestinal microbial overgrowth syndromes including small intestinal bacterial overgrowth (SIBO) and intestinal methanogen overgrowth (IMO) (Table 1). Consensus on optimal treatment strategies is still evolving and lack of large-scale data presents challenges in accurately diagnosing, managing, and understanding the underlying risk factors for SIBO and IMO. We aimed to assess the utilization of these codes in the US with a focus on demographic characteristics and treatment regimens.
Methods: This retrospective cohort study utilized data from the TriNetX database, which provides access to de-identified medical records from over 130 million patients across 94 healthcare organizations in the US. The study included patients with ICD-10 codes K63.8219, K63.8211, K63.8212, K63.829, and K63.822 (Table 1). Considering the introduction date of the new ICD10 codes, we analyzed data from Nov 2023 to May 2025. Demographics, including age, sex, ethnicity, and race, of each patient group, as well as the common treatment regimens used across these populations were analyzed.
Results: The most common ICD10 codes were “SIBO, unspecified” (K63.8219) and “IMO unspecified” (K63. 929). (Table 1) The SIBO cohort consisted of 16,327 patients with a mean age of 49±21 years (71.7% female). Regarding racial distribution, 76.1% were White, 7.1% were Black or African American, and 2.9% were Asian. Regarding ethnicity, 80.7% identified as non-Hispanic and 8.3% as Hispanic. Furthermore, 50% of the patients were treated with rifaximin, which was the most commonly used therapeutic approach. (Figure 1A) The IMO cohort consisted of 1,846 patients, with a mean age of 51±18 years (72.1% female). Regarding race, 80.5% were White, 6.2% were Black or African American, and 2.7% were Asian. 85.6% identified as non-Hispanic and 6.1% identified as Hispanic. Additionally, 54.9% of the patients were treated with rifaximin and neomycin as the prevailing treatment approach (Figure 1B).
Discussion: The widespread adoption of new diagnostic codes for microbial overgrowth is offering valuable insights into the burden, demographics, and treatment patterns of these patients on a national level. However, there is a pressing need to enhance education and awareness about the distinct subtypes of microbial overgrowth to promote accurate diagnosis and tailored treatment approaches.
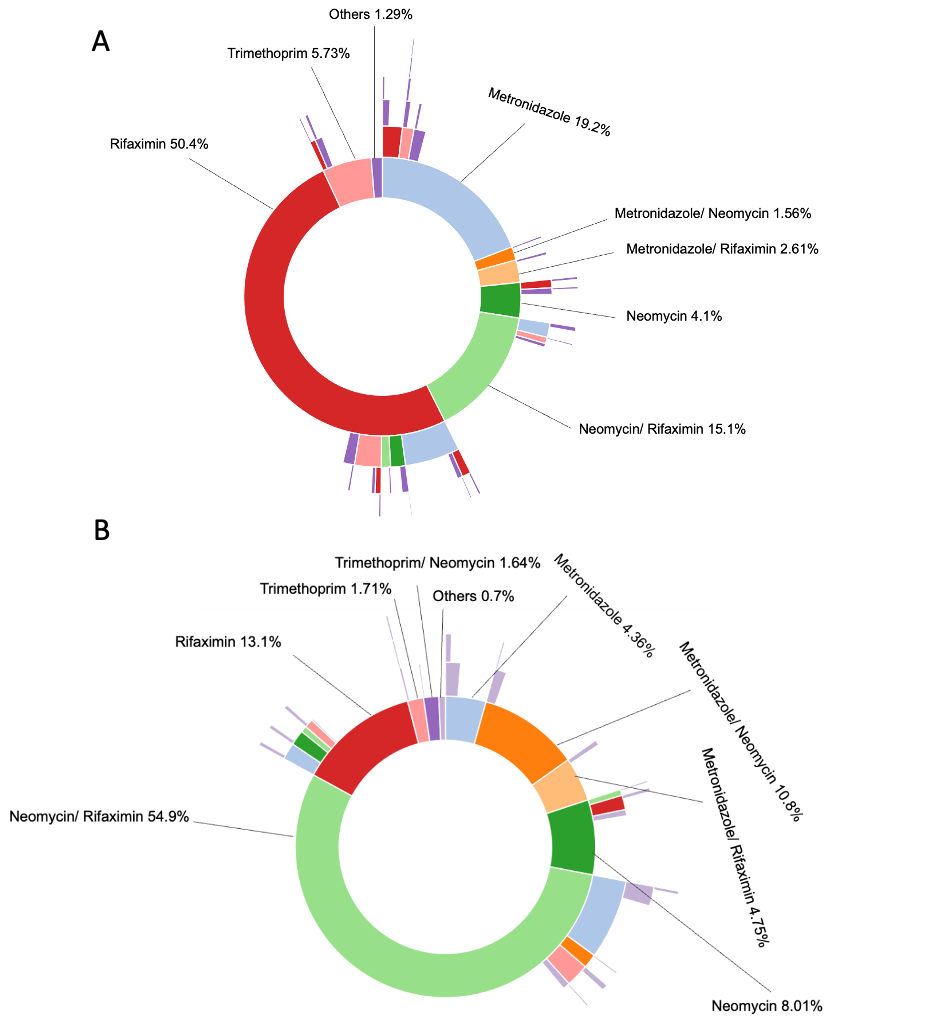
Figure: Figure1: Treatment patterns among patients with small intestinal overgrowth (panel A) and intestinal methanogen overgrowth (panel B).
