Monday Poster Session
Category: Interventional Endoscopy
P3572 - Endoscopic Treatment With Stenting, Cricopharyngeal Myotomy, and Vacuum-Assisted Closure of Iatrogenic Cervical Esophageal Perforation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- YH
Yassmin Hegazy, MD (she/her/hers)
University of Mississippi Medical Center
Jackson, MS
Presenting Author(s)
Award: ACG Presidential Poster Award
Yassmin Hegazy, MD, Shou-jiang Tang, MD, Parker Mullen, MD, Rachael Pace, MD, Jacob Moremen, MD
University of Mississippi Medical Center, Jackson, MS
Introduction: Patients with cervical esophageal perforations rarely require procedural intervention. Surgical management may include abscess drainage or primary repair in severe cases with stenting considered ineffective for perforation at or above the cricopharyngeus. This case demonstrates endoscopic treatment using stenting, cricopharyngeal myotomy, and Endoluminal Vacuum Assisted Closure (EVAC) to treat an iatrogenic case of cervical esophageal perforation.
Case Description/
Methods: A 76-year-old female with a history of hypertension and diabetes sustained an iatrogenic submucosal dissection from an endoscopic ultrasound (EUS). Computed Tomography (CT) imaging and esophagram showed a submucosal dissection extending from the cervical to the distal thoracic esophagus (Figure 2A). Repeat esophagram showed persistent contrast leak after 5 days of conservative management with intravenous antibiotics and nothing by mouth (NPO). Endoscopy revealed a perforation at the cricopharyngeus with a long tunnel (Figure 1A) not amenable to clip or suture closure. A prominent cricopharyngeal bar was present (Figure 1B) likely as an instigating factor and obstructing our instrumentation of the defect. Using standard tunneling technique, a full myotomy was performed giving greater access to the non-healing wound (Figure 1C). Mucopurulent fluid was lavaged out of the cavity, and an overtube was placed into the defect to facilitate EVAC placement. A granulofoam sponge was suture fixated to a Blake drain and pushed into the cavity then brought out through the nose and secured to the Vaccuum-Assisted Closure (VAC) cannister. She underwent two EVAC placements over 10 days until the wound was clean and sufficient granulation present (Figure 1D). A covered stent was placed just below the esophageal inlet to collapse the cavity and accelerate closure of the now clean defect. The stent was removed 39 days post-EUS, 2 weeks after placement, with healed perforation. Repeat esophagram showed no esophageal perforation or leak (Figure 2B). The patient was seen in clinic one-month post-discharge with resolved dysphagia and tolerating oral intake.
Discussion: Cervical esophageal perforations that do not heal spontaneously are rare and often difficult to manage. Stenting alone is not an option and the narrowed lumen from the cricopharyngeus limits additional instrumentation. Our case demonstrates that endoscopic intervention with cricopharyngeal myotomy and EVAC can be successful in treatment of esophageal perforation at experienced centers.
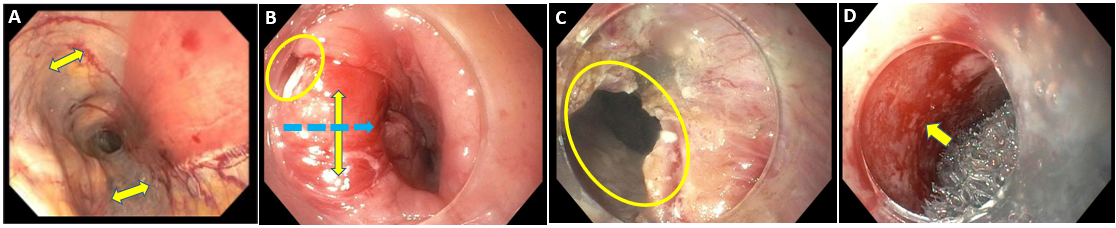
Figure: Figure 1A: EUS with submucosal dissection (arrows). Figure 1B: Cricopharyngeal bar (yellow arrow), perforation (circle), and myotomy pathway (blue arrow) Figure 1C: Defect following cricopharyngeal myotomy (circle). Figure 1D: Granulation tissue (arrow) following EVAC sponge
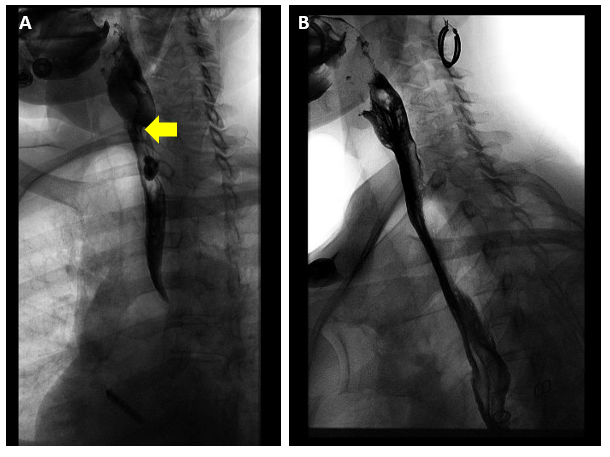
Figure: Figure 2A: Initial Barium Esophagram showing submucosal dissection and contrast leak. Figure 2B: Barium esophagram one month post-esophageal perforation with no contrast leak of perforation
Disclosures:
Yassmin Hegazy indicated no relevant financial relationships.
Shou-jiang Tang indicated no relevant financial relationships.
Parker Mullen indicated no relevant financial relationships.
Rachael Pace indicated no relevant financial relationships.
Jacob Moremen indicated no relevant financial relationships.
