Monday Poster Session
Category: Interventional Endoscopy
P3588 - Minimally Invasive Resolution of Necrotizing Pancreatitis and Biliary Fistula via Sequential Endoscopic Interventions
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ali Shaat, MD
Lahey Hospital and Medical Center
Burlington, MA
Presenting Author(s)
Ali Shaat, MD1, Ishan Antony, MD2, Christopher Ward, MD1
1Lahey Hospital and Medical Center, Burlington, MA; 2Beth Israel Lahey Health, Burlington, MA
Introduction: Complications arising from acute necrotizing pancreatitis, such as walled-off necrosis (WON) and biliary fistula formation, present significant clinical challenges. This case highlights the role of advanced endoscopic interventions in the management of severe post-procedural pancreatitis complications in a patient following ampullectomy.
Case Description/
Methods: A 48-year-old man with a history of gastroesophageal reflux disease and hyperlipidemia was found to have a 3 cm multilobulated periampullary adenoma during a routine upper endoscopy. He underwent an endoscopic ultrasound-guided (EUS) endoscopic retrograde cholangiopancreatography (ERCP) with resection of the ampullary adenoma and closure of a mucosal defect with endoscopic clips. Post-procedure, he developed acute interstitial pancreatitis with cholestatic transaminases, and a follow-up ERCP demonstrated biliary obstruction, which was managed with the placement of a plastic stent in the distal common bile duct (CBD). He subsequently developed sepsis, and abdominal imaging revealed necrotizing pancreatitis with gas formation and a WON in the lesser sac. He was also found to have fistulous tracts from both the common hepatic duct (CHD) and the duodenal bulb communicating with the necrotic collection. He underwent a series of advanced endoscopic procedures for source control and drainage. An ERCP was done, during which a left hepatic duct stent was placed, and a double-pigtail stent was placed between the collection and the duodenal bulb. Subsequently, two fully covered self-expanding metal stents were placed in the CHD and CBD to ensure biliary decompression. This was followed by the placement of a lumen-apposing metal stent (LAMS) into the duodenal fistula to create a cystoduodenostomy. Over the ensuing weeks, he underwent serial endoscopic necrosectomies through the LAMS, resulting in significant clinical and radiologic improvement. Final follow-up endoscopy and imaging confirmed complete resolution of the WON and closure of the biliary fistula. The LAMS was removed, and a permanent double-pigtail catheter was placed.
Discussion: The use of EUS-guided LAMS placement for cystoduodenostomy, combined with targeted biliary stenting and endoscopic necrosectomy, provided a definitive and minimally invasive alternative to surgical intervention. This case demonstrates the efficacy of a step-up endoscopic approach in managing complex pancreatitis-related complications.
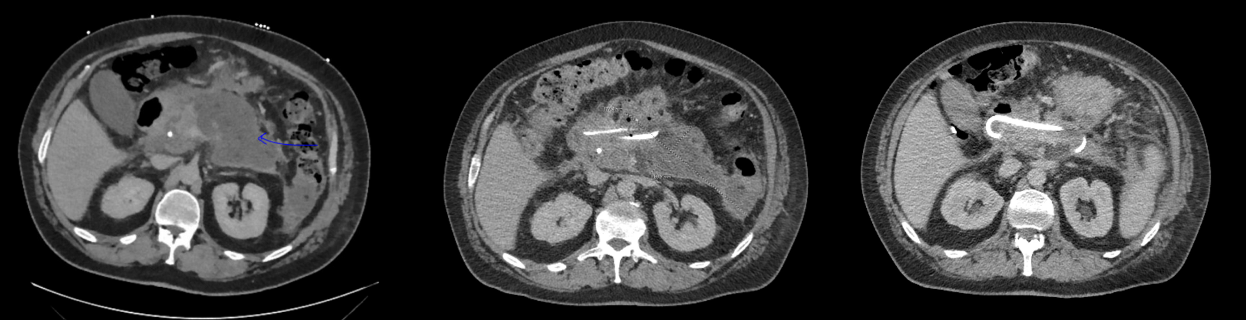
Figure: Computed tomography (CT) of the abdomen showing progression from walled-off necrosis (WON) to resolution following serial endoscopic interventions, including placement of double-pigtail stents (images shown left to right).
