Monday Poster Session
Category: Interventional Endoscopy
P3582 - Endoscopic Ultrasound-Guided Luminal Apposing Metal Stent Drainage of a Post-Splenectomy Abscess: A Case Report
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nikita Garg, MD (she/her/hers)
Geisinger Wyoming Valley Medical Center
Wilkes-Barre, PA
Presenting Author(s)
Nikita Garg, MD1, Danial Nadeem, MD1, Tushar Abhinav, MD2, Mutshipay Christian Mpoy, MD3, Kishore Kumar, MD4, Nihaal Karnik, MD1
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2The Wright Center for Graduate Medical Education, Wilkes-Barre, PA; 3Geisinger Health System, Wilkes-Barre, PA; 4Geisinger Community Medical Center, Scranton, PA
Introduction: Splenic abscess is a rare but potentially life-threatening condition. Endoscopic ultrasound (EUS)-guided drainage with lumen-apposing metal stents (LAMS) is an emerging minimally invasive approach for patients deemed poor surgical candidates, however, reported cases remain limited. We present a case of a post-splenectomy splenic bed abscess successfully managed with EUS-guided transmural drainage utilizing a LAMS and coaxial double-pigtail stent.
Case Description/
Methods: A 21-year-old male with recent gunshot injury to the left flank underwent exploratory laparotomy with splenectomy and diaphragm repair. Two weeks postoperatively, he presented with fever and worsening abdominal pain. Imaging revealed a 4.1 x 5.8 cm rim-enhancing fluid collection in the splenectomy bed, consistent with an abscess in the post-splenectomy cavity. The collection was closely adjacent to the gastric fundus and diaphragm. Due to the high location of the abscess and lack of a safe percutaneous window, interventional radiology deemed image-guided drainage unfeasible. Given the anatomic proximity of the collection to the stomach, EUS was performed. A well-defined hypoechoic abscess was identified adjacent to the gastric fundus. Following doppler evaluation to exclude intervening vasculature, a 10 mm × 10 mm LAMS (AXIOS, Boston Scientific) was deployed under EUS and fluoroscopic guidance using direct puncture with pure cutting current. Immediate purulent drainage confirmed successful cavity access. An abscessogram demonstrated proper positioning and contrast flow. A 10 Fr × 3 cm double-pigtail plastic stent was placed coaxially through the LAMS to prevent stent occlusion and migration. The procedure was well tolerated with no complications. Follow up CT at 6 weeks demonstrated complete resolution of the abscess with the LAMS still in place. The stent was safely removed one week later.
