Monday Poster Session
Category: Interventional Endoscopy
P3574 - Roux-en-Y Gone Awry: Endosuture Closure of a Large Anastomotic Perforation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MC
Mark Cromer, MD
Prisma Health Greenville Memorial Hospital
Greenville, SC
Presenting Author(s)
Mark Cromer, MD, Kalpit Devani, MD
Prisma Health Greenville Memorial Hospital, Greenville, SC
Introduction: Anastomotic leaks occur in 0.1 – 5.6% of cases following Roux-en-Y gastric bypass (RYGB) surgery; they are associated with significant risk of morbidity and mortality and remain challenging to treat. Endoscopic interventions are safe, effective methods for closure of gastrointestinal (GI) perforations with lower procedural risks than surgery. This case demonstrates the utility of endosuture for non-surgical management of a complex anastomotic perforation.
Case Description/
Methods: A 68-year-old male with history of multiple abdominal surgeries underwent RYGB for refractory class 3 obesity with metabolic syndrome. The procedure was technically difficult and prolonged due to dense adhesions but without immediate complication.
On post-operative day (POD)-3, the patient presented with sudden onset severe diffuse abdominal pain. He was tachycardic and tachypneic with otherwise normal vitals. His abdomen was soft, non-distended, tender to palpation over epigastrium but without peritoneal signs. Lab work revealed an anion gap metabolic acidosis (20 mmol/L) but normal lactic acid and white blood cell count. A computed tomography (CT) scan showed oral contrast leakage into a 10.5 x 7.2cm gas-containing fluid collection between the gastric pouch and remnant stomach. The patient underwent emergent exploratory laparotomy (ex-lap) with evacuation of a turbid peri-anastomotic fluid collection, but no obvious defect was identified. On POD-1 after ex-lap, imaging showed persistent oral contrast leakage near the anastomosis. On POD-7, esophagogastroduodenoscopy (EGD) with thoracic surgery confirmed an anastomotic perforation. Despite attempted closure with endo-vacuum therapy (EVT), surveillance imaging showed a persistent anastomotic leak.
On POD-11, EGD with gastroenterology showed a large perforation (12 x 6cm) with exposed peritoneum. The perforation was successfully closed using 8 endoscopic sutures and 4 through the scope clips. Unfortunately, the patient’s critical illness led to progressive dehiscence that required multidisciplinary intervention and prolonged EVT. Surveillance EGD 2 months later revealed an 8mm contained defect; 2 plastic double-pigtail stents were placed to facilitate closure.
Discussion: Endosuturing has demonstrated >90% technical and clinical success in closure of large GI perforations. This case demonstrates that endosuturing was not limited by anatomic location or defect size and should be considered for primary closure and multidisciplinary intervention of complex GI perforations.
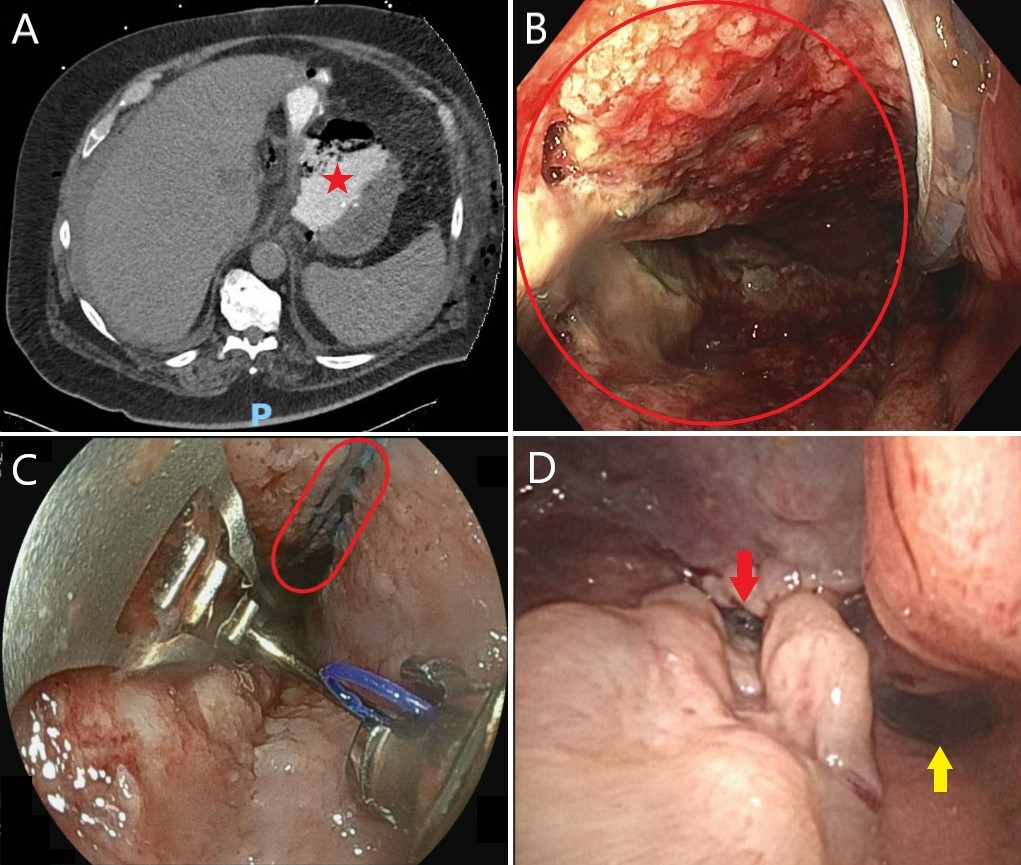
Figure: Figure 1: Case images
A) Axial view of computed tomography scan showing oral contrast leakage into a 10.5 x 7.2cm gas-containing fluid collection between the gastric pouch and remnant stomach (star).