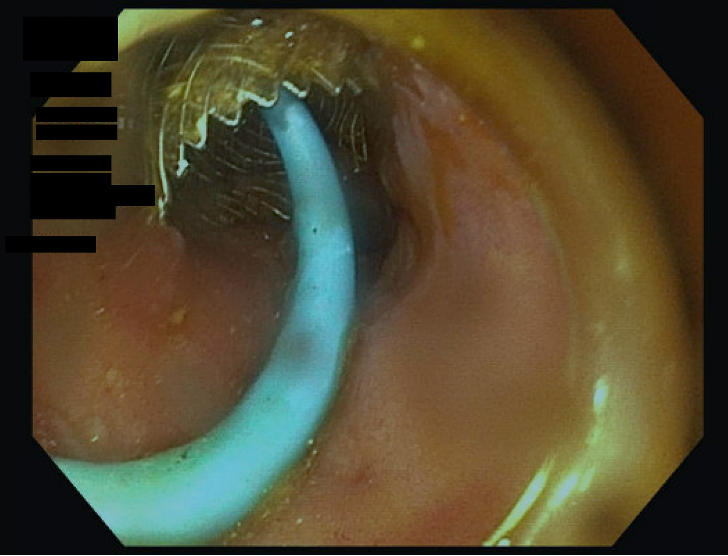
Figure: Cystoduodenostomy performed using a 20 × 10 mm LAMS (AXIOS) with an internal double-pigtail stent deployed through the LAMS.
Disclosures:
Ali Shaat indicated no relevant financial relationships.
Ishan Antony indicated no relevant financial relationships.
Christopher Ward indicated no relevant financial relationships.
Ali Shaat, MD1, Ishan Antony, MD2, Christopher Ward, MD1. P3588 - Minimally Invasive Resolution of Necrotizing Pancreatitis and Biliary Fistula via Sequential Endoscopic Interventions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Lahey Hospital and Medical Center, Burlington, MA; 2Beth Israel Lahey Health, Burlington, MA
Introduction: Complications arising from acute necrotizing pancreatitis, such as walled-off necrosis (WON) and biliary fistula formation, present significant clinical challenges. This case highlights the role of advanced endoscopic interventions in the management of severe post-procedural pancreatitis complications in a patient following ampullectomy.
Case Description/
Methods: A 48-year-old man with a history of gastroesophageal reflux disease and hyperlipidemia was found to have a 3 cm multilobulated periampullary adenoma during a routine upper endoscopy. He underwent an endoscopic ultrasound-guided (EUS) endoscopic retrograde cholangiopancreatography (ERCP) with resection of the ampullary adenoma and closure of a mucosal defect with endoscopic clips. Post-procedure, he developed acute interstitial pancreatitis with cholestatic transaminases, and a follow-up ERCP demonstrated biliary obstruction, which was managed with the placement of a plastic stent in the distal common bile duct (CBD). He subsequently developed sepsis, and abdominal imaging revealed necrotizing pancreatitis with gas formation and a WON in the lesser sac. He was also found to have fistulous tracts from both the common hepatic duct (CHD) and the duodenal bulb communicating with the necrotic collection. He underwent a series of advanced endoscopic procedures for source control and drainage. An ERCP was done, during which a left hepatic duct stent was placed, and a double-pigtail stent was placed between the collection and the duodenal bulb. Subsequently, two fully covered self-expanding metal stents were placed in the CHD and CBD to ensure biliary decompression. This was followed by the placement of a lumen-apposing metal stent (LAMS) into the duodenal fistula to create a cystoduodenostomy. Over the ensuing weeks, he underwent serial endoscopic necrosectomies through the LAMS, resulting in significant clinical and radiologic improvement. Final follow-up endoscopy and imaging confirmed complete resolution of the WON and closure of the biliary fistula. The LAMS was removed, and a permanent double-pigtail catheter was placed.