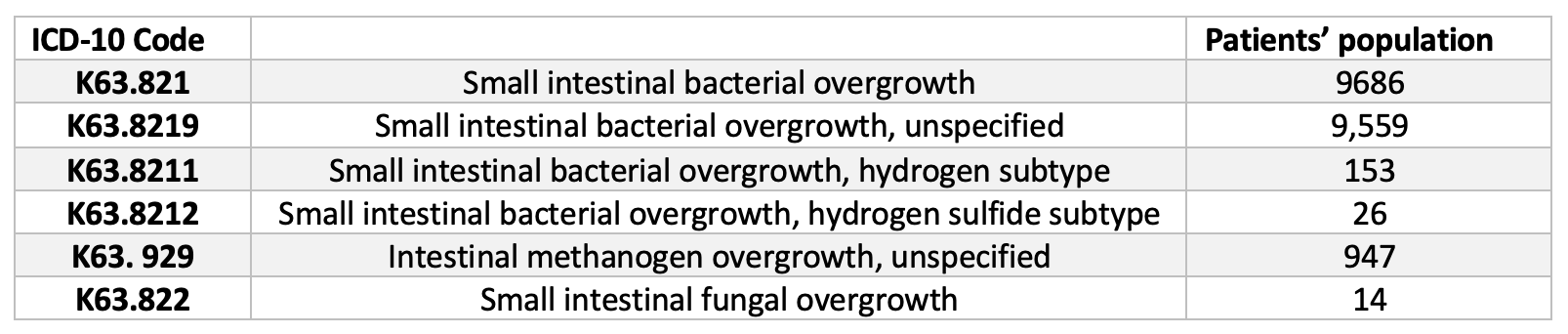
Figure: Table 1: ICD-10 Reference for Intestinal Overgrowth Subtypes
Disclosures:
Sepideh Mehravar indicated no relevant financial relationships.
Gabriela Leite indicated no relevant financial relationships.
Parnian Naji indicated no relevant financial relationships.
Ava Hosseini indicated no relevant financial relationships.
Ruchi Mathur: Gemelli Biotech – Royalties, Stock-privately held company. goodLFE – Stock-privately held company.
Mark Pimentel: Ardelyx – Consultant. Gemelli Biotech – Advisory Committee/Board Member, Royalties, Stock-privately held company. GoodLFE – Stock-privately held company. Salvo Health, Cylinder Health – Stock Options.
Ali Rezaie: Ardelyx, Blueprint Medicine and Salix Pharmaceuticals – Consultant. Gemelli Biotech, and Good LFE – Equity stake.