Discussion: Although EUS-guided drainage is well established for pancreatic fluid collections, its application in non-pancreatic abscesses—particularly splenic bed collections—remains rare. This case highlights the feasibility and safety of EUS-guided transmural drainage using a LAMS in a post-splenectomy patient, where percutaneous access was not possible. Internal drainage via EUS offered a minimally invasive alternative to surgery, with successful infection resolution and no procedural complications. This approach may expand the therapeutic arsenal for managing deep-seated intra-abdominal abscesses in high-risk surgical patients.
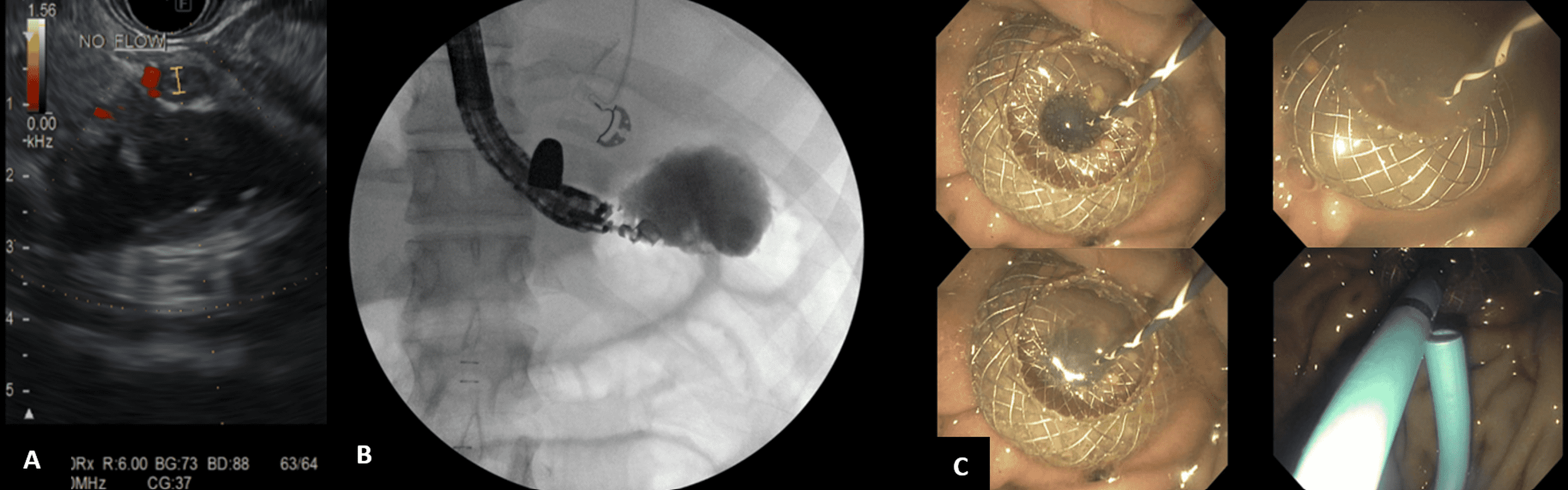
Figure: Figure.1 Axial (a) and coronal (b) contrast enhanced CT through the abdomen on 3/22/2025 demonstrating a 4 x 6 cm abscess (arrow) within the splenectomy bed (solid arrow) abutting the stomach (*) posteriorly. Bullet fragment (dashed arrow) to the left of the T11 vertebral body on the coronal. Contrast enhanced axial (c) and coronal (d) CT through the abdomen on 5/23/2025 status post upper endoscopic ultrasound (EUS) guided transmural drainage via the gastric fundus with placement of AXIOS lumen apposing stent. Images showing AXIOS stent apparatus in the region of the gastric fundus (arrowheads). Resolution of abscess with residual collapsed cavity (solid arrow). Bullet fragment adjacent to the T11 vertebral body (dashed arrow) on the coronal.
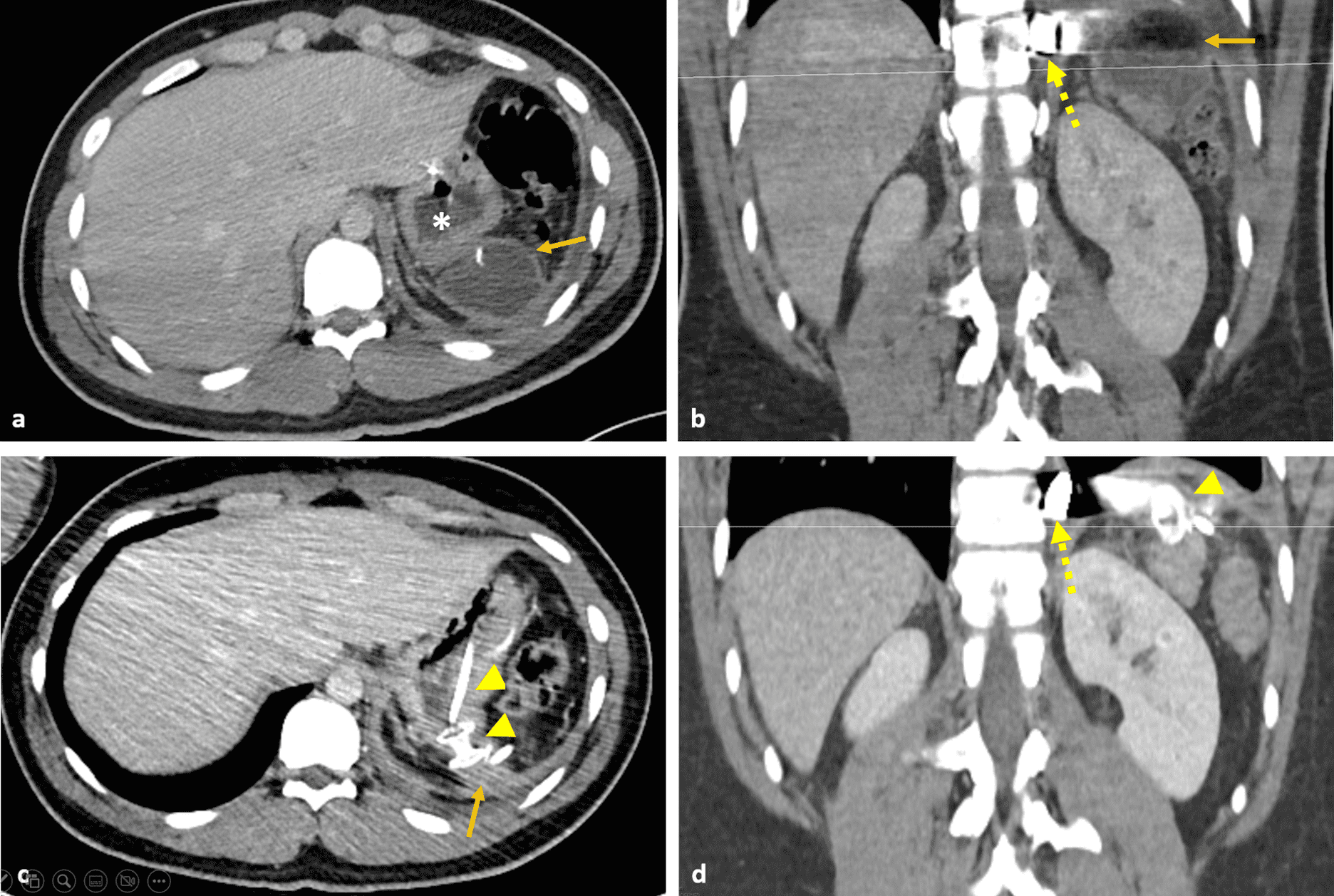
Figure: Figure.2 (A) Endoscopic ultrasound (EUS) image demonstrating a well-circumscribed, hypo-anechoic collection in the splenic bed consistent with an abscess. (B) Intraprocedural abscessogram performed during EUS-guided drainage. Contrast injection clearly delineates the abscess cavity without opacification of adjacent bowel loops, confirming appropriate localization and minimizing the risk of inadvertent deployment of the LAMS into surrounding structures. (C) Endoscopic images demonstrating EUS-guided drainage of a splenic bed abscess using a LAMS
Disclosures:
Nikita Garg indicated no relevant financial relationships.
Danial Nadeem indicated no relevant financial relationships.
Tushar Abhinav indicated no relevant financial relationships.
Mutshipay Christian Mpoy indicated no relevant financial relationships.