B) Endoscopy image revealing a large (12cm x 6cm) anastomotic perforation with exposed peritoneum extending from the esophagogastric junction to the gastric pouch opening.
C) Endoscopy image of endoscopic suturing to close the anastomotic perforation. Eight endoscopic sutures were used, and the residual defect (circled) was successfully closed using 4 through-the-scope clips.
D) Surveillance endoscopy image 2 months after endosuture closure which revealed an 8mm residual contained defect (red arrow) adjacent to lumen (yellow arrow); two plastic double-pigtail stents were then placed to facilitate final closure.
Disclosures:
Mark Cromer indicated no relevant financial relationships.
Kalpit Devani indicated no relevant financial relationships.
Mark Cromer, MD, Kalpit Devani, MD. P3574 - Roux-en-Y Gone Awry: Endosuture Closure of a Large Anastomotic Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Prisma Health Greenville Memorial Hospital, Greenville, SC
Introduction: Anastomotic leaks occur in 0.1 – 5.6% of cases following Roux-en-Y gastric bypass (RYGB) surgery; they are associated with significant risk of morbidity and mortality and remain challenging to treat. Endoscopic interventions are safe, effective methods for closure of gastrointestinal (GI) perforations with lower procedural risks than surgery. This case demonstrates the utility of endosuture for non-surgical management of a complex anastomotic perforation.
Case Description/
Methods: A 68-year-old male with history of multiple abdominal surgeries underwent RYGB for refractory class 3 obesity with metabolic syndrome. The procedure was technically difficult and prolonged due to dense adhesions but without immediate complication.
On post-operative day (POD)-3, the patient presented with sudden onset severe diffuse abdominal pain. He was tachycardic and tachypneic with otherwise normal vitals. His abdomen was soft, non-distended, tender to palpation over epigastrium but without peritoneal signs. Lab work revealed an anion gap metabolic acidosis (20 mmol/L) but normal lactic acid and white blood cell count. A computed tomography (CT) scan showed oral contrast leakage into a 10.5 x 7.2cm gas-containing fluid collection between the gastric pouch and remnant stomach. The patient underwent emergent exploratory laparotomy (ex-lap) with evacuation of a turbid peri-anastomotic fluid collection, but no obvious defect was identified. On POD-1 after ex-lap, imaging showed persistent oral contrast leakage near the anastomosis. On POD-7, esophagogastroduodenoscopy (EGD) with thoracic surgery confirmed an anastomotic perforation. Despite attempted closure with endo-vacuum therapy (EVT), surveillance imaging showed a persistent anastomotic leak.
On POD-11, EGD with gastroenterology showed a large perforation (12 x 6cm) with exposed peritoneum. The perforation was successfully closed using 8 endoscopic sutures and 4 through the scope clips. Unfortunately, the patient’s critical illness led to progressive dehiscence that required multidisciplinary intervention and prolonged EVT. Surveillance EGD 2 months later revealed an 8mm contained defect; 2 plastic double-pigtail stents were placed to facilitate closure.