Sepideh Mehravar, MD1, Gabriela Leite, PhD2, Parnian Naji, MD3, Ava Hosseini, MPH2, Ruchi Mathur, MD2, Mark Pimentel, MD, FACG1, Ali Rezaie, MD, MSc1. P3441 - Adoption of New ICD-10 Codes for Microbial Overgrowth Syndromes: A Nationwide Analysis of Demographics and Treatment Trends, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cedars-Sinai Medical Center, Los Angeles, CA; 2Cedars-Sinai Medical Center, West Hollywood, CA; 3University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: In October 2023, the World Health Organization introduced International Classification of Disease (ICD) codes for intestinal microbial overgrowth syndromes including small intestinal bacterial overgrowth (SIBO) and intestinal methanogen overgrowth (IMO) (Table 1). Consensus on optimal treatment strategies is still evolving and lack of large-scale data presents challenges in accurately diagnosing, managing, and understanding the underlying risk factors for SIBO and IMO. We aimed to assess the utilization of these codes in the US with a focus on demographic characteristics and treatment regimens.
Methods: This retrospective cohort study utilized data from the TriNetX database, which provides access to de-identified medical records from over 130 million patients across 94 healthcare organizations in the US. The study included patients with ICD-10 codes K63.8219, K63.8211, K63.8212, K63.829, and K63.822 (Table 1). Considering the introduction date of the new ICD10 codes, we analyzed data from Nov 2023 to May 2025. Demographics, including age, sex, ethnicity, and race, of each patient group, as well as the common treatment regimens used across these populations were analyzed.
Results: The most common ICD10 codes were “SIBO, unspecified” (K63.8219) and “IMO unspecified” (K63. 929). (Table 1) The SIBO cohort consisted of 16,327 patients with a mean age of 49±21 years (71.7% female). Regarding racial distribution, 76.1% were White, 7.1% were Black or African American, and 2.9% were Asian. Regarding ethnicity, 80.7% identified as non-Hispanic and 8.3% as Hispanic. Furthermore, 50% of the patients were treated with rifaximin, which was the most commonly used therapeutic approach. (Figure 1A) The IMO cohort consisted of 1,846 patients, with a mean age of 51±18 years (72.1% female). Regarding race, 80.5% were White, 6.2% were Black or African American, and 2.7% were Asian. 