Kishore Kumar indicated no relevant financial relationships.
Nihaal Karnik indicated no relevant financial relationships.
Nikita Garg, MD1, Danial Nadeem, MD1, Tushar Abhinav, MD2, Mutshipay Christian Mpoy, MD3, Kishore Kumar, MD4, Nihaal Karnik, MD1. P3582 - Endoscopic Ultrasound-Guided Luminal Apposing Metal Stent Drainage of a Post-Splenectomy Abscess: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2The Wright Center for Graduate Medical Education, Wilkes-Barre, PA; 3Geisinger Health System, Wilkes-Barre, PA; 4Geisinger Community Medical Center, Scranton, PA
Introduction: Splenic abscess is a rare but potentially life-threatening condition. Endoscopic ultrasound (EUS)-guided drainage with lumen-apposing metal stents (LAMS) is an emerging minimally invasive approach for patients deemed poor surgical candidates, however, reported cases remain limited. We present a case of a post-splenectomy splenic bed abscess successfully managed with EUS-guided transmural drainage utilizing a LAMS and coaxial double-pigtail stent.
Case Description/
Methods: A 21-year-old male with recent gunshot injury to the left flank underwent exploratory laparotomy with splenectomy and diaphragm repair. Two weeks postoperatively, he presented with fever and worsening abdominal pain. Imaging revealed a 4.1 x 5.8 cm rim-enhancing fluid collection in the splenectomy bed, consistent with an abscess in the post-splenectomy cavity. The collection was closely adjacent to the gastric fundus and diaphragm. Due to the high location of the abscess and lack of a safe percutaneous window, interventional radiology deemed image-guided drainage unfeasible. Given the anatomic proximity of the collection to the stomach, EUS was performed. A well-defined hypoechoic abscess was identified adjacent to the gastric fundus. Following doppler evaluation to exclude intervening vasculature, a 10 mm × 10 mm LAMS (AXIOS, Boston Scientific) was deployed under EUS and fluoroscopic guidance using direct puncture with pure cutting current. Immediate purulent drainage confirmed successful cavity access. An abscessogram demonstrated proper positioning and contrast flow. A 10 Fr × 3 cm double-pigtail plastic stent was placed coaxially through the LAMS to prevent stent occlusion and migration. The procedure was well tolerated with no complications. Follow up CT at 6 weeks demonstrated complete resolution of the abscess with the LAMS still in place. The stent was safely removed one week later.
