Monday Poster Session
Category: Interventional Endoscopy
P3509 - Outcomes of Endoscopic Cystogastrostomy Using Lumen-Apposing Metal Stents: A Multi-Institutional Real-World Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ashujot K. Dang, MD
University of California Riverside School of Medicine
Riverside, CA
Presenting Author(s)
Ashujot K. Dang, MD1, Vikash Kumar, MD2, Aalam Sohal, MD2, Dalbir Sandhu, MD2
1University of California Riverside School of Medicine, Riverside, CA; 2Creighton University School of Medicine, Phoenix, AZ
Introduction: Pancreatic fluid collections (PFCs) often require drainage when symptomatic or infected. Endoscopic cystogastrostomy using lumen-apposing metal stents (LAMS) has become the preferred minimally invasive approach due to its high technical success and favorable safety profile. While prior studies have demonstrated efficacy in small cohorts or single-center settings, comprehensive multi-institutional data remain limited. This study provides a comprehensive, real-world evaluation of short-term clinical outcomes following LAMS placement across a diverse network of U.S. healthcare institutions.
Methods: We performed a retrospective cohort study using the TriNetX US Collaborative Network, comprising 69 healthcare organizations. Adult patients (≥18 years) with pancreatic cysts or pseudocysts (ICD-10: K86.2, K86.3) who underwent endoscopic transmural drainage with a LAMS (CPT: 43240) were included. The index event was defined as the first documented stent placement. Outcomes were assessed from Day 1 to Day 90 post-procedure and included bleeding, readmission, shock, infection, mortality, and the need for interventional radiology (IR) or surgical reintervention. Patients with pre-existing events were excluded from relevant outcome analyses. Kaplan-Meier survival curves and risk analyses were conducted.
Results: A total of 5,793 patients met inclusion criteria, with a median follow-up of 90 days. The 90-day cumulative incidence of complications was as follows: bleeding (0.8%), shock (3.2%), infection/sepsis (0.8%), and mortality (4.0%). Among 2,115 patients eligible for readmission analysis, the 90-day readmission rate was 29.3%. IR reintervention was required in 8.0% of patients, and 2.1% underwent surgical reintervention. Kaplan-Meier analysis demonstrated high 90-day survival probabilities across outcomes—95.7% for overall survival and 91.7% for freedom from IR reintervention. Relative 90-day risk estimates, used as proxies for hazard ratios, are shown in the accompanying figure.
Discussion: In this large multi-institutional study, endoscopic drainage of PFCs using LAMS was associated with low rates of bleeding, infection, and mortality, along with high 90-day survival and relatively infrequent need for reintervention. These findings support LAMS as a safe and effective first-line approach for managing symptomatic or infected PFCs in routine practice. Prospective studies are needed to optimize long-term outcomes and patient selection.
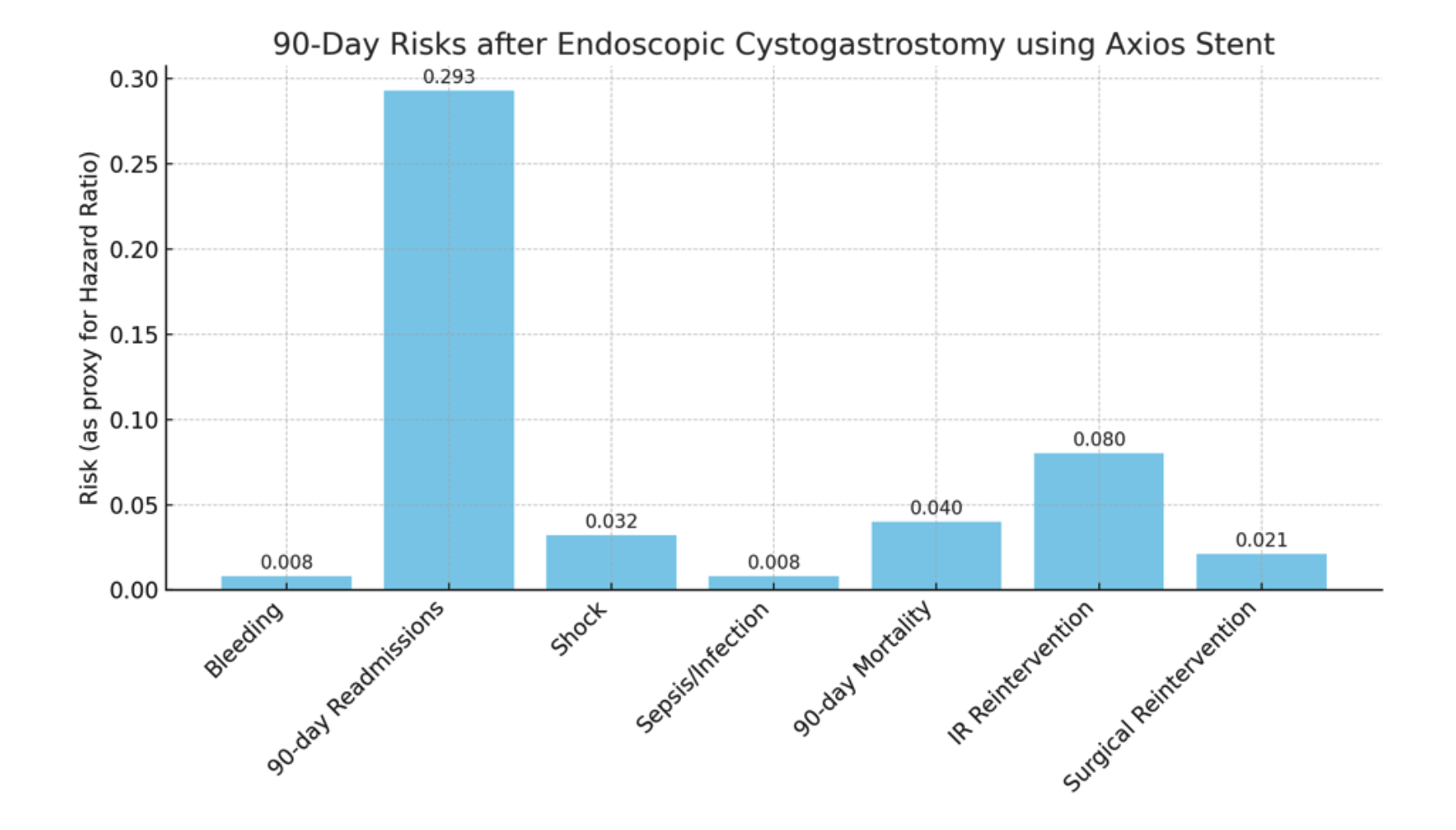