Discussion: The use of EUS-guided LAMS placement for cystoduodenostomy, combined with targeted biliary stenting and endoscopic necrosectomy, provided a definitive and minimally invasive alternative to surgical intervention. This case demonstrates the efficacy of a step-up endoscopic approach in managing complex pancreatitis-related complications.
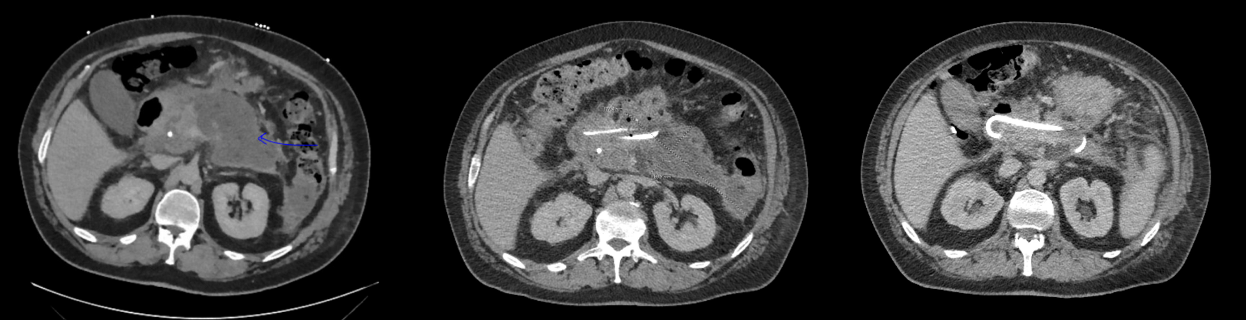
Figure: Computed tomography (CT) of the abdomen showing progression from walled-off necrosis (WON) to resolution following serial endoscopic interventions, including placement of double-pigtail stents (images shown left to right).
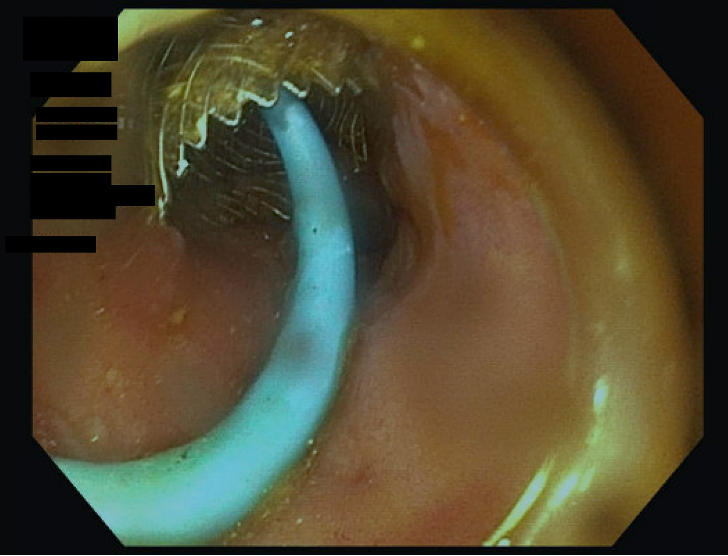
Figure: Cystoduodenostomy performed using a 20 × 10 mm LAMS (AXIOS) with an internal double-pigtail stent deployed through the LAMS.
Disclosures:
Ali Shaat indicated no relevant financial relationships.
Ishan Antony indicated no relevant financial relationships.
Christopher Ward indicated no relevant financial relationships.
Ali Shaat, MD1, Ishan Antony, MD2, Christopher Ward, MD1. P3588 - Minimally Invasive Resolution of Necrotizing Pancreatitis and Biliary Fistula via Sequential Endoscopic Interventions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
