Monday Poster Session
Category: Infections and Microbiome
P3439 - Microbial Profiling of Perianal Fistulas in Crohn’s Disease Across Anatomical Sites
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Samuel Guo Pan, MD (he/him/his)
Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Samuel Guo. Pan, MD1, Hunter R. Moran, 1, Marko Mrdjen, PhD1, Jeremiah Faith, PhD1, Sergey Khaitov, MD1, Bari Giller, PA-C2, Serre-Yu Wong, MD, PhD1
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai Hospital, New York, NY
Introduction: Perianal fistulas are abnormal connections between the anorectum and perianal skin and occur in up to one third of patients with Crohn’s disease (CD), termed perianal fistulizing Crohn’s disease (PFCD). The microbiome of perianal fistulas remains poorly defined in adults with PFCD. We aim to characterize the microbiome composition of the perianal skin, fistula tract, and internal orifice, as well as monitor changes over time in response to CD therapy.
Methods: We conducted a longitudinal, prospective observational study of 14 adult patients with a perianal fistula, with or without CD, at a single center. Baseline fistula characteristics were determined by pelvic MRI or MRE. Specimens were collected from three sites of the fistula tunnels: (1) swab of perianal skin at the external opening, (2) brushing of the fistula tract, and (3) brushing of the internal orifice. Each patient contributed samples at two or three timepoints, yielding 33 total sampling timepoints. Microbiome composition was determined using 16S rRNA gene sequencing and processed by the DADA2 pipeline in R. Shannon diversity and the principal component analysis were calculated using the unfiltered relative abundance matrix and measured with Bray-Curtis similarity using the Phyloseq package in R.
Results: Among the 14 patients, 86% had CD, 71% were male, and 64% were Caucasian. All PFCD patients had prior advanced CD therapy. At the time of sampling, 91% of sampling timepoints occurred while patients were on advanced CD therapy, 30% while on antibiotics in the past 30 days, and 18% while a diverting ostomy was present. The most common types of fistulas were transphincteric (53%) and intersphincteric (27%).
Microbiome analysis revealed distinct clustering by anatomical site, with closer clustering between the fistula tract and internal orifice microbiomes. The perianal skin had higher Corynbacterium and lower Streptococcus relative abundances compared to the fistula tract and internal orifice. The internal orifice had higher Finegoldia and lower Corynbacterium relative abundances compared to the fistula tract.
Discussion: The microbial signature of the fistula microbiome is distinct across the perianal skin, fistula tract, and internal orifice. The internal orifice and fistula tract microbiomes were more similar to each other than to the perianal skin microbiome. A future direction of the study is to evaluate the longitudinal impact of CD treatment on the perianal fistula microbiome composition.
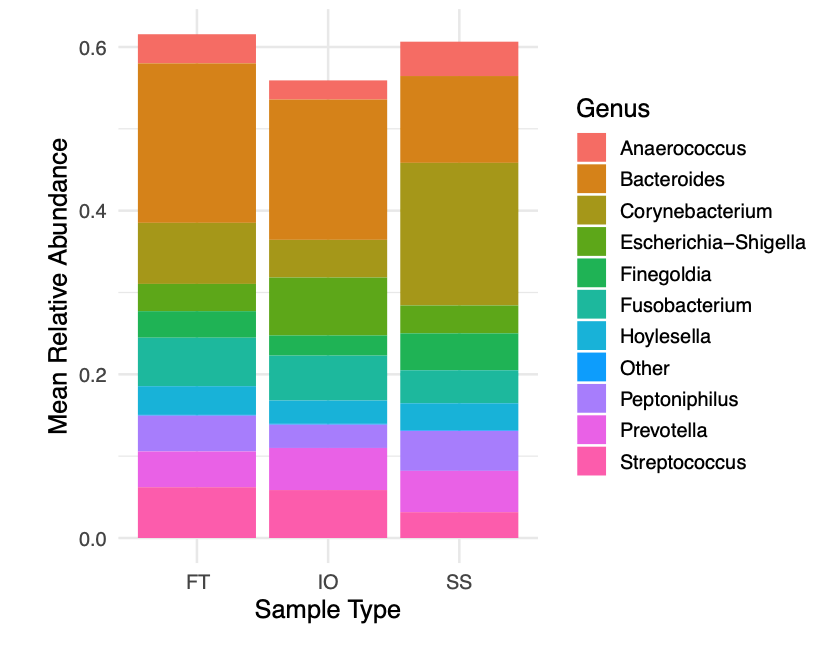
Figure: Figure 1. PCoA by sample type
Beta-diversity, determined by principal coordinates analysis (Bray-Curtis) and measured using the Phyloseq package in R. Fistula tract (FT), internal orifice (IO), and perianal skin swab (SS).