Discussion: Although EUS-guided drainage is well established for pancreatic fluid collections, its application in non-pancreatic abscesses—particularly splenic bed collections—remains rare. This case highlights the feasibility and safety of EUS-guided transmural drainage using a LAMS in a post-splenectomy patient, where percutaneous access was not possible. Internal drainage via EUS offered a minimally invasive alternative to surgery, with successful infection resolution and no procedural complications. This approach may expand the therapeutic arsenal for managing deep-seated intra-abdominal abscesses in high-risk surgical patients.
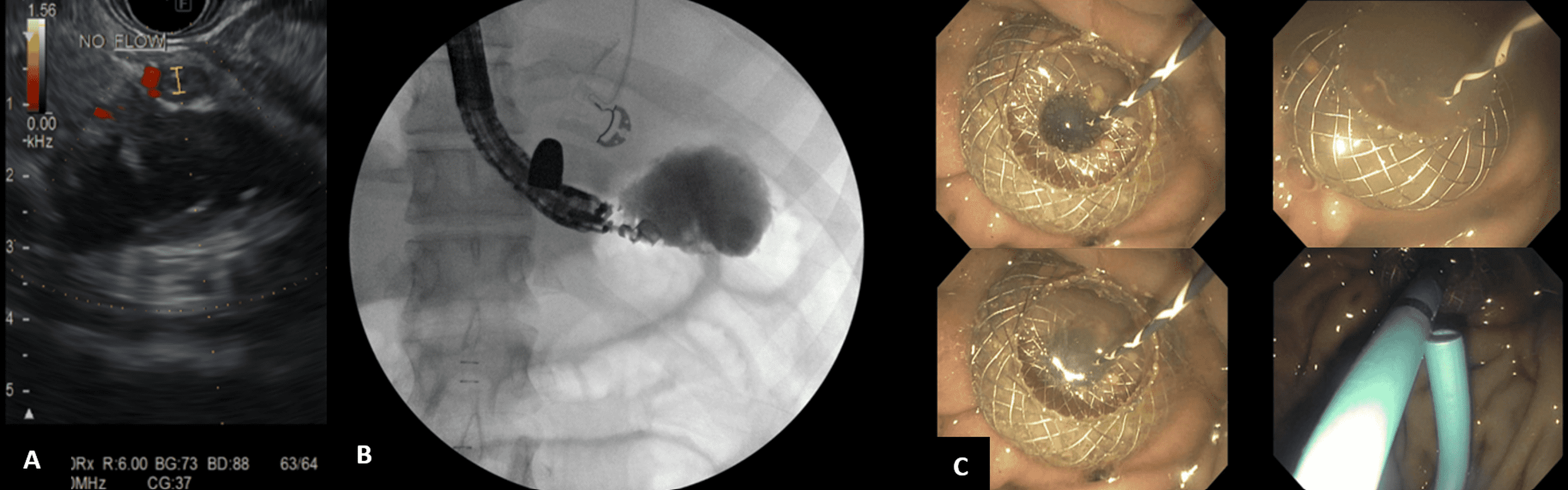
Figure: Figure.1 Axial (a) and coronal (b) contrast enhanced CT through the abdomen on 3/22/2025 demonstrating a 4 x 6 cm abscess (arrow) within the splenectomy bed (solid arrow) abutting the stomach (*) posteriorly. Bullet fragment (dashed arrow) to the left of the T11 vertebral body on the coronal. Contrast enhanced axial (c) and coronal (d) CT through the abdomen on 5/23/2025 status post upper endoscopic ultrasound (EUS) guided transmural drainage via the gastric fundus with placement of AXIOS lumen apposing stent. Images showing AXIOS stent apparatus in the region of the gastric fundus (arrowheads). Resolution of abscess with residual collapsed cavity (solid arrow). Bullet fragment adjacent to the T11 vertebral body (dashed arrow) on the coronal.