Discussion: Endosuturing has demonstrated >90% technical and clinical success in closure of large GI perforations. This case demonstrates that endosuturing was not limited by anatomic location or defect size and should be considered for primary closure and multidisciplinary intervention of complex GI perforations.
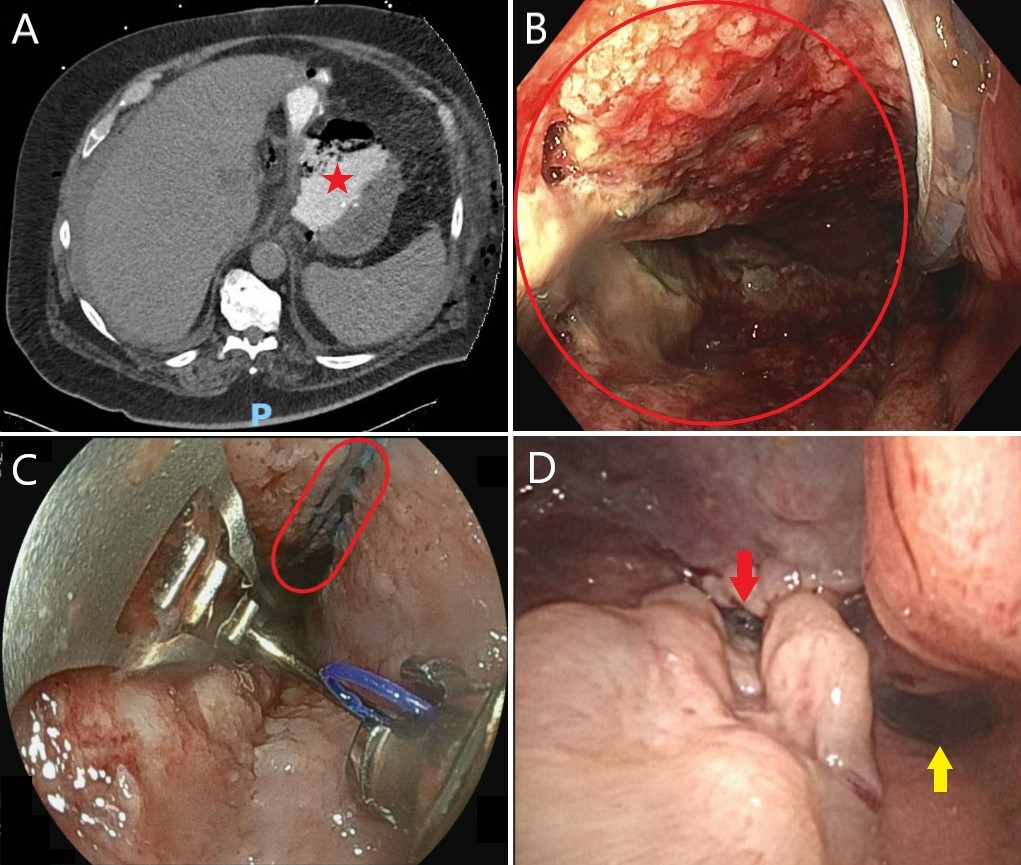
Figure: Figure 1: Case images
A) Axial view of computed tomography scan showing oral contrast leakage into a 10.5 x 7.2cm gas-containing fluid collection between the gastric pouch and remnant stomach (star).
B) Endoscopy image revealing a large (12cm x 6cm) anastomotic perforation with exposed peritoneum extending from the esophagogastric junction to the gastric pouch opening.
C) Endoscopy image of endoscopic suturing to close the anastomotic perforation. Eight endoscopic sutures were used, and the residual defect (circled) was successfully closed using 4 through-the-scope clips.
D) Surveillance endoscopy image 2 months after endosuture closure which revealed an 8mm residual contained defect (red arrow) adjacent to lumen (yellow arrow); two plastic double-pigtail stents were then placed to facilitate final closure.
Disclosures:
Mark Cromer indicated no relevant financial relationships.
Kalpit Devani indicated no relevant financial relationships.
Mark Cromer, MD, Kalpit Devani, MD. P3574 - Roux-en-Y Gone Awry: Endosuture Closure of a Large Anastomotic Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