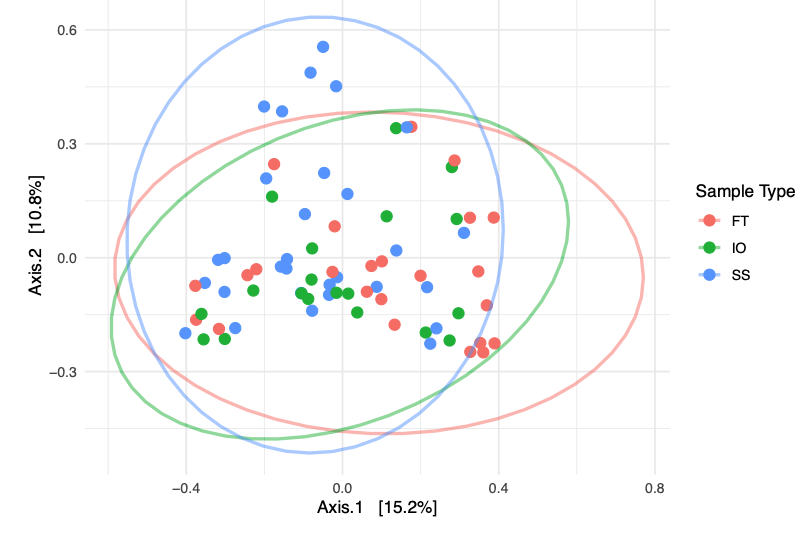
Figure: Figure 2. Top 10 genera abundances by sample type
Microbiome composition was determined using 16S rRNA gene sequencing. Fistula tract (FT), internal orifice (IO), and perianal skin swab (SS).
Disclosures:
Samuel Pan indicated no relevant financial relationships.
Hunter Moran indicated no relevant financial relationships.
Marko Mrdjen indicated no relevant financial relationships.
Jeremiah Faith: Genfit – Consultant. Janssen Research & Development – Grant/Research Support. Vedanta Biosciences – Consultant.
Sergey Khaitov indicated no relevant financial relationships.
Bari Giller indicated no relevant financial relationships.
Serre-Yu Wong: BMS – Advisory Committee/Board Member. Eli Lilly and Company – Grant/Research Support. Takeda/Trinetx – Grant/Research Support.
Samuel Guo. Pan, MD1, Hunter R. Moran, 1, Marko Mrdjen, PhD1, Jeremiah Faith, PhD1, Sergey Khaitov, MD1, Bari Giller, PA-C2, Serre-Yu Wong, MD, PhD1. P3439 - Microbial Profiling of Perianal Fistulas in Crohn’s Disease Across Anatomical Sites, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai Hospital, New York, NY
Introduction: Perianal fistulas are abnormal connections between the anorectum and perianal skin and occur in up to one third of patients with Crohn’s disease (CD), termed perianal fistulizing Crohn’s disease (PFCD). The microbiome of perianal fistulas remains poorly defined in adults with PFCD. We aim to characterize the microbiome composition of the perianal skin, fistula tract, and internal orifice, as well as monitor changes over time in response to CD therapy.
Methods: We conducted a longitudinal, prospective observational study of 14 adult patients with a perianal fistula, with or without CD, at a single center. Baseline fistula characteristics were determined by pelvic MRI or MRE. Specimens were collected from three sites of the fistula tunnels: (1) swab of perianal skin at the external opening, (2) brushing of the fistula tract, and (3) brushing of the internal orifice. Each patient contributed samples at two or three timepoints, yielding 33 total sampling timepoints. Microbiome composition was determined using 16S rRNA gene sequencing and processed by the DADA2 pipeline in R. Shannon diversity and the principal component analysis were calculated using the unfiltered relative abundance matrix and measured with Bray-Curtis similarity using the Phyloseq package in R.
Results: Among the 14 patients, 86% had CD, 71% were male, and 64% were Caucasian. All PFCD patients had prior advanced CD therapy. At the time of sampling, 91% of sampling timepoints occurred while patients were on advanced CD therapy, 30% while on antibiotics in the past 30 days, and 18% while a diverting ostomy was present. The most common types of fistulas were transphincteric (53%) and intersphincteric (27%).
Microbiome analysis revealed distinct clustering by anatomical site, with closer clustering between the fistula tract and internal orifice microbiomes. The perianal skin had higher Corynbacterium and lower Streptococcus relative abundances compared to the fistula tract and internal orifice. The internal orifice had higher Finegoldia and lower Corynbacterium relative abundances compared to the fistula tract.
Discussion: The microbial signature of the fistula microbiome is distinct across the perianal skin, fistula tract, and internal orifice. The internal orifice and fistula tract microbiomes were more similar to each other than to the perianal skin microbiome. A future direction of the study is to evaluate the longitudinal impact of CD treatment on the perianal fistula microbiome composition.