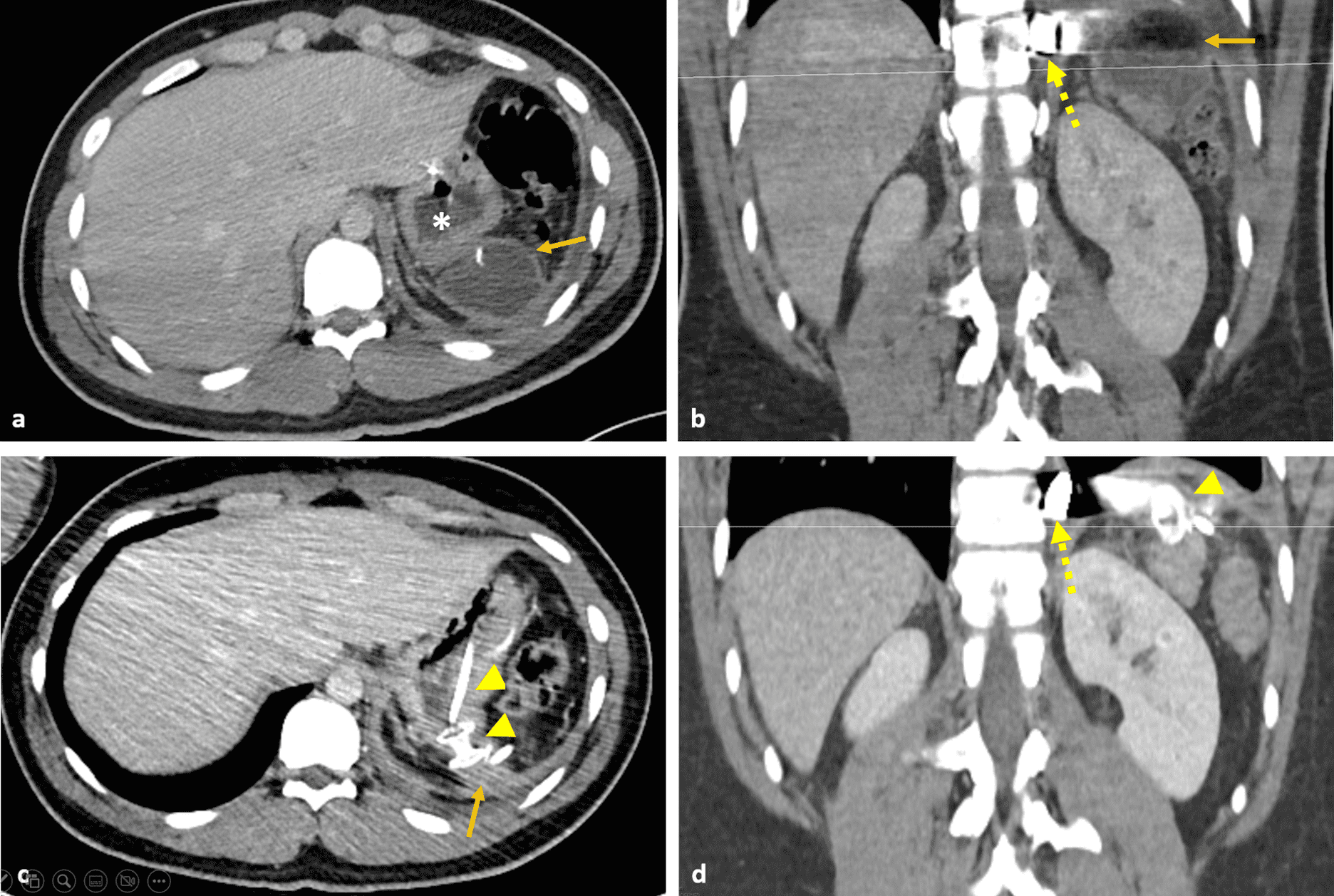
Figure: Figure.2 (A) Endoscopic ultrasound (EUS) image demonstrating a well-circumscribed, hypo-anechoic collection in the splenic bed consistent with an abscess. (B) Intraprocedural abscessogram performed during EUS-guided drainage. Contrast injection clearly delineates the abscess cavity without opacification of adjacent bowel loops, confirming appropriate localization and minimizing the risk of inadvertent deployment of the LAMS into surrounding structures. (C) Endoscopic images demonstrating EUS-guided drainage of a splenic bed abscess using a LAMS
Disclosures:
Nikita Garg indicated no relevant financial relationships.
Danial Nadeem indicated no relevant financial relationships.
Tushar Abhinav indicated no relevant financial relationships.
Mutshipay Christian Mpoy indicated no relevant financial relationships.
Kishore Kumar indicated no relevant financial relationships.
Nihaal Karnik indicated no relevant financial relationships.
Nikita Garg, MD1, Danial Nadeem, MD1, Tushar Abhinav, MD2, Mutshipay Christian Mpoy, MD3, Kishore Kumar, MD4, Nihaal Karnik, MD1. P3582 - Endoscopic Ultrasound-Guided Luminal Apposing Metal Stent Drainage of a Post-Splenectomy Abscess: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