Yassmin Hegazy, MD, Shou-jiang Tang, MD, Parker Mullen, MD, Rachael Pace, MD, Jacob Moremen, MD. P3572 - Endoscopic Treatment With Stenting, Cricopharyngeal Myotomy, and Vacuum-Assisted Closure of Iatrogenic Cervical Esophageal Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Yassmin Hegazy, MD, Shou-jiang Tang, MD, Parker Mullen, MD, Rachael Pace, MD, Jacob Moremen, MD
University of Mississippi Medical Center, Jackson, MS
Introduction: Patients with cervical esophageal perforations rarely require procedural intervention. Surgical management may include abscess drainage or primary repair in severe cases with stenting considered ineffective for perforation at or above the cricopharyngeus. This case demonstrates endoscopic treatment using stenting, cricopharyngeal myotomy, and Endoluminal Vacuum Assisted Closure (EVAC) to treat an iatrogenic case of cervical esophageal perforation.
Case Description/
Methods: A 76-year-old female with a history of hypertension and diabetes sustained an iatrogenic submucosal dissection from an endoscopic ultrasound (EUS). Computed Tomography (CT) imaging and esophagram showed a submucosal dissection extending from the cervical to the distal thoracic esophagus (Figure 2A). Repeat esophagram showed persistent contrast leak after 5 days of conservative management with intravenous antibiotics and nothing by mouth (NPO). Endoscopy revealed a perforation at the cricopharyngeus with a long tunnel (Figure 1A) not amenable to clip or suture closure. A prominent cricopharyngeal bar was present (Figure 1B) likely as an instigating factor and obstructing our instrumentation of the defect. Using standard tunneling technique, a full myotomy was performed giving greater access to the non-healing wound (Figure 1C). Mucopurulent fluid was lavaged out of the cavity, and an overtube was placed into the defect to facilitate EVAC placement. A granulofoam sponge was suture fixated to a Blake drain and pushed into the cavity then brought out through the nose and secured to the Vaccuum-Assisted Closure (VAC) cannister. She underwent two EVAC placements over 10 days until the wound was clean and sufficient granulation present (Figure 1D). A covered stent was placed just below the esophageal inlet to collapse the cavity and accelerate closure of the now clean defect. The stent was removed 39 days post-EUS, 2 weeks after placement, with healed perforation. Repeat esophagram showed no esophageal perforation or leak (Figure 2B). The patient was seen in clinic one-month post-discharge with resolved dysphagia and tolerating oral intake.
Discussion: Cervical esophageal perforations that do not heal spontaneously are rare and often difficult to manage. Stenting alone is not an option and the narrowed lumen from the cricopharyngeus limits additional instrumentation. Our case demonstrates that endoscopic intervention with cricopharyngeal myotomy and EVAC can be successful in treatment of esophageal perforation at experienced centers.
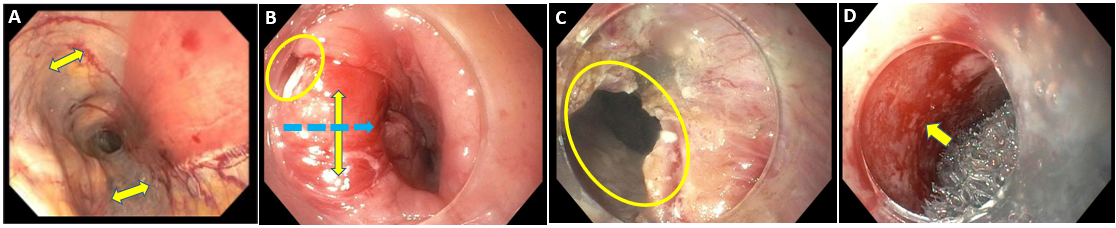
Figure: Figure 1A: EUS with submucosal dissection (arrows). Figure 1B: Cricopharyngeal bar (yellow arrow), perforation (circle), and myotomy pathway (blue arrow) Figure 1C: Defect following cricopharyngeal myotomy (circle). Figure 1D: Granulation tissue (arrow) following EVAC sponge
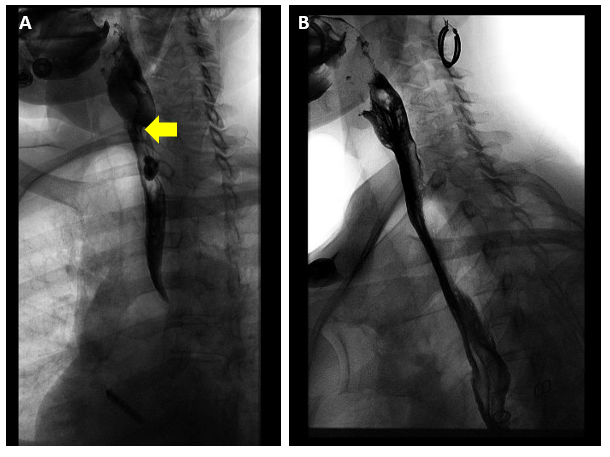
Figure: Figure 2A: Initial Barium Esophagram showing submucosal dissection and contrast leak. Figure 2B: Barium esophagram one month post-esophageal perforation with no contrast leak of perforation
Disclosures:
Yassmin Hegazy indicated no relevant financial relationships.
Shou-jiang Tang indicated no relevant financial relationships.
Parker Mullen indicated no relevant financial relationships.
Rachael Pace indicated no relevant financial relationships.
Jacob Moremen indicated no relevant financial relationships.
Yassmin Hegazy, MD, Shou-jiang Tang, MD, Parker Mullen, MD, Rachael Pace, MD, Jacob Moremen, MD. P3572 - Endoscopic Treatment With Stenting, Cricopharyngeal Myotomy, and Vacuum-Assisted Closure of Iatrogenic Cervical Esophageal Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