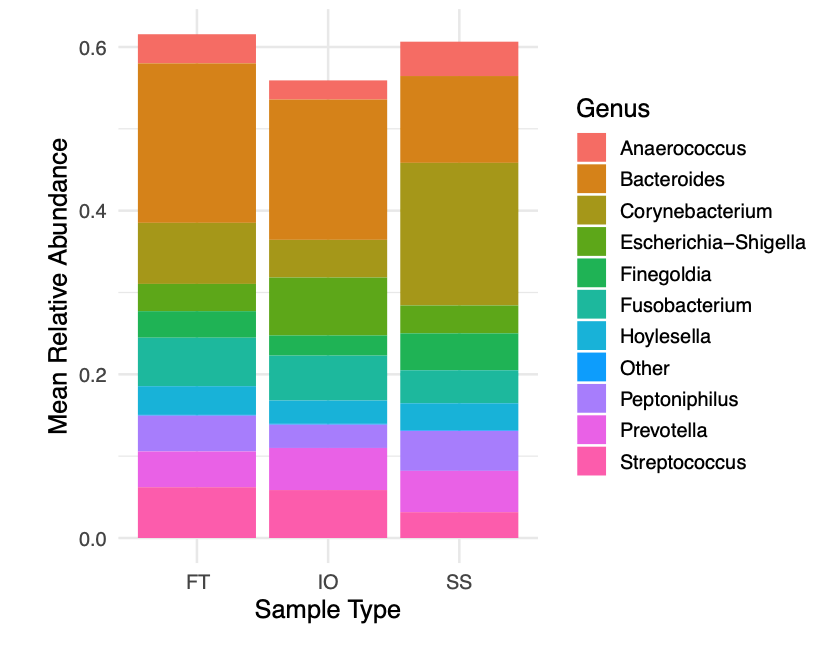
Figure: Figure 1. PCoA by sample type
Beta-diversity, determined by principal coordinates analysis (Bray-Curtis) and measured using the Phyloseq package in R. Fistula tract (FT), internal orifice (IO), and perianal skin swab (SS).
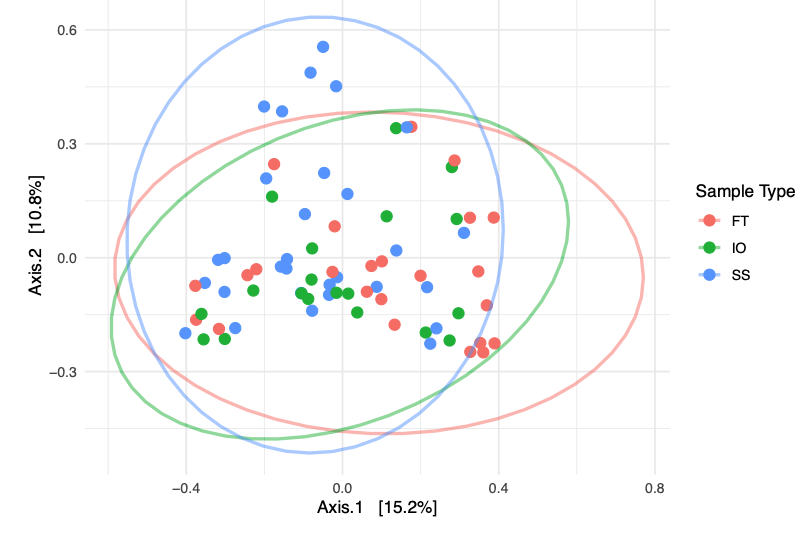
Figure: Figure 2. Top 10 genera abundances by sample type
Microbiome composition was determined using 16S rRNA gene sequencing. Fistula tract (FT), internal orifice (IO), and perianal skin swab (SS).
Disclosures:
Samuel Pan indicated no relevant financial relationships.
Hunter Moran indicated no relevant financial relationships.
Marko Mrdjen indicated no relevant financial relationships.
Jeremiah Faith: Genfit – Consultant. Janssen Research & Development – Grant/Research Support. Vedanta Biosciences – Consultant.
Sergey Khaitov indicated no relevant financial relationships.
Bari Giller indicated no relevant financial relationships.
Serre-Yu Wong: BMS – Advisory Committee/Board Member. Eli Lilly and Company – Grant/Research Support. Takeda/Trinetx – Grant/Research Support.
Samuel Guo. Pan, MD1, Hunter R. Moran, 1, Marko Mrdjen, PhD1, Jeremiah Faith, PhD1, Sergey Khaitov, MD1, Bari Giller, PA-C2, Serre-Yu Wong, MD, PhD1. P3439 - Microbial Profiling of Perianal Fistulas in Crohn’s Disease Across Anatomical Sites, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