85.6% identified as non-Hispanic and 6.1% identified as Hispanic. Additionally, 54.9% of the patients were treated with rifaximin and neomycin as the prevailing treatment approach (Figure 1B).
Discussion: The widespread adoption of new diagnostic codes for microbial overgrowth is offering valuable insights into the burden, demographics, and treatment patterns of these patients on a national level. However, there is a pressing need to enhance education and awareness about the distinct subtypes of microbial overgrowth to promote accurate diagnosis and tailored treatment approaches.
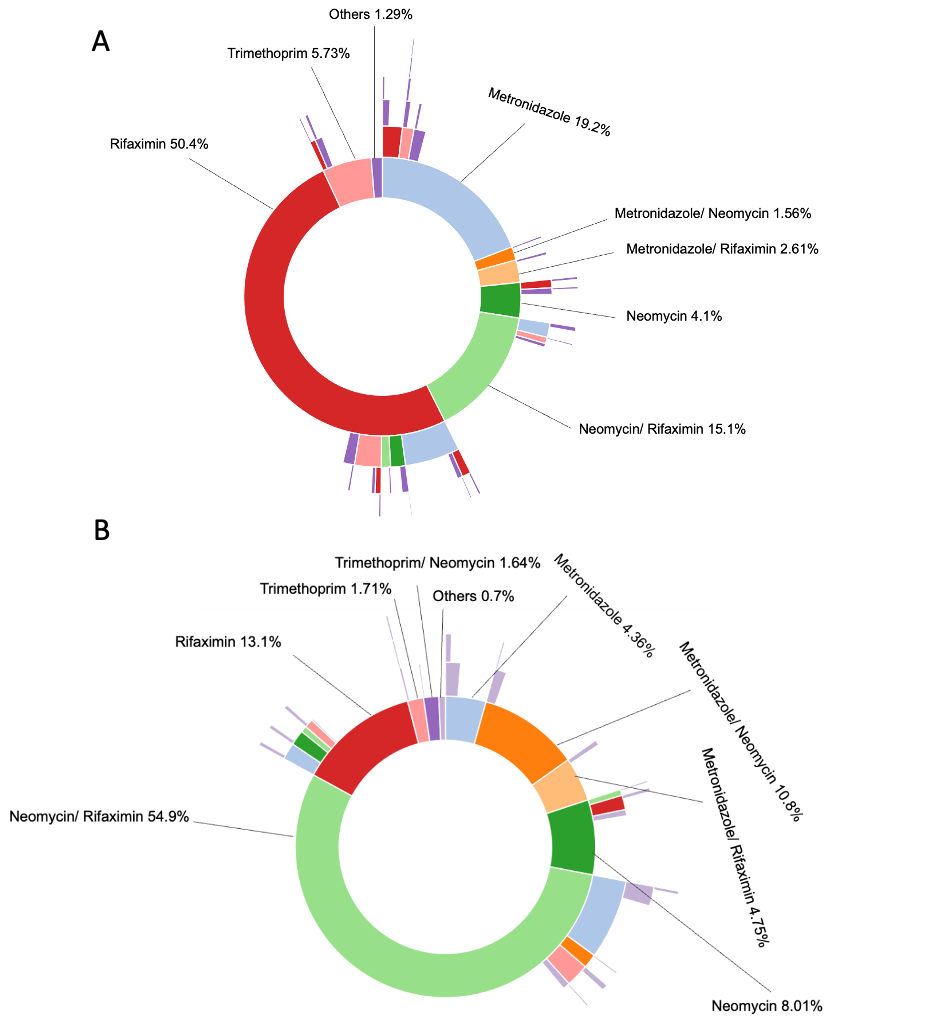
Figure: Figure1: Treatment patterns among patients with small intestinal overgrowth (panel A) and intestinal methanogen overgrowth (panel B).
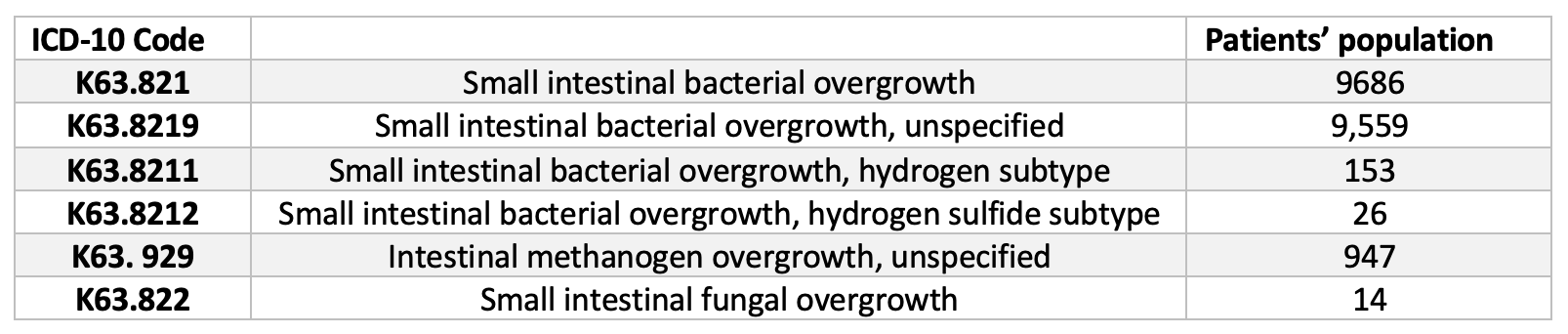
Figure: Table 1: ICD-10 Reference for Intestinal Overgrowth Subtypes
Disclosures:
Sepideh Mehravar indicated no relevant financial relationships.
Gabriela Leite indicated no relevant financial relationships.
Parnian Naji indicated no relevant financial relationships.
Ava Hosseini indicated no relevant financial relationships.
Ruchi Mathur: Gemelli Biotech – Royalties, Stock-privately held company. goodLFE – Stock-privately held company.
Mark Pimentel: Ardelyx – Consultant. Gemelli Biotech – Advisory Committee/Board Member, Royalties, Stock-privately held company. GoodLFE – Stock-privately held company. Salvo Health, Cylinder Health – Stock Options.
Ali Rezaie: Ardelyx, Blueprint Medicine and Salix Pharmaceuticals – Consultant. Gemelli Biotech, and Good LFE – Equity stake.
Sepideh Mehravar, MD1, Gabriela Leite, PhD2, Parnian Naji, MD3, Ava Hosseini, MPH2, Ruchi Mathur, MD2, Mark Pimentel, MD, FACG1, Ali Rezaie, MD, MSc1. P3441 - Adoption of New ICD-10 Codes for Microbial Overgrowth Syndromes: A Nationwide Analysis of Demographics and Treatment Trends, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