Figure: 90-day risks for outcomes after LAMS like axios placement in patients with pancreatic fluid collections
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Dalbir Sandhu indicated no relevant financial relationships.
Ashujot K. Dang, MD1, Vikash Kumar, MD2, Aalam Sohal, MD2, Dalbir Sandhu, MD2. P3509 - Outcomes of Endoscopic Cystogastrostomy Using Lumen-Apposing Metal Stents: A Multi-Institutional Real-World Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Riverside School of Medicine, Riverside, CA; 2Creighton University School of Medicine, Phoenix, AZ
Introduction: Pancreatic fluid collections (PFCs) often require drainage when symptomatic or infected. Endoscopic cystogastrostomy using lumen-apposing metal stents (LAMS) has become the preferred minimally invasive approach due to its high technical success and favorable safety profile. While prior studies have demonstrated efficacy in small cohorts or single-center settings, comprehensive multi-institutional data remain limited. This study provides a comprehensive, real-world evaluation of short-term clinical outcomes following LAMS placement across a diverse network of U.S. healthcare institutions.
Methods: We performed a retrospective cohort study using the TriNetX US Collaborative Network, comprising 69 healthcare organizations. Adult patients (≥18 years) with pancreatic cysts or pseudocysts (ICD-10: K86.2, K86.3) who underwent endoscopic transmural drainage with a LAMS (CPT: 43240) were included. The index event was defined as the first documented stent placement. Outcomes were assessed from Day 1 to Day 90 post-procedure and included bleeding, readmission, shock, infection, mortality, and the need for interventional radiology (IR) or surgical reintervention. Patients with pre-existing events were excluded from relevant outcome analyses. Kaplan-Meier survival curves and risk analyses were conducted.
Results: A total of 5,793 patients met inclusion criteria, with a median follow-up of 90 days. The 90-day cumulative incidence of complications was as follows: bleeding (0.8%), shock (3.2%), infection/sepsis (0.8%), and mortality (4.0%). Among 2,115 patients eligible for readmission analysis, the 90-day readmission rate was 29.3%. IR reintervention was required in 8.0% of patients, and 2.1% underwent surgical reintervention. Kaplan-Meier analysis demonstrated high 90-day survival probabilities across outcomes—95.7% for overall survival and 91.7% for freedom from IR reintervention. Relative 90-day risk estimates, used as proxies for hazard ratios, are shown in the accompanying figure.
Discussion: In this large multi-institutional study, endoscopic drainage of PFCs using LAMS was associated with low rates of bleeding, infection, and mortality, along with high 90-day survival and relatively infrequent need for reintervention. These findings support LAMS as a safe and effective first-line approach for managing symptomatic or infected PFCs in routine practice. Prospective studies are needed to optimize long-term outcomes and patient selection.
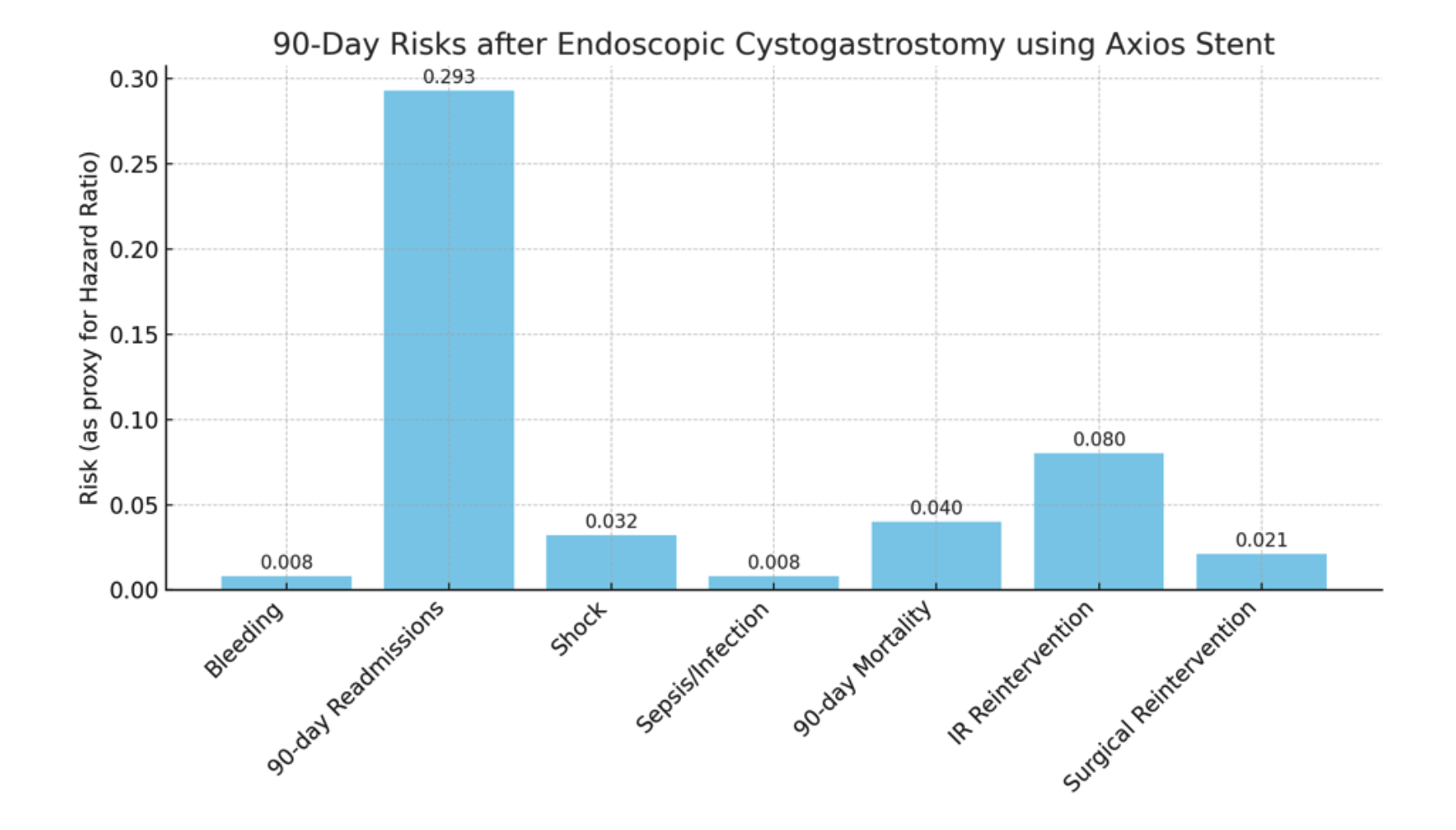
Figure: 90-day risks for outcomes after LAMS like axios placement in patients with pancreatic fluid collections
Disclosures:
Ashujot Dang indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Aalam Sohal indicated no relevant financial relationships.
Dalbir Sandhu indicated no relevant financial relationships.
Ashujot K. Dang, MD1, Vikash Kumar, MD2, Aalam Sohal, MD2, Dalbir Sandhu, MD2. P3509 - Outcomes of Endoscopic Cystogastrostomy Using Lumen-Apposing Metal Stents: A Multi-Institutional Real-World Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
